INTRODUCTION
The Latarjet procedure was initially described by Michel Latarjet in 1954 as a novel treatment for recurrent dislocations of the shoulder (Latarjet 1954). The procedure involves transfer of the coracoid, along with the conjoined tendon, to the anteroinferior surface of the glenoid. It is hypothesized to improve anterior shoulder instability by increasing the bony surface area of the shoulder joint, supplementation of the capsuloligamentous complex with the coracohumeral ligament, and via a “sling-effect” with the conjoined tendon provided an additional anterior restraint to subluxation when in an abducted and externally rotated position (Yamamoto, Muraki, An, et al. 2013). Although initially described as a treatment for recurrent instability, the Latarjet procedure is frequently used in both primary and revision settings, demonstrating a significant reduction in instability events (Allain, Goutallier, and Glorion 1998; Yapp, Nicholson, McCallum, et al. 2020; Werthel, Sabatier, Schoch, et al. 2020). Common indications include young, contact athletes with a high risk of recurrence and patients with glenoid bone loss (Allain, Goutallier, and Glorion 1998; Domos, Lunini, and Walch 2018; Giles, Boons, Elkinson, et al. 2013; Hurley, Schwartz, Mojica, et al. 2021; Gilat, Lavoie-Gagne, Haunschild, et al. 2020; Arner et al. 2020).
Numerous techniques have been described since the procedure’s inception, with the arthroscopic Latarjet emerging over the last decade as the natural evolution of the classic open Latarjet procedure (Burkhart, De Beer, Barth, et al. 2007; Young et al. 2011; Getz and Joyce 2020; Wong, Friedman, and Garrigues 2020; du Plessis, Dachs, Vrettos, et al. 2018; Lafosse and Boyle 2010; Sharareh et al. 2021; Bhatia, Frank, Ghodadra, et al. 2014). This arthroscopic approach allows for many advantages of the open Latarjet procedure with the additional advantages of minimally invasive techniques (John and Wong 2019). While this technically demanding procedure comes with its own challenges and complications, recent modifications have been made to mitigate these new concerns (Tibone 2016; Moga, Konstantinidis, Coady, et al. 2018; Imai 2021; Ranne and Kainonen 2021).
The large volume of research being published can create difficulty in finding the most influential articles on a given topic. A bibliometric or citation analysis can be used to determine the impact a publication has on a specific topic or field (Cheek, Garnham, and Quan 2006; Garfield 1972; Lefaivre, Shadgan, and O’Brien 2011). In recent years, bibliometric analyses have been published for all shoulder surgeries, shoulder instability, arthroscopy, and Bankart lesions, though not with specific focus on the Latarjet procedure or bone-augmentation in shoulder instability (Namdari, Baldwin, Kovatch, et al. 2012; Bondar, Damodar, Schiller, et al. 2021; Allahabadi, Eftekhari, Feeley, et al. 2021; Moore et al. 2021). However, Allahabadi et al. in their study of Top 50 most-cited shoulder instability articles, found an increasing emphasis on bone-loss and Latarjet procedures during the last 10 years when compared to the cohort as a whole (Allahabadi, Eftekhari, Feeley, et al. 2021). This highlights the growing impact and utilization of the latarjet procedure in orthopedics and the need to best understand the existing research on the topic (Reider 2020; Kukkonen, Elamo, Flinkkilä, et al. 2021).
The purpose of our study was to identify the fifty most cited publications on the Latarjet procedure, as well as the articles’ associated characteristics. We hypothesized that year of publication would significantly impact the frequency an article was cited. The secondary purpose was to evaluate the evidence-level of the most influential articles. We anticipated that the majority of the most-cited articles would be of lower level evidence versus Level I or Level II studies. These findings can also highlight the recently-increased interest and controversies around this procedure and identify potential areas of focus for future research, particularly in respect to the types of studies needed.
METHODS
Institutional review board approval was not required because the data in the Clarivate Analytics Web of Science is publicly available. The Clarivate Analytics Web of Science was queried multiple times on December 12th, 2021 to perform this analysis. Numerous boolean combinations were entered into the database until a search-term provided the greatest number of returned articles. We attempted to include reference to relevant modifications on the Latarjet procedure, including by May in 1970 and Patte in 1980, in our search terms (May 1970). The final search-term used was “TOPIC: latarjet OR latarjet-bristow OR bristow-latarjet OR latarjet-patte or patte-latarjet”.
Articles returned by the final search-term were sorted based on the total citations per article. Titles and abstracts were reviewed and analyzed to exclude studies that were clearly unrelated to Latarjet. Articles needed to present information on indications, procedural descriptions, techniques, outcomes, or outcomes of Latarjet to be included. Articles that were systematic reviews or briefly mentioned Latarjet were excluded. These inclusion and exclusion criteria were similar to that utilized by other citation analyses (Barbera, Selverian, Courington, et al. 2020). If there was no agreement about whether an article should be included or excluded, the entire article was reviewed by a board-certified shoulder surgeon for the final determination.
Top fifty most-cited Latarjet articles were reviewed (XXX, XXX, and XXX) to collect each article’s author names, country of origin, publishing journal, type of article (e.g. biomechanical/cadaveric study, case-control study, cohort study, etc.) year of publication, number of citations, and the level of evidence according to The Journal of Bone and Joint Surgery’s published guidelines (Marx, Wilson, and Swiontkowski 2015). Citation density was calculated for each article as the total number of citations divided by years since publication according to Moore et al (Moore et al. 2021). The level of evidence and type of article were independently determined by (XXX, XXX). If a consensus on classification could not be reached, then a third author (XXX) made the final determination.
RESULTS
The final search-term used on the Clarivate Analytics Web of Science returned 921 results. The first 921 articles were reviewed to identify fifty articles that were the most-cited articles relating to Latarjet (Table 1).
There were a total of 5,319 citations (106 citations per article) among the top 50 most-cited Latarjet articles (Table 1). Allain et al., published in 1998, had the most citations with 454 total citations and an average of 19 citations per year. The article with the least number of citations was published in 2011 by Dolan et al. and has been cited 44 times (4 citations per year). The article with the most citations did not have the highest citation density. Rather, Burkhart et al., published in 2007, had the highest citation density at 23 citations per year. Burkhart et al. also had the second most citations overall (349).
The earliest publication year of all the articles in our study was 1983 (Figure 1). Two of the top 50 articles were published in 1983, and another top-50 Latarjet article was not published until 1994. There were 8 top 50 Latarjet articles published in 2016, which is the most among all years represented in our study. Following 2016, there was 1 top-50 article published in 2017, and none since 2017. There was also a dip between 2014 and 2016, with only 2 top-50 articles published in 2015. The overall trend shows that the majority of top 50 most-cited Latarjet articles were published after the year 2000. The median year of publication was 2012.
The total number of citations among top 50 Latarjet papers has increased exponentially since 1983 (Figure 2), when the first high-impact Latarjet article was published. In 2021 alone, the top 50 Latarjet articles were cited a total of 599 times. The single year with the most citations was 2020 with 701 citations.
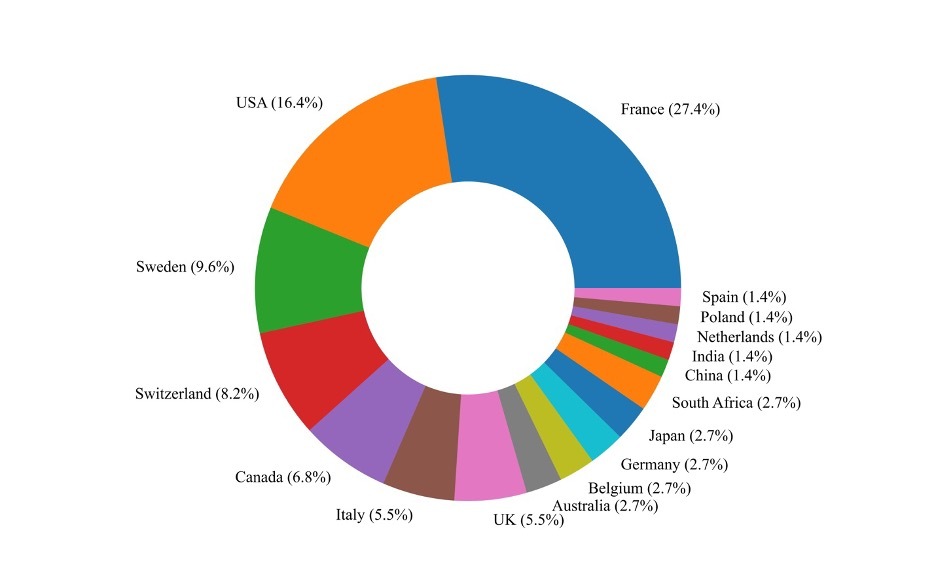
A total of 17 countries were represented by the authors of the articles in our study (Figure 3). France represented the highest number of author affiliations at 27% (n=14). The United States (n=8, 16%), Sweden (n=5, 10%), and Switzerland (n=4, 8%) followed France with the most author affiliations within our study. Five countries (Australia, Belgium, Germany, Japan, South Africa) were represented in 2 top-50 articles each, and five countries (China, India, Netherlands, Poland, Spain) were represented in a single top-50 article.
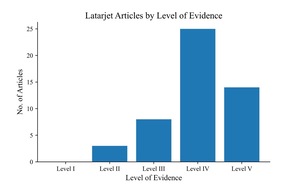
There was significant variation with respect to study type and level of evidence of the articles in our study. The most common study type was case series (24 articles). The least represented study type was prospective cohort studies, of which there were three (Table 2). Other study types included retrospective cohort studies (9), biomechanical/cadaveric studies (8), and expert opinions (6). There were no RCTs within the top 50 most-cited Latarjet articles. Level of evidence category IV was most common among the articles in our study (25 articles). There were no articles that fit the level of evidence category I. There were, however, 3 articles with level of evidence II, 9 with level III, and 14 with level V (Figure 4).
The articles in our study were published in various journals by many different authors. The top-50 articles were published in 13 different orthopedic journals (Table 3). Seventeen articles were published in the Journal of Shoulder and Elbow Surgery, which published the most top-50 articles. The other most-cited journals included Arthroscopy (7), The Journal of Bone and Joint Surgery American (6), the American Journal of Sports Medicine (5), and the Journal of Bone and Joint Surgery British (2), which is now The Bone & Joint Journal (Table 3). The author with the most first-author top 50 Latarjet publications was Hovelius, with 7 articles. Meanwhile, Boileau was the second most-published first author with 4 top 50 articles.
DISCUSSION
Our bibliometric analysis found that the top fifty most-cited articles on the Latarjet procedure were case series studies (24) and studies with Level IV evidence (25), a finding that has been observed in many bibliometric analyses in orthopedic surgery (Lefaivre, Shadgan, and O’Brien 2011; Moore et al. 2021; Barbera, Selverian, Courington, et al. 2020; Baldwin, Kovatch, Namdari, et al. 2012; Holzer and Holzer 2014). This finding suggests the need for a greater number of higher-level evidence studies on the Latarjet procedure, though this need is certainly not unique to the Latarjet procedure, as this trend and has been observed in other areas as well (Namdari, Baldwin, Kovatch, et al. 2012; Holzer and Holzer 2014). We also noted that there were no Level I studies amongst this body of literature that is highly influential to surgeons. While general guidelines exist on the optimal management of shoulder instability based on patient-specific factors, there are no consensus recommendations regarding which procedure surgeons should use and which technique is best (i.e. open versus arthroscopic). While this lack of consensus may be partly due to the rapid evolution and adoption of techniques (i.e. arthroscopic bone-block, etc), the lack of Level I evidence may be related to the lack of consensus. The findings of this article-review are important, and emphasize the need for higher-level studies on this topic.
We also observed that 12 studies (24%) were classified as cohort studies (prospective and retrospective), while in a similar study on most cited articles on rotator cuff surgery (Sochacki et al. 2018), only 5 articles (10%) were classified as cohort studies (prospective and retrospective). This may be due to interest in comparing the Latarjet procedure to other shoulder stabilization techniques such as the Bankart repair, particularly given that there no consensus on either procedure’s use as the gold standard treatment for recurrent anterior shoulder instability (Imam, Shehata, Martin, et al. 2021), in the primary or revision setting (Calvo, Luengo, Morcillo, et al. 2021). Retrospective and prospective cohort studies could have been used to uncover differences in outcomes between these procedures, thereby providing evidence for one procedure to be favored over the other for a given indication. Another finding was that the third most common study design among the top 50 most-cited Latarjet papers was biomechanical/cadaveric (8). This trend aligns with results of previous bibliometric analyses of shoulder instability (Allahabadi, Eftekhari, Feeley, et al. 2021), and reflects the ongoing efforts to fully understand the complex mechanics of shoulder instability.
We also noted that the majority (45) of top 50 most-cited papers were published after 2000, with a particularly high density (35) between 2010 and 2016 (Figure 1), a finding similarly-observed in bibliometric analyses on hip arthroscopy (Barbera, Selverian, Courington, et al. 2020) and shoulder arthroscopy (Moore et al. 2021), which both saw a prevalence of studies published in the late 2000s. This trend aligns with the growing interest in the arthroscopic Latarjet procedure, which is a much more recent (Lafosse, Lejeune, Bouchard, et al. 2007) development, relatively speaking (Wong, Friedman, and Garrigues 2020; van der Linde, van Wijngaarden, Somford, et al. 2016). In our citation analysis, 13 of the top 50 most-cited Latarjet articles specifically examined arthroscopic Latarjet, 12 of which were published after 2009. Therefore, the high density of top 50 most-cited Latarjet papers published between 2010 and 2016 may be partly due to the rapid development and expansion of arthroscopic technologies over the past two decades (Moore et al. 2021). Although technically demanding, the arthroscopic Latarjet may offer advantages including lower invasiveness for associated lesions (Lafosse and Boyle 2010; John and Wong 2019; Lafosse, Lejeune, Bouchard, et al. 2007; Castricini, De Benedetto, Orlando, et al. 2013).
The increasing interest in the arthroscopic latarjet likely affects not only the observed trend in publication date, as discussed above, but also likely influences the observed trend related to level of evidence.New treatments and ideas are usually presented through observational studies with lower level-of-evidence (Namdari, Baldwin, Kovatch, et al. 2012). As arthroscopic Latarjet is still in its relatively early stages, many of today’s most-cited articles may form the foundation that current and future higher level-of-evidence studies build upon in their research. In contrast to Moore et al’s prediction that RCTs will displace case series and expert opinion articles in future analyses of most-cited shoulder arthroscopy studies, future high-impact studies may include long-term case series that provide long-term data on the arthroscopic Latarjet (Moore et al. 2021). In regard to the traditionally open Latarjet, an older procedure than arthroscopic Latarjet, some randomized control trials may replace lower level-of-evidence studies currently in the top 50. This trend has been observed in citation analyses of older procedures such as hip and knee arthroplasty (Holzer and Holzer 2014; Piuzzi, Sultan, Gatta, et al. 2019), such as Kukkonen et al’s RCT on arthroscopic Bankart versus open Latarjet procedure in the treatment of traumatic shoulder instability in young males (Kukkonen, Elamo, Flinkkilä, et al. 2021).
There are many other factors that contribute to the citation frequency of a scientific article, including the originality of the findings, the rigor of the research methodology, its potential to change clinical practice, and its ability to influence new research inquiries. Additionally, numerous bibliometric analyses in both orthopedics and healthcare broadly have shown that the time amassed since an article’s publication contributes significantly to the number of citations it receives (Namdari, Baldwin, Kovatch, et al. 2012; Allahabadi, Eftekhari, Feeley, et al. 2021; Moore et al. 2021; Adams and Simonson 2004; Ahmad, Evangelopoulos, Abbasian, et al. 2014). as articles published earlier form a foundation for future articles to build and expand upon (Barbera, Selverian, Courington, et al. 2020). The present study’s findings also highlight the significant contributions of French surgeons to this area.
Authors of French origin contributed the highest number of studies to the top fifty most-cited articles on the Latarjet procedure. These results differ from other bibliometric analyses in orthopedic surgery and various other medical specialties where American authors have often produced the highest number of most-cited articles (Lefaivre, Shadgan, and O’Brien 2011; Namdari, Baldwin, Kovatch, et al. 2012; Moore et al. 2021; Barbera, Selverian, Courington, et al. 2020; Merigó and Núñez 2016; Loonen, Hage, and Kon 2008; Paladugu et al. 2002). The unique trend observed in this study likely reflects the pioneering contribution that French surgeons and researchers played in the development and use of the Latarjet procedure over the last half-century (Latarjet 1954). It may also reflect the preference of French surgeons for the Latarjet as a first-line surgical treatment modality for recurrent shoulder instability, given their successful outcomes (Imam, Shehata, Martin, et al. 2021; Thomazeau, Courage, Barth, et al. 2010). The successful track-record of the Latarjet by French surgeons likely continues to drive research and publication regarding this surgical technique. It is also unclear to what degree, if any, these results may be influenced by the large volume of orthopedic shoulder research produced in France and the United States, or biases in the publication process for French and American authors more broadly.
In addition to the length of time since publication and author country of origin, the publishing journal likely contributes to the overall number of citations an article obtains. Approximately one-third of the fifty most-cited articles were published in the Journal or Shoulder and Elbow Surgery, with Arthroscopy and Journal of Bone and Joint Surgery (American Volume) publishing the second and third most articles, respectively. This trend was not surprising considering these journals are well-established and popular, high-impact journals at the forefront of orthopedics and shoulder surgery.
As the arthroscopic Latarjet continues to evolve and expand over the coming years, the articles included in this analysis can serve as a starting point for understanding both the history and evolving landscape of the Latarjet procedure. This analysis of the most-cited articles on the Latarjet procedure can provide students, trainees and practicing orthopedic surgeons with a list of “should read” articles on this topic (Namdari, Baldwin, Kovatch, et al. 2012).
Limitations
Bibliometric and citation analyses have inherent limitations. The use of fifty articles as a cutoff in this study was arbitrary and may have led to other “influential” and “important” articles being omitted. However, this seems to be an established adequate number from which meaningful observations can be made (Namdari, Baldwin, Kovatch, et al. 2012; Bondar, Damodar, Schiller, et al. 2021; Allahabadi, Eftekhari, Feeley, et al. 2021; Moore et al. 2021). Second, related to the previous limitation, because this bibliometric analysis was based on an eponymous procedure, it inevitably excluded some early influential papers that did not yet refer to “Latarjet” as the name of this procedure. Though some prior descriptive manuscripts may have been excluded, we feel that our search captured the most influential articles for today’s readership. Another potential limitation, which has been recognized by other citation analyses, is that of a “snowball effect” that may have caused articles to have an artificially inflated number of citations (Lefaivre, Shadgan, and O’Brien 2011; Namdari, Baldwin, Kovatch, et al. 2012; Ahmad, Evangelopoulos, Abbasian, et al. 2014). This term describes a phenomenon by which authors are more likely to cite an article because it was previously cited, rather than citing it based on content or quality. While unavoidable, this phenomenon should be recognized by the reader, and emphasizes the need for personal and individual scrutiny of a publication prior to citing it oneself. Additionally, both citation density and total number of citations can be inflated by self-citations. For example, an author who regularly produces work on a specific topic is more likely to cite their past work and thereby increase their total number of citations, which is a consideration, but that would not affect the results presented here. Finally, there was some degree of inherent subjectivity in the inclusion and exclusion of each article in this study. To mitigate any bias or subjectivity in this regard, we incorporated various levels of review, across different levels of experience (e.g., medical students, residents, attending), when determining inclusion and exclusion.
CONCLUSION
The most-cited articles on the Latarjet procedure tend to be case series, cohort studies, and expert opinions published primarily by French and American authors between 2000 and 2016. With the recent technical innovation surrounding the Latarjet procedure and glenoid bone-block reconstruction in general, these articles may form the foundation that future higher level-of-evidence studies will build upon in their research. These findings highlight the need for higher level studies in this rapidly evolving field.