INTRODUCTION
Total knee arthroplasty (TKA) falls within the top 20 list of operating room procedures performed in both inpatient and outpatient settings, with the number of TKAs in the USA projected to reach 1.26 million annually by 2030 (McDermott and Liang 2021a, 2021b; Sloan, Premkumar, and Sheth 2018). With the advancements in perioperative surgical techniques and post-operative (PO) rehabilitation procedures, TKA is the preferred surgical intervention to relieve pain and improve joint function in patients with osteoarthritis who have failed conservative treatments (Hsu and Siwiec 2022).
Although TKA has a high satisfaction rate, the tissue injury sustained during the procedure causes a complex cascade of immune inflammatory responses that results in significant lower extremity edema (Yang et al. 2023). The highly invasive nature of the TKA procedure can result in significant tissue damage causing the release of Damage-Associated Molecular Patterns (DAMPs), which are molecules that trigger tissue-intrinsic and tissue-extrinsic responses initiating the pro-inflammatory cascade (Arias, Aller, and Arias 2009; Roh and Sohn 2018; Szpaderska and DiPietro 2005). An unchecked inflammatory response can cause a “swelling tsunami” in the affected joint due to increased vascular permeability, fluid extravasation, and fluid displacement to the subcutaneous tissue causing a pathophysiologic state called interstitial inflammatory stasis, resulting in chronic pain syndrome (Tuckey et al. 2021; Wickline et al. 2023). On a proteomic and cellular level, the inflammatory cascade involves the active recruitment of circulating immune cells like neutrophils and monocytes from the blood into the tissue, as well as the recruitment of tissue resident macrophages that release cytokines and chemokines which contribute to joint effusion and soft tissue edema (Chovatiya and Medzhitov 2014; Preston et al. 2016; Pittman and Kubes 2013). Matrix metalloproteinases (MMPs) are a family of calcium dependent, zinc-containing proteolytic enzymes that play a central role in normal and pathological inflammatory processes of wound healing by degrading various extracellular matrix (ECM) components and mediating ECM remodeling. Macrophages and neutrophils recruited in the inflammatory phase are the main sources of MMPs (Caley, Martins, and O’Toole 2015; Chen et al. 2013). Mitigating the deleterious inflammatory loop by decreasing the activity of early chemokines and MMPs and facilitating the beneficial proliferative and remodeling phases of wound healing could be advantageous in limiting swelling and pain post TKA.
Swelling following TKA causes pain, reduced range of motion (ROM), and slower recovery with 10–34% of patients experiencing pain between three months and five years following surgery and 20% of patients reporting worse swelling and pain post-operatively than preoperatively (Beswick et al. 2012; Li et al. 2020). An accurate and reliable method to quantify PO swelling is critical to monitoring the efficacy of treatments to manage inflammation and edema. Technologies like bioimpedance spectroscopy (BIS) and magnetic resonance imaging (MRI), although expensive and time consuming, enable precise quantification of knee swelling that traditional volumetric and circumferential measurements lack (Yau et al. 2022). Single frequency-bioelectrical impedance assessment (SF-BIA) in conjunction with the development of a reference chart to stratify patients by swelling percentiles is an affordable, less time-consuming, and clinically relevant tool set to accurately measure minute fluctuations in impedance to quantify swelling after TKA, which can be easily performed in the clinician’s office at point of care (Loyd et al. 2020, 2021).
Although PO swelling is a significant and common complication associated with primary TKA, periprosthetic joint infections (PJI), albeit at much lower incidence rates than swelling complications, can be costly and clinically challenging complications (Premkumar et al. 2021). Most infections including PJI are attributed to the formation of biofilm . Biofilms are complex microbial communities sheathed within a protective matrix of self-produced extracellular polymeric substances (EPS) which once formed, are notoriously difficult to eradicate (Yadav et al. 2020; Vestby et al. 2020). Thus, multi-tiered infection prevention regimens, including the use of intraoperative antimicrobial irrigants are recommended to prevent the microbial contamination and subsequent development of biofilm within the surgical wound space (Tarabichi and Parvizi 2023).
The purpose of this pilot study was to evaluate the hypothesis that the intraoperative use of the novel antimicrobial surgical irrigant, XPERIENCE® Advanced Surgical Irrigation (XP) , designed as an intraoperative surgical irrigant to remove debris, including microorganisms from the wound space, would also decrease PO swelling, and improve functional outcomes post TKA by potentially acting as an inflammatory modulator in the surgical wound space .
METHODS
Study design
The study protocol was reviewed and approved by the Institutional Review Board (IRB) for the Protection of Human Subjects of St. Elizabeth’s Medical Center in Utica, NY. The study was designed as a non-randomized, controlled, multisite, pilot clinical study. Sites included in the study were Genesee Orthopedics & Plastic Surgery Associates in New Hartford, NY, St. Elizabeth Medical Center in Utica, NY and Apex Surgical in Westmoreland, NY. All TKA procedures were conducted by a single surgeon who served as the principal investigator of the study.
Subjects were consented into the protocol in a non-randomized manner based on inclusion/exclusion criteria listed below. The first 30 subjects were enrolled in the control arm and were treated intraoperatively with approximately 0.44% dilute PI, which is within the literature reported PI dilution ranges (0.3%->0.5%) used in primary arthroplasty ( Goswami and Austin 2019, AAOS Toolkits, Siddiqi et al. 2021) . The subsequent 31 subjects were enrolled in the intervention arm and treated intraoperatively with undiluted XP.
Inclusion criteria
-
Unilateral primary total knee replacement.
-
18 years or older.
Exclusion criteria
-
Previous major lower extremity surgery within 6 months on the opposite side or major lower extremity surgery on opposite side with permanent resultant lymphedema / swelling.
-
One leg markedly larger than the other (>20%).
-
Dialysis, or glomerular filtration rate < 30 mL/min/1.73 min2.
-
Previous vein harvesting for coronary artery bypass graft,
-
Previous vein surgery.
-
Previous artery bypass below aortic bifurcation.
-
Pregnancy or lactating.
-
Subjects unable to follow study protocol instructions or provide informed consent.
-
Subjects on loop diuretics (furosemide or torsemide or bumetanide).
-
Rheumatoid arthritis.
-
Sensitivity/allergy to Betadine or PI.
-
Pre-op narcotic use (> 5 pills within previous 90 days).
-
Use of anticoagulants other than aspirin (e.g., warfarin, clopidogrel, enoxaparin, apixaban, rivaroxaban).
-
Has an implanted cardiac rhythm management device (pacemaker or implantable cardioverter defibrillator).
-
Resides >20 miles from the orthopedic office, limiting the practicality of in-home visits by the research staff on defined post-operative days (POD) for endpoint measurements.
The primary endpoint was percent swelling measurements by SF-BIA to generate a 6-week swelling curve while the secondary endpoints included evaluation of range of motion (ROM), dependence on ambulatory assistive devices (AADs), opioid usage and pain scores. Table 1 lists the endpoints analyzed, and associated instrumentation, methodology or rating scale used at the various time points pre- and post-operatively.
Percent swelling measured by SF-BIA
Single frequency-bioimpedance assessment was used to measure lower extremity swelling (Loyd et al. 2020, 2021; Wickline et al. 2023). Measurements were obtained using the Quantum® II body composition analyzer (RJL Systems, Clinton Township, MI). Subjects were made to lie flat for 10 minutes. Four surface electrodes were placed on the non-surgical limb as described below.
-
20 cm proximal to the superior pole of the patellar over the midline of the thigh.
-
10 cm proximal to the superior pole of the patellar over the midline of the thigh.
-
On a point midway between the medial and lateral malleolus.
-
10 cm distal to the midway point between the malleoli over the 2nd ray.
Once appropriately placed, the electrodes were attached to the SF-BIA device. The device was turned on and after a lag of at least 5 seconds, values were recorded. The same procedure was then followed for the planned surgical limb. Lower levels of assessed bioimpedance indicated higher fluid content and therefore greater swelling. Percent swelling was calculated as a difference in the surgical limb to the non-surgical limb using the formula: (1-(surgical limb BIA/non-surgical limb BIA)) *100. Normalizing swelling in the surgical limb against the non-surgical limb of the same patient enabled accurate measurements of changes in fluid status in the surgical limb over time and allowed for valid swelling curve comparisons within and between cohorts despite the variability in body compositions. The time points and time frame for swelling evaluations were selected based on prior observations by the principal investigator on typical post TKA pain spikes noted in the practice with an assumption of correlates of pain to swelling.
Ambulatory Assistive Device Usage
Subjects were queried about usage of AADs at each visit. Changes in AAD dependence between visits were not considered. If subjects indicated no device used or knee brace used, they were scored at 0. Subjects indicating use of a cane, crutches or a walker were scored at 1.
Intraoperative surgical irrigants
Ten percent PI sterile solution (0.75oz/packet) (EuroAmerican, Pompano Beach, FL) was diluted in 500 mL of sterile saline resulting in a final 0.44% dilute PI solution used in the control cohort. Povidone iodine is a water-soluble iodine-releasing agent with the free iodine acting as the active bactericidal agent. The free iodine molecules can penetrate microorganisms causing oxidization of proteins, nucleotides, and fatty acids, eventually leading to cell death (Lepelletier et al. 2020). Although dilute PI solution has been advocated for wound irrigation by the American Academy of Orthopedic Surgeons (AAOS), Centers for Disease Control and Prevention (CDC), World Health Organization (WHO), and the International Consensus on Orthopedic Infections (AAOS Toolkits, n.d.; Berríos-Torres et al. 2017; WHO 2018; Blom et al. 2019), there is no standard recommendation of final PI concentration and volume that should be used.
XPERIENCE Advanced Surgical Irrigation (500 mL/container) (Next Science®, Jacksonville, FL), was used undiluted in the intervention cohort. It is an FDA cleared product available as a sterile solution and is indicated for use as an irrigant to clean and remove debris including microorganisms from the surgical wound space. It was designed based on a patented technology platform called XBIOTM that utilizes material science approaches to prevent the formation of biofilm, as well as treat and remove established biofilm. (Biofilm and Antibiotic Resistance Solutions). XPERIENCE (pH 3.93), consists of citric acid, sodium citrate, and sodium lauryl sulfate in water with citric acid and sodium citrate serving as pH buffers and aiding in metal ion chelation, while sodium lauryl sulfate acts as the surfactant, assisting in lysis and removal of microorganisms. The “no-rinse” feature enables residual XP to continue its activity for a prolonged time in the surgical wound space post closure (Bashyal et al. 2022).
Surgical procedures for control and intervention cohorts
All TKA surgeries were conducted by a single surgeon using an identical cemented medial pivot prosthesis and an unrestricted kinematic alignment philosophy using a medial parapatellar approach (Medacta GMK Sphere, Castel San Pietro, Switzerland). The patella was never everted. Every subject had the patella resurfaced, no subject had the MCL released, and no tourniquet was utilized, including during cementation.
For the first set of 30 subjects comprising the control cohort, 0.9% sterile saline was used as the surgical irrigant. Prior to closure of the deep layer, 500 mL of 0.44% PI was applied and allowed to sit in the surgical wound space for 3 minutes. Povidone iodine was then rinsed from the wound with 1000 mL of saline using pulsatile lavage followed by closure of the deep layer. After deep closure, the surrounding superficial layer was rinsed with 500 mL of saline using pulsatile lavage prior to closure of the superficial layers.
After completion of 30 surgical TKA procedures for the control cohort, the next 31 subjects were enrolled in the XP cohort. A total volume of 500 mL of XP was used during the entire surgery. Briefly, subjects were treated with 250 mL of XP using a bulb syringe at the beginning of implantation and 200 mL at the end of implantation after saline pulsatile lavage. Excess solution was suctioned from the surgical cavity, but the product was not rinsed out after the 200 mL addition of XP at the end of implantation. Finally, 50 mL of XP was placed over the arthrotomy closure after saline pulsatile lavage.
Perioperative standard of care (SOC) and patient education
The principal investigator has developed multimodal perioperative protocols focused on identifying limb edema preoperatively and has instituted intraoperative and PO techniques that decrease swelling and dependence on opioids with marked success (Stevenson and Wickline 2020; Wickline and Corrado 2021; Wickline et al. 2023). Subjects received the same detailed education booklet, viewed the same pre and post operative videos, and followed the same home-based physical therapy protocols, including the maximum daily step count for six weeks after surgery (Wickline et al. 2023).
Data handling and data collation
All source data collated for the study was managed according to the requirements of the Health Insurance Portability and Accountability Act of 1996 (HIPAA). The study case report forms (CRFs) were the primary source data collated for the study. Data was also extracted from hospital records, clinical charts, laboratory results, evaluation checklists, pharmacy dispensing records and recorded data from automated instruments.
Statistical evaluations
Five parameters were assessed for change over time between the two arms of the study: swelling, ROM, ambulatory assistive device (AAD) usage, opioid use, and pain score. Swelling and pain score were analyzed as continuous factors using pairwise Wilcoxon signed rank tests at each time point. Range of motion was compared to baseline values and assigned a binary value based on whether range of motion was (1) or was not (0) returned to at least the baseline ROM prior to surgery. Range of motion, opioid use, and AAD use were analyzed as binary factors, with a two-tailed Fisher’s exact test used to determine statistical significance at each time point. Statistical analyses were conducted using R v4.3 (R Foundation for Statistical Computing, Vienna, Austria ) . Two control and one intervention subjects were excluded from ROM analysis since they lacked baseline ROM data. In two subjects where there was incomplete follow-up, the Last-One-Carried-Forward (LOCF) method was used to fill missing data points with the previous observed value from the same subject.
RESULTS
In total, 68 subjects were screened for enrollment in the study. Thirty subjects were enrolled in the control cohort and 31 subjects were enrolled in the XP cohort. Study enrollment was completed in 12 months. Demographic and comorbidity information for the control and XP cohorts are presented in table 2. There were no significant differences in the demographic and comorbidity profiles noted between the two cohorts (table 2). A higher number of women and predominantly white population comprised both cohorts. Sixty three percent of subjects in the control cohort and 58% of subjects in the XP cohort exhibited BMI>30 while 10% in each cohort were diabetic with HgA1C values>6.5.
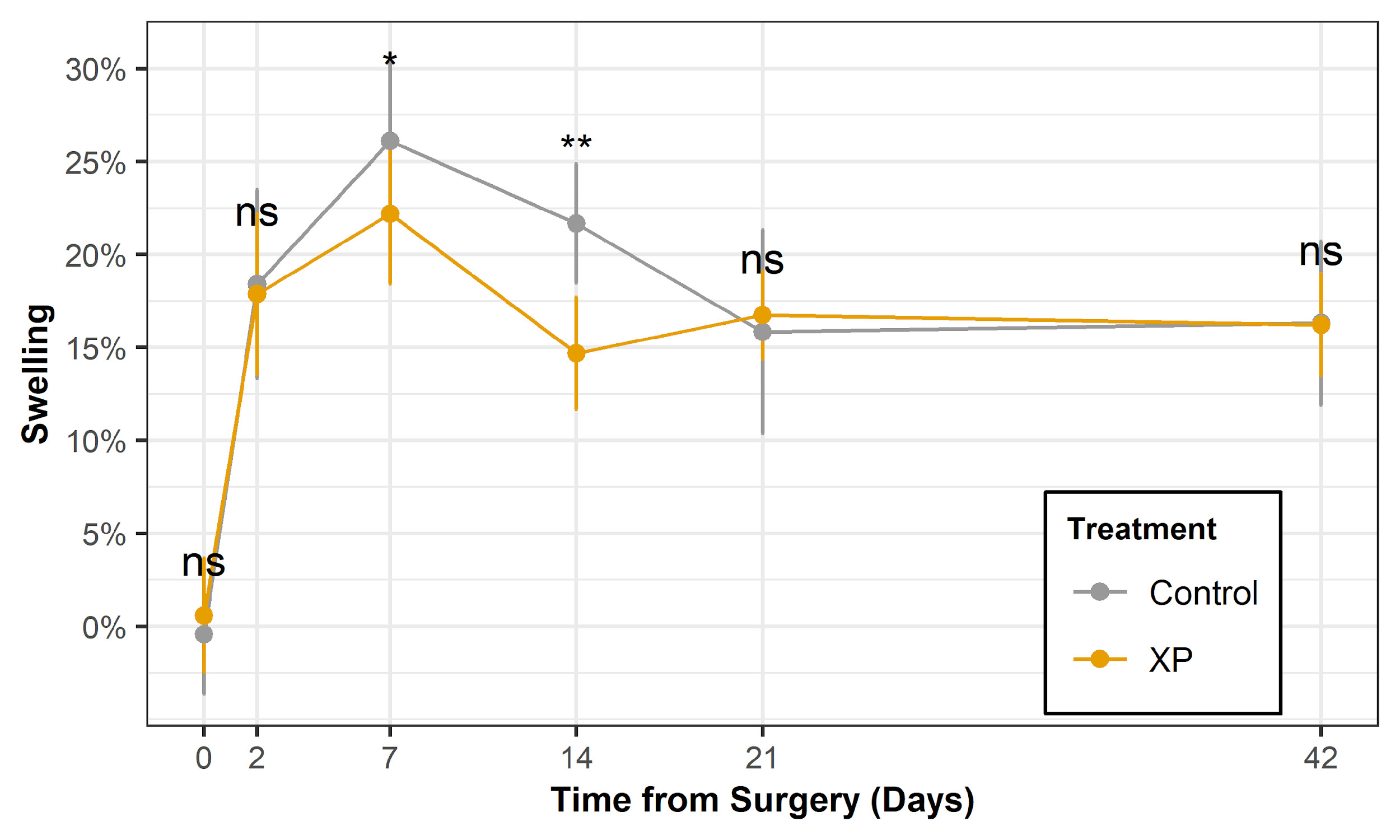
To evaluate edema as an indication of inflammation in the lower extremity post-surgery, swelling was measured using SF-BIA. The XP cohort exhibited significantly reduced swelling (p<0.05) at days 7 and 14 when compared to the control cohort (figure 1A). Percent swelling on day 7 was 26.1% in PI cohort versus 22.2% in XP cohort and 21.7% in control PI cohort versus 14.7% in XP cohort on day 14. Figure 1B indicates swelling curves in the pilot study in relation to the literature reported reference standard. Comparison of both control and XP swelling curves to the reference curves presented in the literature determined that both cohorts trended towards the 10th percentile of the reference curve indicating optimal swelling management compared to the reference standards participants (Loyd et al. 2020).
To evaluate limb functionality, subjects were assessed for their ability to regain at least baseline or better ROM. Subjects in the XP cohort exhibited significantly greater return to baseline ROM at day 7 compared to the control PI cohort (table 3).
Table 4 summarizes dependence on AADs over the 6-week period for the control and XP cohorts. The XP cohort exhibited at least a 10% lower AAD usage compared to the control cohort at 7 days and all days following, with statistical significance at day 21 (p = 0.049).
An exponential decay function was used to estimate the time to mid-point for AAD usage in each cohort (figure 2). The XP cohort exhibited a quicker 50% “device-free” profile reaching half of maximum percentage of patients using AADs by day 12 while the control cohort achieved the equivalent ratio statistic by day 19, indicating a 7-day estimated improvement in the XP cohort. Thus, evaluation of both functional parameters of ROM and AADs indicated quicker “return of limb functionality” with use of XP.
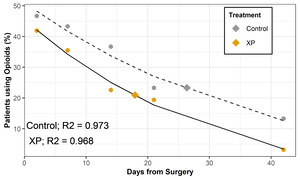
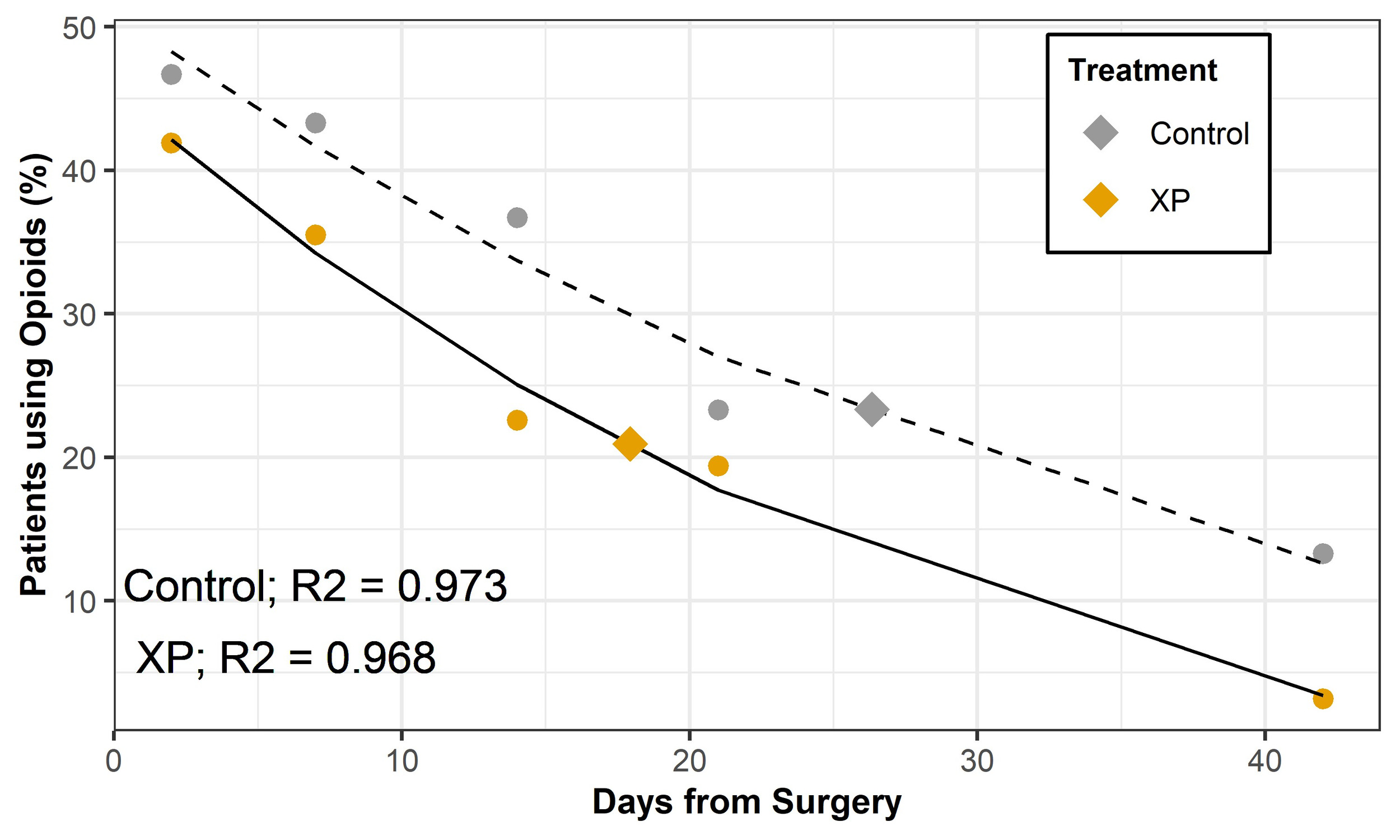
Opioid use was summarized as a binary response regardless of drug prescription and dosage (none=0, opioids used=1). Table 5 indicates a decrease in opioid use over time for the control and XPERIENCE cohort. Though the comparisons did not reach statistical significance, opioid usage was between 4 and 14 absolute percentage points lower in the XP cohort compared to control cohort at each time point.
An exponential decay function was used to estimate the time to mid-point for opioid usage in each cohort (figure 3). Fitting an exponential decay to the opioid use curve from peak to end determined the half-life of percentage of subjects using opioid between control and XP cohorts. In this pilot study, the XP cohort exhibited quicker “weaning off opioids” reaching half of maximum percentage of subjects on opioids by day 18 while the control PI cohort achieved the same statistic at day 26 indicating an 8-day estimated improvement in the XP cohort.
Evaluation of pain using NRS determined that there were no significant differences in perceived levels of pain between the cohorts at any time points measured (figure 4).
Correlations were used to evaluate the relationship between the key parameter of swelling associated with inflammation and the other measures evaluated in the study (figure 5). Underscoring the relatedness of these measurements, reduced swelling was significantly associated with increased return of range of motion (R-sq 64%) and decreased reliance on device usage (R-sq 45%). Decreased opioid usage and pain were considered as surrogate indicators of improved quality of life. The increase in swelling correlated with an increase in the percentage of patients using opioids (R-sq 63%) but in this pilot study, swelling was not significantly associated with patients’ reported perception of pain (R-sq 1.2%).
DISCUSSION
Total knee arthroplasty is the second and 16th most common operating room surgical procedure performed on an in-patient and ambulatory basis respectively (McDermott and Liang 2018, McDermott and Liang 2019). Based on various projections, TKA volumes are expected to reach 1.26 million to as high as 1.92 million surgeries annually by 2030 (Sloan, Premkumar, and Sheth 2018; Singh et al. 2019). Post-operative pain is a significant concern in patients undergoing surgery (Londhe et al. 2021). Notwithstanding the improvements in TKA procedures, 10-34% of patients are dissatisfied with their outcomes due to lack of improvement in functional movement and persistence of pain (Beswick et al. 2012) . Control of postoperative edema, an expected sequelae to TKA, is essential for successful outcomes post-surgery (Wickline et al. 2023).
To decrease PO swelling in TKA patients, the principal investigator instituted multimodal swelling reduction protocols as SOC, with marked success noted in post operative swelling, improved functional outcomes, and associated decreased need for opioids and post operative physical therapy (Stevenson and Wickline 2020; Wickline and Corrado 2021; Wickline et al. 2023). Following AAOS, CDC, WHO and ICM recommendations for infection prevention, the principal investigator uses dilute PI intraoperatively as SOC.
Percent swelling measured by SF-BIA and the swelling curves generated over 6 weeks post index TKA in the pilot study determined that the control cohort exhibited swelling profiles that were equivalent to the lowest 10th percentile swelling curves in the reference standard (Loyd et al. 2020), thus validating the efficacy of the multimodal swelling-reduction regimen instituted at the facility (Wickline et al. 2023). It was notable that a single intraoperative treatment with XP was able to significantly decrease swelling at POD 7 and 14 when compared to the control cohort, indicating a considerable additive effect of XP to the inherently successful SOC multimodal swelling reduction regimen.
Given that a portion of the multimodal swelling reduction regimen includes self-implemented (at home protocols), active adherence by the patients to these protocols is required for success. The primary investigator has endeavored to design home-based protocols that are detailed and simplified which has been instrumental to adherence and success. A meta-analysis analyzing more than 2000 patients did not show a significant clinical difference in improving pain, function, and mobility outcomes after TKA between supervised and unsupervised physical therapy (Bravi et al. 2023). Thus, home-based physical therapy protocols as implemented in this pilot study are appropriate for ensuring success of multimodal swelling reduction regimens.
To evaluate functional recovery post TKA between the cohorts, ROM, and dependence on AAD were determined. A statistically significant improvement in ROM at POD 7 and a significantly decreased dependence on AADs at POD 21 in the XP cohort were noted compared to control PI. It was notable that t he XP cohort exhibited a 7-day estimated improvement reaching half of maximum percentage of patients using AADs compared to the control cohort. Evaluation of both functional parameters of ROM and AADs indicated quicker “return of limb functionality” with XP intervention.
Opioid misuse and related deaths are serious health problems in the United States (US) with opioids involved in 80,411 overdose deaths in the US in 2021 (CDC 2021). Orthopedic surgeons have the third highest per capita rate of opioid prescribing of all medical specialties (Guy and Zhang 2018). Excessive and prolonged opioid prescriptions post TKA have been widely reported. A national database query of 113,337 TKAs in the USA determined that approximately 31.5% the patients were prescribed narcotics for more than 3 months postoperatively which was associated with an increased risk of short-term and long-term complications following TKA (Cancienne et al. 2018) while a retrospective study of Medicaid patients undergoing TKA determined that 69.9% of patients continued opioid use 90 to 270 days after discharge (Ward et al. 2022).
Instituting protocols that minimize opioid use should be a mainstay in all orthopedic practices. In a prior study of the orthopedic practice conducting this pilot study, multimodal perioperative pain control protocols to decrease opioid use after TKA resulted in 18.9% of subjects not requiring any opioids throughout their 12-week PO episode of care while 86.3% of patients needed 10 or fewer opioids in total through 12 weeks postoperatively (Stevenson and Wickline 2020). In the current pilot study, 33% of subjects in the control cohort and 52% of subjects in the XP cohort did not require any opioids in the 6-weeks post TKA although the intraoperative treatment with XP did not statistically reduce opioid use at each POD compared to the PI group nor was there a statistical significance in pain scores.
The overall results in this pilot study warrant further definitive investigations of XP on PO swelling, limb function, opioid use and reported pain outcomes in appropriately powered, multicenter, randomized, controlled clinical trials, with a focus in clinical settings where multimodal swelling reduction regimens are not actively implemented post primary and secondary knee replacements. Preclinical and clinical studies interrogating the mechanistic activity of XP on inflammation and swelling in the wound space milieu in TKA are also warranted. While this pilot study did not evaluate the mechanisms of action of XP in decreasing swelling post TKA, preclinical studies conducted with a wound gel designed on the same XBIO technology platform as XP, resulted in decreased proinflammatory chemokines in the wound space and enhanced wound healing timelines (Bounds et al. 2021) thus indicating that a similar function could be hypothesized with XP in the surgical wound space. The “no-rinse” feature of XP would potentially enable continued activity of residual product within the wound space for prolonged times without negatively affecting host tissue (Bashyal et al. 2022; Cheng et al. 2022). Conversely, intraoperative treatment with dilute PI is limited to a few minutes and followed by an extensive saline rinse to obviate tissue cytotoxicity.
A correlation analysis of percent swelling with all parameters tested (ROM, AAD, opioid use, and pain score) indicated that managing swelling intraoperatively could be crucial in managing downstream/side effects of inflammation and warrants the pursuit of novel therapies like XP with potential multi-functional modes of action and capabilities of addressing dual complications of infection and inflammation related adverse events in joint arthroplasties.
LIMITATIONS
This pilot study represents the initial evaluation of XP as part of a swelling management regimen in a single surgeon’s practice. The study was non-randomized, wherein the control PI cohort was completely enrolled before the intervention XP cohort. Thus, any learning curve difficulties with study protocols, instrumentation and measurements would likely be manifested in the control cohort. The pilot study results may not be generalizable to other practices that follow alternative TKA protocols. Validating and extrapolating the findings more broadly will require definitive, powered, randomized, controlled, multi-site and multi-surgeon clinical study.
CONCLUSION
Detrimental edema attributed to unmitigated host pro-inflammatory processes post TKA can delay functional recovery of the joint. Strategies to reduce PO swelling by modulating inflammatory responses could prove beneficial. This pilot study was designed to evaluate the impact of the intraoperative use of XP on PO swelling and associated parameters of ROM, AAD usage, opioid use, and perceived pain. These preliminary results indicated that XP decreased swelling, improved ROM, and decreased usage of AAD in a statistically significant manner when compared to control. This indicates the potential utility of XP as a multifunctional, anti-inflammatory, and anti-microbial intraoperative surgical irrigant in joint arthroplasty.
Acknowledgments
Dr. Matthew Melin and Dr. Richard Southgate for reviewing the paper.
Dr. Craig Tipton at RTL Genomics, Lubbock, TX for conducting the statistical analysis.