Background
Total knee arthroplasty (TKA) is a popular and successful treatment for end-stage knee arthritis. Despite vastly improved outcomes since pioneering knee replacement surgery last century, patient dissatisfaction rates are approximately 20% and only a small percentage of patients report no problems with their TKA. Currently, the optimal integration of knee anatomy, prosthesis biomechanics and implant design remain debated. Knowledge of the former two is integral to understanding the rationale behind different types of TKA designs and their impact on knee replacement biomechanics.
The Freeman Swanson TKA was the first ever condylar knee and was implanted in 1970 at Royal London Hospital, UK (figure 1) (Freeman, Swanson, and Todd 1973). The total condylar knee arthroplasty was introduced in 1974 and is arguably the first recognisable “modern-type” implant (Kristensen et al. 1992). Good outcomes were demonstrated after 5 to 10 years, with up to 95% survival rate after 15 years (Kristensen et al. 1992; Insall, Tria, and Scott 1979; Rinonapoli et al. 1992). From then on, many TKA designs have been developed and routinely used worldwide. Most protheses have either cruciate-retaining (CR) bearing surfaces or posterior-stabilized (PS) articulation (National Joint Registry for England and Wales 2020). CR designs tend to be either round-on-flat or flat-on-flat articulations. The drawbacks of the early CR designs included difficulties in range of motion and stair-climbing ability, and posterior tibial subluxation due to a paradoxical slide with flexion. To improve the posterior-stabilised prosthesis designs, a cam and post were added within the femoral and tibial polyethylene components respectively (Hossain et al. 2011; Insall, Lachiewicz, and Burstein 1982). The cam and post are designed to interact to guide the femur posteriorly with progressive knee flexion, inducing femoral rollback in an attempt to mimic the perceived action of the posterior cruciate ligament (PCL) (van Duren, Pandit, Beard, et al. 2007).
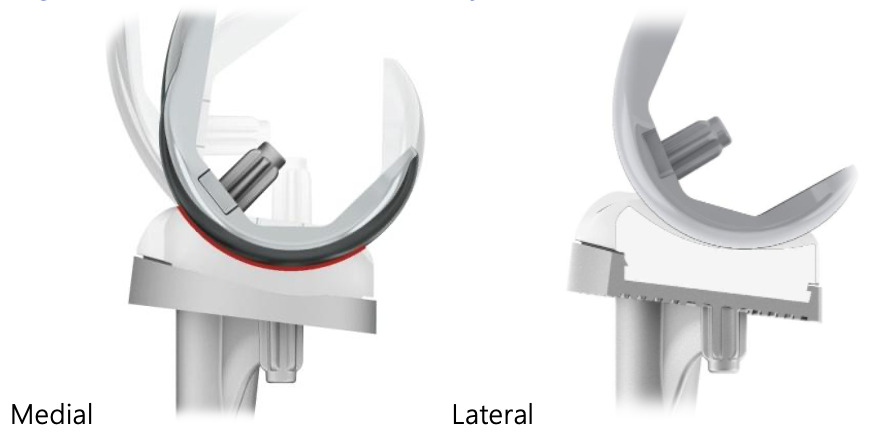
Understanding of native knee kinematics has improved over recent decades. With observations showing stability is primarily provided by the medial congruency of the natural knee, the MS-TKA (Medial-Stabilised-Total Knee Arthroplasty) concept was developed in the early 1990s (Nisar et al. 2022). The Medial-Stabilised (MS) design aims to reproduce the tibial–femoral kinematics observed in a healthy knee more closely. Typically, MS-TKA designs have an asymmetric liner and femoral component with a spherical single radius medial femoral condyle (Cassar-Gheiti et al. 2020). Ball and socket geometry of the medial compartment components has full congruency providing increased sagittal stability while laterally less congruent articulation permits the lateral condyle posterior roll and slide during flexion (figure 2). Thus for a MS-TKA to behave as a medial stabiliser, it should demonstrate full congruency medially from extension to beyond 90 degrees of knee flexion (thereby preventing a forced rollback until the end point in deep flexion) with the ability to translate more freely on the lateral side (Freeman and Pinskerova 2003). The term “medial pivot knee” can be misleading as it usually refers to the Advanced Medial Pivot (AMP) TKA (Microport Orthopedics Incorporated, Arlington, TN, USA). “Medial-Stabilised knee” is better terminology to explain the class of implant which fulfil these criteria.
The past decade has seen a significant increase in MS-TKA implanted globally with encouraging results. In this literature review, we summarise normal knee biomechanics and discuss the history and development of MS TKA. We also investigate the types of MS-TKA implants, revision rates, objective functional outcomes, patient-reported outcome measures (PROMs), and in-vivo kinematics.
Biomechanics of the natural knee
Some of the earliest studies of tibiofemoral movement suggested a medial-stabilised model of the knee. The earliest known description of a medial pivot model of the knee appears in Borelli’s posthumous publication in 1680 . In 1836, the Weber brothers hypothesised posterior translation of lateral femoral condyle in flexion with anteroposterior (AP) medial femoral condyle stability (Weber and Weber 1836; Pinskerova, Maquet, and Freeman 2000). They surmised this to suggest a longitudinal axis of rotation through the medial femoral condyle during flexion. The earliest stereophotogrammetry works provided further evidence for internal rotation about the medial femoral condyle on knee flexion (Pinskerova, Maquet, and Freeman 2000). Meanwhile, radiography work in 1904 by Zuppinger investigating native knee movement first described a rigid crossed-four-bar link model, whereby a tense pair of cruciate ligaments guide tibiofemoral movement causing posterior movement of both femoral condyles in relation to their articulation with the proximal tibia (Zuppinger 1904; O’Connor et al. 1989). The process is known as femoral “roll-back”. The Weber brother work was written in Old German and discounted rigid links because the anterior cruciate ligament (ACL) and PCL are not rigid, however it is believed that the diagrams alone were taken as an incorrect reference (Pinskerova, Maquet, and Freeman 2000). The model proposed by Zuppinger implies a helical axis of rotation describing the motion of the tibia, with centre of rotation at the intersection of the cruciate ligaments (O’Connor et al. 1989; Blaha et al., n.d.). This opinion prevailed for much of the 20th century and in part contributed to development of the J-curved CR and PS TKA concept (Freeman and Pinskerova 2005).
Subsequent extensive work around the turn of this century contradicts this theory. Freeman and Pinskerova produced a series of papers. They used cross-sectional imaging in weight-bearing and non-weight bearing living subjects, and anatomical studies in cadaveric knees (Freeman and Pinskerova 2003). They divided the flexion arc into three parts. The functional active arc covers approximately 20 to 120 degrees of flexion entirely under active muscle control and the medial condyle was stable in the AP plane. This appears caused by the constraint of the firmly adhered medial meniscus and fibres of the medial collateral ligament (MCL) combined with the ACL and PCL. In contrast, the lateral meniscus is more mobile, moving with the lateral femoral condyle in AP movement in a combination of rolling and sliding relative to the tibia. The overall result is the availability of voluntary internal/external rotation of the tibia vs. the femur during activities. This is about an axis parallel to the tibial long axis and centred on the medial femoral condyle centre of rotation. Indeed, magnetic resonance imaging at varying degrees of flexion in unloaded cadaveric knees demonstrated very little medial femoral condyle posterior translation, while the lateral femoral condyle moved by up to 19 mm (Iwaki, Pinskerova, and Freeman 2000). Subsequent fluoroscopic analysis of normal living knees in deep flexion demonstrated average lateral femoral condyle posterior translation of 12.7 mm, vs. 2.9 mm on the medial side (Komistek, Dennis, and Mahfouz 2003). These confirm the medially stabilised model of the native knee. This study emphasized that the condylar translation and movement of the contact point in the AP plane is dependent on the surface geometry.
Rationale and History of Medial-Stabilised TKA
PS and CR TKA designs minimise tibiofemoral conformity to prevent conflict with the physiological “rollback” described in the crossed four-bar linkage model (Blaha 2004). Fluoroscopic studies suggest neither PS nor CR TKA designs result in physiological knee kinematics. The cam-post design in PS TKA is largely ineffective in inducing the intended femoral rollback up to 60 degrees of knee flexion (van Duren, Pandit, Beard, et al. 2007) (partly dependent on cam position and activity type) and indeed paradoxical anterior sliding of the femoral component was noted in both PS and CR designs (Pandit et al. 2005; Dennis, Komistek, and Mahfouz 2003; Komistek and Dennis 2001). Blaha et al suggested a rationale for this (Blaha 2004). The knee is extended at the point of heel strike and the gait progresses to foot flat and maximum load. In a CR knee, the PCL is not tight until at least 45 degrees of flexion. Combined with minimal tibiofemoral congruence there is therefore little constraint to paradoxical anterior translation at the point of maximal load in normal gait. Similarly, the cam and post of PS implants are not fully engaged at the point of maximal load, which also may suggest the anterior translation observed in some studies (Blaha 2004; Komistek and Dennis 2001).
Failure of PS and CR designs to reproduce physiological knee kinematics may partly be because they are based on an outdated model of normal tibiofemoral motion. As discussed, various kinematic studies demonstrate a MS concept whereby the medial femoral condyle undergoes little or no femoral rollback (Hossain et al. 2011). The medially conforming “ball-and-socket” articulation was developed and purported to better reproduce native knee behaviour. The Freeman-Samuelson-1000 (FS-1000) knee was first implanted in November 1994 and later marketed as the Medial Rotation Knee (figure 3) (MRK, Finsbury Orthopaedics, Leatherhead, UK). This design was based on 1970s cadaveric studies conducted by the group and its clinical use pre-dates other MS-TKA designs. In this design, the medial femoral condyle is spherical and conformed with the concave medial tibial component, increasing sagittal plane stability. Meanwhile, the lateral side is less congruent and so posterior roll-back on the lateral tibia is permitted (Blaha 2002). Freeman’s group reported a registry study recording a ten year survival rate of 96% with aseptic loosening as the primary end point (Robertsson, Scott, and Freeman 2000). Currently, the following MS prostheses are used clinically: SAIPH (MatOrtho Ltd., Leatherhead, UK) developed from the MRK knee (figure 4), Evolution MP (MicroPort Orthopedics Inc., Arlington, TN, USA) replacing Advance Medial Pivot (AMP), and GMK Sphere (Medacta, Castel San Pietro, Switzerland) adding to the GMK knee platform. Importantly, differentiation between a true medially stabilised knee arthroplasty and medial congruent designs must be appreciated: the former are a true ball-in-socket design, while the latter rely on an ultra-congruent medial polyethylene insert for their stability and are outside the scope of this review.
Clinical Evidence for MS-TKA
AP Stability
MS-TKA provides more conformity medially and this is reflected in the AP stability these designs provide. Jones et al reported a matched-cohort cross-sectional study on 60 TKA patients at 1-year follow-up (Jones et al. 2020). Three surgeons performed 10 MS TKA and 10 non-MS TKA. Sagittal stability was assessed by a blinded observer using a KT-1000 arthrometer (Med Metrics Corp. Inc., San Diego, California, USA), Lachman’s test, and the anterior drawer test. PROMs utilised included: Oxford Knee Score, Knee Injury and Osteoarthritis Outcome Score, Western Ontario and McMaster Universities Osteoarthritis Index, Forgotten Joint Score, and visual analogue scale for functional and satisfaction assessments. MS-TKA demonstrated significantly decreased translation and improved stability vs. non-MS-TKA. Superior PROMs were demonstrated in the MS-TKA group compared with the non-MS-TKA group. When divided based on objective stability, regardless of prosthesis type, patients with a stable knee had superior PROMs, particularly in sports-related questions. The authors concluded that MS-TKA provided significantly greater sagittal stability, and improved PROMs, and satisfaction compared with non-MS-TKA. Independent of prosthesis design, patients with greater sagittal stability demonstrated improved PROMs.
Survival rates
There is still a debate on whether a high level of congruency in MS TKA increases forces at the implant-bone interface, potentially increasing the risk of early implant loosening. One key outcome measure to assess the rates of aseptic loosening is via critical appraisal of large data sets of revision rates associated with different TKA design philosophies. The National Joint Registries provide real-world evidence, although they cannot overcome the potential confounder of patient and surgeon factors. Such data are increasingly used as “gold standard” for assessing implant survival. Bordini et al compared the data from the Italian Register of Orthopaedic Prosthetic Implants and found the 10-year revision-free survival rate of Advance MP TKA was 96%, which was similar to all other TKA (Bordini, Ancarani, and Fitch 2016). Fitch et al systematically reviewed all types of MS TKA reported in 8 studies (1146 MS TKA) (Fitch, Sedacki, and Yang 2014). They found 5-year and 8-year survival rates of 99% and 98%, respectively, which were comparable with the survival rates of other types of cemented TKA in the NJR. A larger more recent meta-analysis assessed revision rates across registries and the literature included data for over 30,000 MS-TKA and found comparable revision rates with other TKA designs (Cassar-Gheiti et al. 2020). The Australian Orthopaedic Association’s NJR (AOANJRR) 2022 report presents data on “medial pivot” (MP) knees. This is the only registry which reports on medial pivot (medial stabilised) as a separate entity. In 2021, MS design prostheses accounted for 9.2% of primary procedures in Australia (AOANJRR 2022). According to AOANJRR, MS designs have a lower rate of revision compared to PS prostheses (4.9% vs 5.5% at 10 years), but a higher rate of revision compared to minimally stabilised prostheses (4.4%). There is no difference in implant survival if the patella is resurfaced. There appears to be no significant difference between the survival rates for MS vs minimally stabilised knees up to 15 years. However, the reported revision rates and cumulative incidence of patella-femoral pain in MS-TKA seems to increase significantly beyond 15 years. There are three potential reasons behind this observation – non-resurfaced patella, small number of patients at risk and/or variation between the performances of different MS-TKA including use of cementless fixation. At 20 years, only 39 MS-TKA are at risk compared to 342 PS and 2,176 minimally stabilised TKA. In addition, grouping of all MS-TKA together can mask outcomes of individual MS-TKA brands. It is therefore difficult to draw any meaningful conclusion from this data.
In addition, various single-centre prospective observational studies have established the safety of MS-TKA. As expected, first generation MS-TKA have the longest follow-up data, with both Advance MP (95.4%) and MRK knees (96.9%) having excellent survival rates at up to 14 years (AOANJRR 2022).
Objective outcomes
Hossain et al undertook a single-blinded RCT of 82 patients and demonstrated improved range of movement for MS knees compared with PS knees at both 1- and 2-years post-surgery (Hossain et al. 2011). A three-armed RCT comparing MS, PS and CR TKA in 90 patients found no difference in complications, Timed up and go (TUG) test or 6 minute walk (6MW) test at six or twelve months post-surgery (Dowsey et al. 2020). A single-surgeon sequential retrospective study comparing MS with PS knees also found no difference in the post-operative gain of flexion at 12 months (Shakespeare, Ledger, and Kinzel 2006).
Patient reported outcomes
PROMs are often used to assess objective outcomes of orthopaedic implants based on patient satisfaction. Ishida et al studied patients who had undergone MS-TKA (n=20), comparing them with 20 PS double-high insert TKA (Ishida, Matsumoto, Tsumura, et al. 2014). At the 4 to 5 years follow-up, there was no difference in Knee Society Scores (KSS), Knee Society Functional Scores (KSFS), and UCLA activity score, although this study may have been inadequately powered. A single surgeon prospective study comparing 44 CR and 46 MS knees had mixed results (French, Munir, and Brighton 2020). The MS knees had better Forgotten Joint Score (FJS), KOOS-12 Quality of Life subscale and KOOS Quality of Life subscale but there was no difference in Oxford Knee Score (OKS), WOMAC, UCLA activity scale, Visual Analogue Scale-Satisfaction or ROM. Similarly, Hossain et al found an improved physical component of SF-36 and Total Knee Function questionnaire, but no difference in American Knee Society, WOMAC or OKS (Hossain et al. 2011). A recent systematic review and meta-analysis studied 4,102 TKA across 22 studies demonstrating mixed results (Nisar et al. 2022). OKS was better in MS-TKA, but with no difference in FJS, WOMAC, KSS-knee, KSS-function or ROM.
A single-centre prospective observational study by Katchky et al reported five-year clinical results in 100 consecutive MS-TKA in 92 patients (Am et al. 2019). At five-years, three patients had died (three TKA) and a further two TKA were revised. Of the remaining 95 TKA, five-year follow-up data were available for 81 TKA (85%). There were significant improvements in all PROMs and high satisfaction. The mean ROM at final follow-up was from 0° (full extension) to 124° flexion. There were seven major complications (7%): one infection, two deep vein thromboses, one cerebrovascular event, and two patients with stiffness requiring a manipulation under anaesthesia. Two patients required a lateral retinacular release to optimize patellar tracking in valgus knees; no additional ligament releases were performed in any patient. Radiological analysis demonstrated no evidence of implant-related complications.
In-vivo knee kinematics
It is important to establish if MS-TKA behaves like the normal knee in vivo. Various studies have tried to assess this with in vivo kinematic evaluation during various phases of gait and/or standardised knee ROM exercises. Schütz et al compared changes in joint kinematics introduced by MS-TKA design during gait activities compared with fixed-bearing PS and ultra-congruent (UC) mobile-bearing geometries (Schütz et al. 2019). Subjects were analysed throughout complete cycles of gait activities using dynamic video-fluoroscopy. The MS-TKA showed the smallest range of medial compartment AP translation for level walking, downhill walking, and stair descent (3.6 ± 0.9 mm, 3.1 ± 0.8 mm, 3.9 ± 1.3 mm), followed by the UC (5.7 ± 1.0 mm, 8.0 ± 1.7 mm, 8.7 ± 1.9 mm) and the PS (10.3 ± 2.2 mm, 10.1 ± 2.6 mm, 11.6 ± 1.6 mm) geometries. The MS-TKA also exhibited the largest range of lateral compartment AP translation (12.1 ± 2.2 mm), and the largest range of tibial internal/external rotation (13.2 ± 2.2°), both during stair descent. This study has shown that the MS-TKA clearly restricts AP motion of the medial condyle during gait activities while still allowing a large range of axial rotation.
Shimmin et al reported a single-surgeon series of 14 consecutive patients with a minimum 24 month follow-up (Shimmin et al. 2015). They performed clinically relevant functional activities of pivoting, kneeling, lunge and step-up/down activities while knee motion was recorded by video-fluoroscopy. Mean maximum knee flexion during kneeling activity was 127° (100°-155°). An asymmetric posterior translation of the lateral femoral condyle was observed during all the activities without any paradoxical anterior translation of the femoral condyles in any activity.
Beach et al compared three matched groups (18 per group) with MS, PS and CR TKA using motion analysis and surface electromyography during step-ascent and walking tasks (Beach et al. 2019). MS-TKA exhibited a greater range of absolute tibial motion compared with the CR knee and significantly greater knee extensor activation during the step-ascent compared to the PS group during the step-ascent task.
Consideration of alignment technique also adds an additional dimension to the discussion around MS-TKA. The traditional alignment philosophy utilises mechanical alignment; the creation of a neutral mechanical axis (hip-knee-ankle angle) in the coronal plane. This technique is highly reproducible but necessarily changes the patient’s native anatomy as only 0.1% of patients naturally have a neutral mechanical axis (Almaawi et al. 2017). Kinematic alignment (KA) is an alternative technique which aims to restore pre-arthritic anatomy, including all three axis. Given that KA aims to restore natural lower limb axes and MS-TKA aims to restore natural tibiofemoral kinematics, recent work has emerged which aims to combine the two. Early small studies suggest similar or even better results compared with traditional techniques (French, Munir, and Brighton 2020; Risitano et al. 2020; Malavolta et al. 2022).
Conclusions
Despite decades of development and millions of successful TKA procedures, there remains residual dissatisfaction in many patients. The majority of implants are PS or CR, and are based on the crossed-four-bar link model theory of tibiofemoral articulation (O’Connor et al. 1989). Anatomical studies of the normal knee appear to disagree with this model, leading to the development of the medially stabilised TKA implant (Weber and Weber 1836; Freeman and Pinskerova 2005; Iwaki, Pinskerova, and Freeman 2000). This appears to better mimic normal knee movement.
A number of studies explore outcomes of the MS knee compared with the PS or CR knee implants (Nisar et al. 2022). The MS knee revision rate appears to be comparable with other implant types in both medium and long term (Cassar-Gheiti et al. 2020; Bordini, Ancarani, and Fitch 2016; Fitch, Sedacki, and Yang 2014; Karachalios et al. 2016). Despite the MS knee appearing more anatomical in its biomechanics, studies exploring objective and subjective outcomes present more mixed results. Some studies suggested improved functional outcomes of MS knees in ROM, TUG test, and 6MW test (Hossain et al. 2011; Nakamura, Inoue, Suguro, et al. 2018), while others found no difference (Dowsey et al. 2020; Shakespeare, Ledger, and Kinzel 2006). Similarly, PROMs for MS knees were no different in some (Ishida, Matsumoto, Tsumura, et al. 2014; French, Munir, and Brighton 2020), while others found better scores for some PROMs (Hossain et al. 2011; Nisar et al. 2022; French, Munir, and Brighton 2020). In summary, MS-TKA tends to show at least as good survival as non-MS-TKA with better function likely due to increased AP stability and lack of paradoxical movement of femur over tibia as seen with both CR and PS designs.
There are limitations to the study of MS knee outcomes which may affect findings. Long term survival rates are only available for first generation implants developed at the turn of the century; the other seven implant designs have not been on the market long enough for this data (Nisar et al. 2022). Additionally, functional outcomes and PROMs studies are generally small, single surgeon data sets. These are often inadequately powered for conclusive results and affected by limitations such as learning curve and selection bias. Large multicentre RCTs would be the ideal solution but present obvious logistical challenges. Another potential limitation is grouping of all MS-TKA together. Although in the same “class”, there are subtle differences between articular geometry and patella-femoral joint (PFJ) kinematics of different MS-TKA and grouping them together prevents individual comparisons. However, to do so, large data sets of each MS-TKA with long term follow up is needed. This is likely to be possible in coming years as MS-TKA increase in popularity.
Some other designs claim to be medial-stabilised TKA but are either not fully conforming or only use a medial congruent bearing which can cause kinematic conflict with the PCL. One example includes use of a medial congruent (MC) bearing with a multi-radius femur. Although it reduces additional inventory requirement and increases interchangeability between a CR and a MC bearing, it is counterintuitive and paradoxical to the principle of MS-TKA. Another example is a non-congruent bearing in a single radius femur. Either of these concepts tend to provide true conformity only in extension and not through the arc of knee flexion from 00 to 900, a prerequisite for a MS-TKA in normal activity.
Future work should interrogate individual MS-TKA with respect to long-term real-world data to establish their efficacy and reasons for revision surgery. Detailed analysis of real-world data for individual MS-TKA is needed as opposed to overall performance of MS-TKA implants as a group. Although broadly similar (with a congruent medial condylar articulation), various other features (e.g., geometry of the PFJ articulation) can significantly impact performance of a TKA. Such analyses would help establish long-term success of each MS-TKA implant and highlight differences in the clinical outcomes. To be meaningful, patient cohorts should be propensity matched to reduce heterogeneity in data introduced by confounders such as age, gender, BMI, pre-operative deformity, and surgical technique used to include alignment philosophy and patella resurfacing status.
Acknowledgements
Hemant Pandit, Sam King and Jeya Palan are supported in part by the National Institute for Health and Care Research (NIHR) Leeds Biomedical Research Centre (BRC) (NIHR203331). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.




.png)
.png)


.png)
.png)