Introduction
Patella dislocations and resultant recurrent instability commonly occurs, especially in adolescent individuals. The medial patellofemoral ligament (MPFL) is the major medial restraint of the patella and prevents lateral dislocation (Buckens and Saris 2010). The MPFL is commonly disrupted when the patella dislocates laterally. The MPFL attaches on the medial side of the patella as well as the femur near the medial epicondyle (Kyung and Kim 2015). When the MPFL is torn, the literature indicates that the risk of recurrence of patella dislocation is substantial (Gurusamy, Pedowitz, Carroll, et al. 2021; Kyung and Kim 2015). Typically, these injuries occur in younger individuals with the highest incidence in adolescents and young adults. Recurrent instability and dislocation of the patella can result in additional injury to the soft tissue as well as osteochondral damage to the patella and femur (Ambra et al. 2021; Buckens and Saris 2010; Hayat, El Bitar, and Case 2022; Migliorini et al. 2022).
Previous studies have demonstrated that simply repairing the MPFL may be inadequate to restore the strength of the native MPFL and prevent recurrent patella instability (Ambra et al. 2021; Mountney et al. 2005). Operative intervention for patella dislocation is indicated in patients who have had multiple patella dislocation or those with a significant osteochondral injury of the patella and or femur after the initial dislocation (Buckens and Saris 2010; Gurusamy, Pedowitz, Carroll, et al. 2021) Techniques have been developed to reconstruct the MPFL. These techniques in essence are used to increase the strength of the MPFL to prevent recurrent dislocation. One of the most common surgical techniques is the two-socket technique in the patella. Two 4.5 mm x 25 mm sockets are made in the upper 2/3 of the medial aspect of the patella and the ends of the graft/tendons are prepared and docked in the tunnels and secured using eyelet interference screws. Subsequently the double over end is inserted and secured in a tunnel at the MPFL attachment in the femur (Gould et al. 2021; Rosinski et al. 2019; Schöttle et al. 2009). Most of these techniques use two incisions near the medial edge of the patella and one by the lateral femoral condyle. The senior author felt that a single incision technique had several advantages including complete visualization of the graft, easy insertion under the fascia, prevent twisting of the graft as it is passed under the fascia and to help prevent over tensioning by easily placing a hemostat underneath the graft as it is inserted and fixed in the femur.
There are multiple grafts and materials that can be utilized for these techniques; the Semitendinosus allograft tendon is the most commonly used (Saper et al. 2017; Sequeira, Imbergamo, and Gould 2022). Several studies have demonstrated the ultimate load to failure of this technique using the Semitendinosus tendon. Technique and graft choice together have been shown to be equal to or several times stiffer than the native MPFL (Joyner et al. 2017; Mountney et al. 2005; Russ et al. 2015; Sequeira, Imbergamo, and Gould 2022). Several other studies have shown good outcomes using bioactive synthetic ligaments (Berruto et al. 2017) or high-tensile strength suture tape (Ishibashi et al. 2020; Mehl et al. 2020; Tsushima et al. 2019; Xu et al. 2021) to augment the MPFL in place of the Semitendinosus tendon. The goal of these techniques described in this paper is not to reconstruct or replace the MPFL but to augment and reinforce the existing repaired ligament (Mountney et al. 2005; Migliorini et al. 2022).
Biologic grafting and augmentation have been a focus within orthopedics over the last decade. Newer biologic augments have shown an ability to provide strength and bio-induction of native tissue. The focus of these augments has typically been seen in rotator cuffs repairs and anterior cruciate ligaments reconstruction (Uchida et al. 2020)
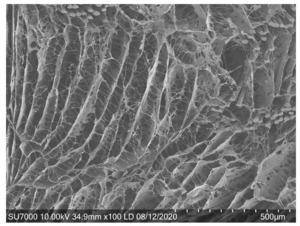
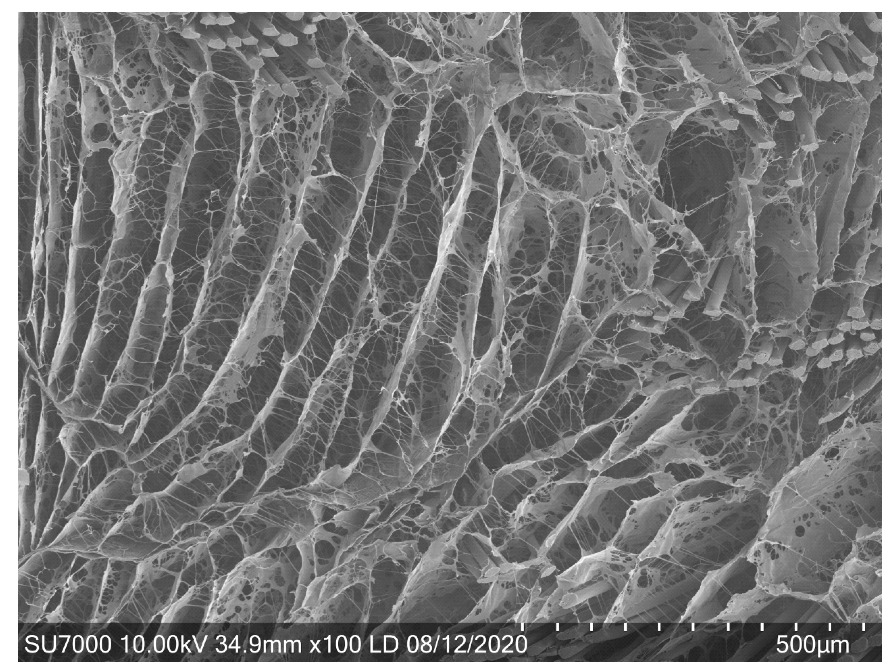
A reinforced bio-inductive implant (RBI) (BioBrace® CONMED, New Haven, CT) was developed to achieve biologic and mechanical augmentation. It is a bio-composite implant made of highly porous collagen sponge for improving healing reinforced with PLLA microfilaments for strength. (Figure 1) It has significant tensile strength that enables load sharing to reinforce the soft tissue repair throughout the healing process. Furthermore, in a large animal model, it has been demonstrated to provide supplemental strength and bio-inductive activity to the native tissue (Carter et al. 2021; Walsh et al. 2021).
The RBI 5x250 mm implant is used to augment the MPFL in the same fashion as the Semitendinosus allograft tendon or other synthetic grafts or suture tape. Recent studies have shown the RBI has similar mechanical strength to the semitendinosus tendon using the patella double socket technique as described above (Wetzler et al. 2024). The purpose of this study is to not only demonstrate a single incision technique to augment the MPFL but also introduce the use of an RBI as the graft for this technique. Each one has its own advantages and together significantly improves augmentation of the MPFL.
Operative Technique.
After a diagnostic arthroscopy of the knee to evaluate and treat any articular cartilage for injuries, the limb is exsanguinated with an Esmarch, and a tourniquet is inflated. The medial patella and medial epicondyle of the femur are palpated, and a 5 cm incision is made midway between these landmarks. The incision may be increased depending on the size of the patient. The medial patella is brought into the wound. The assistant, using their thumb, applies pressure to the lateral border of the patella. After dissecting the subcutaneous tissue, the medial retinaculum and MPFL are located, and an incision is made in the ligament about 1 cm off the patella.
The medial side of the patella is exposed and a burr or rongeur are used to expose the bone. The superior medial aspect of the patella at the point where the patella courses laterally and superiorly is located and is marked. Another point on the patella is marked at a minimum of 1.5 cm distal to the superior corner of the patella. (Figure 3A) The distance can vary depending on the overall size of the patella. Using the superior point as a guide will help place the sockets in the upper 2/3 of the patella. A guide pin is drilled to a depth of 25 mm at the selected points. The surgeon should direct the guide pin perpendicular to the long axis of the patella and parallel to the anterior surface of the patella. The guide pin should be easily drilled to the depth of 25 mm. If the pins meet significant resistance when drilling, the pin could be in subchondral bone which may reduce the strength of fixation of the anchor, and it is suggested that the pin be removed and redrilled. (Figure 3B) The guide pins are over-drilled with a 4.5 mm cannulated drill and a 25 mm socket is created. (Figure 3C)
The RBI is prepared. The implant is shortened to 210 to 220 mm for most knees. It can be shortened further depending on the knee but do not recommend shorter than 200 mm to assure proper fixation in the femoral tunnel. (Figure 4A) A whip stitch is done for 25 mm at each end of the implant. The whip stitch tapers the ends to facilitate insertion into the patella. (Figure 4B)
The implant is doubled over a number #5 braided nonabsorbable suture. A mark is made at 25 mm and 40 mm from the apex of the doubled-over end to assist in visualization during docking into the femoral tunnel. (Figure 5A & B)
Each end of the RBI is docked into the tunnels using a 4.75 screw/eyelet anchor. It is recommended to thoroughly debride each socket. There is usually minimal difficulty docking the implants in the sockets but if there is, it is recommended to over-drill just the opening of the socket with a 5 mm reamer by hand.
A bump is put under the knee and the knee is flexed to approximately 30 degrees. Using the standard technique and radiographic imaging, a 2.4 guide pin is placed in the insertion of the MPFL on the femur between the adductor tubercle and medial epicondyle.
A 7 mm reamer is used to make a 40 to 45 mm socket. It is recommended to drill the femoral tunnel 5-10 mm longer than the estimated length of the RBI in the femoral tunnel. (Figure 7) The marks at 25 mm and 40 mm from the apex of the folded RBI will help the surgeon estimate the amount in the tunnel.
A hemostat is placed from the superficial fascia and grabs the #5 suture, and the implant is passed under the superficial fascia. Care is taken when passing the implant underneath the fascia so that it does not twist. The #5 suture is placed in the eyelet of the 2.4 mm guide pin and passed through the femur. With the knee flexed approximately 30 degrees and the patella centered in the trochlear groove, the implant is inserted into the femoral tunnel. A Kelly or hemostat clamp is placed underneath both limbs just anterior to the femoral tunnel to prevent over-tightening. A 6x23 mm bio-composite interference screw is then placed in the femoral tunnel over a nitinol wire. (Figure 8). In larger patients, the incision can be extended slightly, and care is taken to dissect the soft tissue to be able to create a mobile window allowing adequate exposure of the medial border of the patella and medial epicondyle.
The stability and mobility of the patella are tested. The MPFL is repaired in a Pants over Vest fashion using the sutures from the screw/eyelet anchor and the posterior portion is approximated to the patella with the patella portion over sewn on top. (Figure 9) The incision is then closed in the usual fashion and the patient is placed in a range of motion brace locked in extension.
In patients without repaired osteoarticular injuries, full weight bearing in the range of motion brace is allowed immediately. Due to the fixation strength and biomechanical properties of the RBI (Wetzler et al. 2024) the senior author has adopted an aggressive rehabilitation protocol. Rehabilitation begins at one week with full flexion usually achieved by six weeks postoperatively. At 3 months, the patients can do increased sports or job-specific activities and may return to sports or work as early as 5 months.
Discussion
This study demonstrates not only a single incision technique to augment the MPFL but also introduces the use of an RBI implant as the graft for this technique. Each one has its own advantages and together significantly improves the augmentation of the repaired MPFL.
There are various techniques have been described for reconstructing the MPFL and multiple different types of implants have been used including biologic (allografts and autografts) and nonbiologic grafts (Synthetic ligament and high tensile strength suture tape) for augmentation of an MPFL repair (He et al. 2013; Mehl et al. 2020; Tsushima et al. 2019; Xu et al. 2021; Wang et al. 2017).
There are multiple articles that describe two-incision techniques with good results (Rosinski et al. 2019; Zanon, Marullo, and Benazzo 2013). The only advantage of the two-incision versus a single incision is the length of the incision. The single-incision technique is very cosmetic, and the total length of the incision is about the same length as the sum of the lengths of the incision in the two-incision technique. The femoral insertion of the MPFL can be easily located by direct visualization and palpation. The single incision allows the surgeon to carefully monitor the passage of the graft under the fascia. The senior author has found that the graft may twist itself which may be difficult to see in the two-incision technique but can be easily seen in the single-incision technique. Another advantage of this technique is that the surgeon can easily ensure the docking of the graft into the femoral tunnel. Furthermore, appropriate tensioning of the graft is simplified by placing a hemostat underneath the graft just above the femoral tunnel (Figure 8) which helps prevent over-tensioning of the graft and capturing of the patella a known complication of MPFL reconstruction techniques (Dornacher et al. 2018).
There are also several advantages of using this RBI implant. It is off the shelf, and it does not require any special storage or refrigerator. The RBI implant is consistent in size and shape and easily docked into a 4.5 mm socket. A Semitendinosus tendon almost always has to be trimmed, and it can be difficult to secure it into the 4.5 mm sockets in the patella. When using the Semitendinosus tendon, there is difficulty inserting into the socket due to bunching of the whipstitched end thus the socket may need to be enlarged to 5.0 mm and the fixation graft into the patella may need to be reinforced in some cases. In addition, the RBI implant has comparable pullout strength to the semitendinosus tendon when using this technique for docking it into the patella (Wetzler et al. 2024).
Over time, as cells infiltrate the implant, tissue matures, and with new tissue ingrowth in and round the RBI implants, it increases the implant strength. The RBI implant provides supplemental strength for 2 years during the healing process before it is fully reabsorbing (Carter et al. 2021). There is minimal risk of an adverse immune response which may happen with an allograft (Hinsenkamp et al. 2012).
Due to the fixation strength and biomechanical properties of the RBI (Wetzler et al. 2024) the senior author has adopted an aggressive rehabilitation protocol. Rehabilitation begins at one week with full flexion usually achieved by six weeks postoperatively. At 3 months, the patients can increase sports or job-specific activities and may return to sports or work as early as 5 months. Every patient is unique, and their recovery may vary depending on whether they had any osteoarticular injuries or when they achieve good quadriceps strength and full range of motion. Preliminary results have been reported in seven patients (Wetzler et al., n.d.). There have been no recurrent dislocations, no graft related complications and all patients returned to full activity by 6 months.
Currently, further retrospective and prospective studies are being carried out comparing the RBI in other techniques and comparing it to different grafts. Also, additional biomechanical testing studies are being done on this RBI to determine the ultimate strength and elasticity when used in this and other techniques to augment torn ligaments and tendons.

_the_medial_incision_is_made._the_surgical_assistant_put_pressure_on_the_lateral_edge_o.png)
_the_medial_side_of_the_patella_is_exposed_and_using_a_burr_or_ronguer_to_expose_the_bo.png)
_the_bio-inductive_scaffolding_is_shortened_to_220_mm_(b)_a_whipstitched_is_placed_on_e.png)
_the_rbi_implant_is_folded_over_with_a__5_suture_at_the_apex._(b)_the_implant_is_marked.png)
_(b)_the_implant_attached_to_and_docked_into_the_socket_using_4.75_screw_eyelet_anchor._(c.png)



_the_medial_incision_is_made._the_surgical_assistant_put_pressure_on_the_lateral_edge_o.png)
_the_medial_side_of_the_patella_is_exposed_and_using_a_burr_or_ronguer_to_expose_the_bo.png)
_the_bio-inductive_scaffolding_is_shortened_to_220_mm_(b)_a_whipstitched_is_placed_on_e.png)
_the_rbi_implant_is_folded_over_with_a__5_suture_at_the_apex._(b)_the_implant_is_marked.png)
_(b)_the_implant_attached_to_and_docked_into_the_socket_using_4.75_screw_eyelet_anchor._(c.png)


