INTRODUCTION
Arthroscopy is a minimally invasive surgical procedure for the visualization, diagnosis, and treatment of joint damage. An arthroscope, which is a narrow tube containing a system of lenses, is inserted into the body through a small incision. The arthroscope is attached to a video camera and light for visualization of the surgical field. Video is transmitted from the camera via a monitoring system that allows the surgeon to view the inside of the joint, displayed on a monitor in the operating room (OR). The camera and light are connected to an instrumentation tower by two cables, providing both power and fiber-optic light to the device. These cables can be cumbersome, routed across or around the patient, and have been implicated in both patient burns and healthcare-associated infections (HCAIs) when the sterile field is compromised. The novel ArthroFree device features wireless communication, providing surgeons with untethered movement and eliminating cable-associated risks. A high-efficiency, laser-based light source combined with proprietary wireless and battery technologies has made the first FDA-cleared wireless surgical camera for arthroscopy possible.
Input on the design of the ArthroFree device was sought from surgeons early in development in a low-fidelity formative usability study (Design Concepts 2019). With the objective of selecting preferred design features, the study used non-functional prototypes of the wireless surgical camera to obtain feedback. Inline and pistol handles, different sizes and weights, and multiple locations of buttons and camera controls were among the features evaluated. Results from the formative study were used to refine the device into the current model of the ArthroFree, designed to meet end-user needs. However, the most notable difference between ArthroFree and a conventional arthroscopic camera is not found in these features, but in the absence of a power and light cable (Figure 1).
Here we describe a human factors evaluation following a design validation study or patient surgery using the optimized design of the ArthroFree device. Human factors science provides valuable feedback on new product development (Arthur et al. 1999; Cagan and Vogel 2013; DeLucia et al. 2006; Dreyfuss 2001; Moody, Arthur, Dibble, et al. 2003; Wills, Logan, and McCredie 1996) by studying the interaction between people and machines (Sanders, n.d.). A human factors survey based on the 5-point Likert scale was administered to surgeons and other medical professionals. The survey evaluated ArthroFree in a surgical procedure performed in a patient, cadaver, or simulated model. The results of the survey were analyzed, and a summary is provided. To collect qualitative feedback, surgeons with independent hands-on experience with ArthroFree commented on the benefits of the device in one-on-one interviews. Analysis of their feedback provides key support for ArthroFree’s usability as the first FDA-cleared wireless surgical camera for arthroscopy.
MATERIALS AND METHODS
Evaluation of the ArthroFree Device in a Human Factors Survey
Recruitment
Lazurite® recruited participants from ten medical facilities with wide-ranging levels of experience in arthroscopic surgery. A total of 76 participants including 70 surgeons and 6 other medical professionals completed the human factors survey after design validation testing. An additional 12 surgeons completed the survey after a clinical evaluation with ArthroFree. A breakdown of participants and their experience and training is reported.
Training and Use
Each participant was provided hands-on training in the operation and use of the ArthroFree system. Training included a review of its components, functions, and visual user interface. Participants were asked to use the ArthroFree hand-held device to perform tasks related to the design of the device such as adjusting camera focus, zoom, and capturing still images and video. Participants then explored the joint capsule of a patient (12 participants), cadaveric (67 participants) or simulant knee (9 participants) model as prescribed by standard medical practice. Other tasks, known to frequently be encountered during arthroscopic surgery and chosen by the participant, we also performed.
Human Factors Survey
Upon completion of training and use, each participant was presented with a 13-statement human factors survey designed for the assessment of ArthroFree. The survey evaluated each user’s experience with the ArthroFree device based on ergonomics (weight, balance, comfort), ease of use (navigation buttons, camera function, size/weight of light source, battery indicator, heat), image quality (light/brightness, latency), and patient experience (safety, efficiency, user confidence). Overall results were examined to assess the likelihood of adoption by surgeons.
The users’ opinions on each statement were gauged using a 5-point Likert scale (1 = strongly disagree and 5 = strongly agree). The average score for each statement was calculated. Statements were grouped into categories based on how they related to ergonomics, image quality, ease of use, and patient experience. A score of 3 in any category was interpreted as a neutral response. An increase from 3 indicated a proportional increase in agreement with a statement of approval and considered a good (4) or excellent (5) response. Conversely, a decrease from 3 indicates a proportional decrease in agreement with a statement.
Collecting Qualitative Feedback on the Usability of ArthroFree
Recruitment
Fifteen surgeons were recruited from 9 medical facilities with independent hands-on experience with the ArthroFree device in product demonstrations, simulant models, cadavers, or patients.
Surgeon Interviews
Surgeons experienced with ArthroFree provided qualitative feedback on their experience with the device in one-on-one interviews. Each surgeon was interviewed about their experience with the device and asked to comment on its potential benefits. Interviews were reviewed and benefits common among surgeons were tabulated. Any benefit not specifically mentioned by a surgeon during their interview does not indicate their disagreement, only that it was not raised during the interview.
RESULTS
Human Factors Survey
Participants consisted of 82 surgeons and 6 other medical professionals with experience ranging from 2 – 48 years’ experience (44 participants (50.00%) with 0-15 years of experience, 23 participants (26.14%) with 16 – 30 years of experience, and 21 participants (23.86%) with over 30 years of experience). Forty-five (51.14%) participants were specifically sports fellowship trained and 15 (17.05%) participants were trained in other fellowship programs.
The mean score for all participants in all 13 statements was 4.50 (standard deviation (sd) 0.71, range (r) 4.23 – 4.72) with an overall average of 91.30% (r 86.36 – 97.78%) of responses in agreement with the statements, rating the experience with ArthroFree as good or excellent: i.e., 4 or 5 (Table 1). The highest score for agreement with a single statement was 97.78% of participants giving a good or excellent response to the statement “the navigation buttons were easy to use.” The lowest score, 86.36% of respondents providing a good or excellent response, agreed with the statement “ArthroFree was comfortable to hold.” Notably, 88.10% of participants reported: “I could perform surgery with the same degree of confidence.”
Statements were grouped into categories (Table 2) based on their impact on ergonomics, ease of use, image quality, and patient experience (Table 3). The percentage of responses in agreement for each category ranged from 88.64% to 93.02%. Statements relating to ergonomics (weight, balance, comfort) scored a mean of 4.31 (SD 0.07, r 4.23 – 4.36) with 88.64% (r 86.36 – 90.91%) reporting good or excellent responses. Statements relating to ease of use (navigation buttons, camera function, size/weight of light source, battery indicator, heat) scored a mean of 4.60 (SD 0.09, r 4.49 – 4.72) with 93.02% (r 87.50 – 97.78%) reporting good to excellent responses. Statements relating to image quality (light/brightness, latency) scored a mean of 4.57 (SD 0.21, r 4.42–4.71), with 92.31% (r 90.91–94.55%) reporting good to excellent responses. Statements relating to patient experience (safety, efficiency, and user confidence) scored a mean of 4.52 (SD 0.05, r 4.46 – 4.56), with 91.15% (r 88.10 – 94.32%) reporting good to excellent responses. The overall experience by category scored 4.50 (SD 0.13, r 4.31 – 4.60), with 91.30% (r 88.64 – 93.02%) reporting good to excellent responses and indicative of a high likelihood of adoption by users. The grouping of the 13 statements by category demonstrated the highest mean scores for ease of use, followed by image quality, patient experience, and ergonomics.
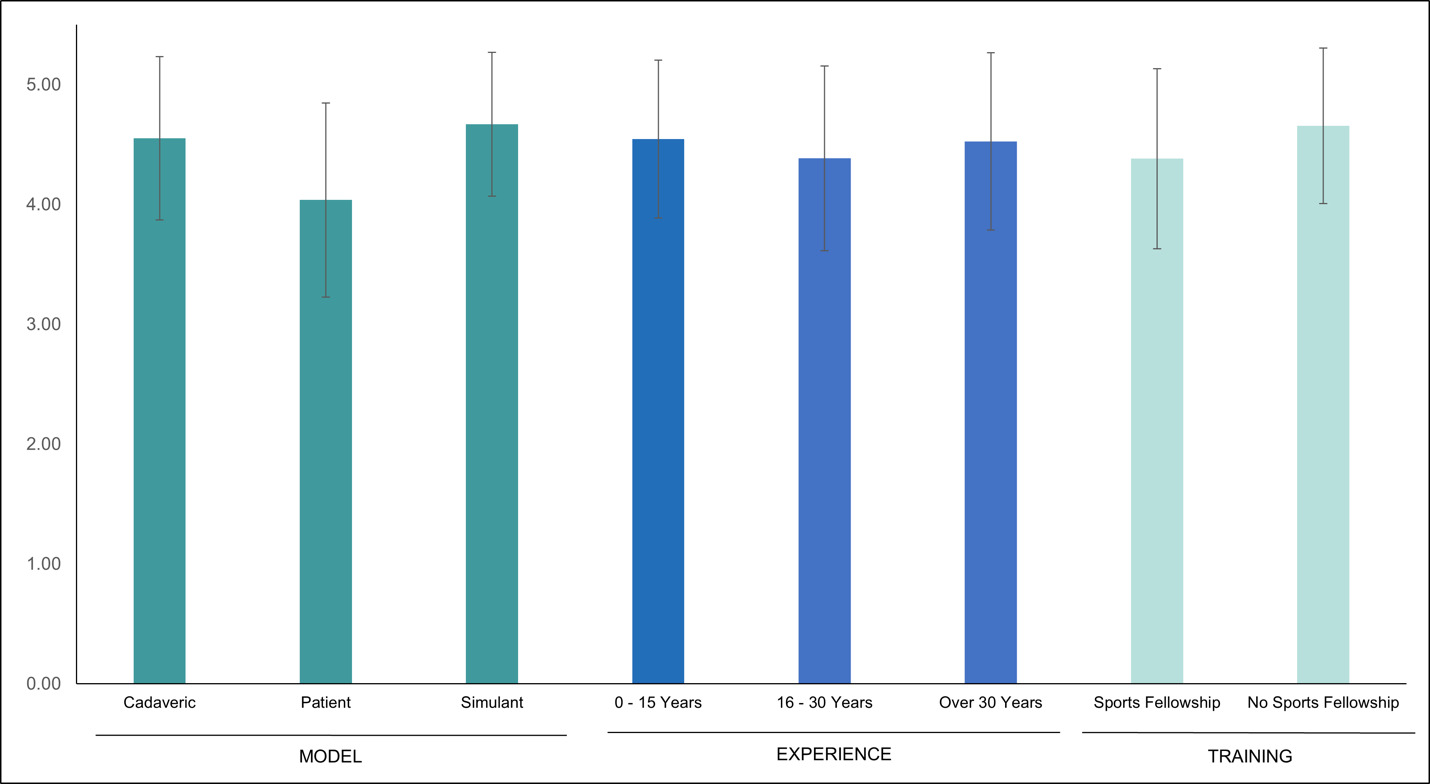
To better understand the impact of the surgical model used and the experience and training of the participants, we examined the difference in overall scores reported within representative groups (Figure 2). Participants using a cadaveric model reported an overall mean score of 4.55 (SD 0.68, r 4.19 – 4.78) with 92.35% agreement (r 83.58 – 97.01%), whereas participants using a simulant model reported an overall mean score of 4.69 (SD 0.60, r 3.90 – 4.78) with 96.30% (r 77.78 – 100.00%). Participants that used ArthroFree in a patient surgery reported an overall mean score of 4.06 (SD 0.81, r 3.08 – 4.50) with 81.06% agreement (r 63.33 – 100.00%). The overall mean score varied little across a broad range of experience; participants with 0 – 15 years of experience reported a mean score of 4.55 (SD 0.66, r 4.27 – 4.80) with 93.27% agreement (r 83.33 – 100.00%), with 16 – 30 years of experience reported a mean score of 4.38 (SD 0.77, r 3.96 – 4.86) with 87.36% agreement (r 73.91 – 100.00%), and with over 30 years of experience reported a mean score of 4.53 (SD 0.74, r 4.09 – 4.33) with 91.43% agreement (r 80.95 – 100.00%). Lastly, participants who were sports fellowship trained reported a mean score of 4.38 (SD 0.75, r 4.13 – 4.64) with 89.10% agreement (r 81.82 – 94.12%), whereas those who were not reported a mean score of 4.63 (SD 0.65, r 4.26 – 5.00) with 93.65% agreement (r 86.05 – 100.00%). None of the differences between these groups were statistically significant.
One-On-One Interviews
Expected benefits of ArthroFree reported by more than half of those interviewed include untethered movement (15/15), decreased setup and teardown times (11/15), and increased efficiency in the OR (8/15). Additional benefits frequently reported include a decrease in the time and cost of the cleaning/sterilization/preparation of the device between surgeries, otherwise known as reprocessing, due to simplification of the components required for surgery (6/15); ease in maintaining the sterile field in absence of the risk of contamination by light and power cords (4/15); and the introduction of new technology to the otherwise long-dormant field of arthroscopy (4/15). Other benefits reported include the decreased risk of fire, burns, or tripping due to cables; the potential for cost savings due to improved efficiency in setup/teardown, surgery, and reprocessing; and the potential for ArthroFree to be utilized for in-office procedures.
DISCUSSION
Wireless technology emerged with the telegraph in the late 1890s (Leone and Robotti 2021) and has since been adopted across numerous industries. However, energy consumption and heat generation of LED light sources have hindered the development of wireless endoscopic camera systems (Williams et al. 2022). Traditional arthroscopes are tethered by cables that provide power and fiber-optic light to the device – and also create risks. Lazurite’s high-efficiency, low-heat Meridiem® light engine—combined with proprietary battery and wireless technology—has made a wireless endoscope camera system possible with ArthroFree.
The current design of the ArthroFree camera head was validated through a human factors survey followed by one-on-one interviews with surgeons. Surveys are cost-effective and easy to administer but have inherent limitations including survey bias, specifically response bias. Response bias refers to factors that can lead respondents to provide inaccurate or false information. This can occur for a variety of reasons including social desirability, a desire to finish quickly, or even a general lack of interest. The importance of providing honest, accurate answers was clearly communicated to all participants in advance of both surveys and one one-on-one interviews. However, a degree of response bias is likely to persist. An additional limitation is the employment of close-ended survey questions. Close-ended questions are quick and easy to answer and obtain measurable, quantitative data that can be analyzed statistically. However, close-ended questions can also be suggestive and open to misinterpretation. As qualitative feedback from experienced surgeons collected during one-on-one interviews supports survey data, these limitations were likely minimized.
The technical specifications identified through design verification testing are supported by the results of this study. The ArthroFree handheld device weighs 438g; 87.34% of survey respondents agree this weight felt good. Agreement with the statements that the “ArthroFree felt well balanced” (90.91%) and that “the size and weight of the light source wouldn’t inadvertently rotate the arthroscope” (87.50%), support that the size (36 X 69 mm) and weight (135 g) of the light source is acceptable by end users. The maximum light source temperature of 43°C, a key design feature, is “comfortable to touch” (94.25%). Additionally, the light/brightness level (generated with <5W of power) was appropriate (90.91%). Lastly, 88.10% of survey respondents and more than half of the surgeons interviewed agreed that the introduction of the wireless ArthroFree device to arthroscopy will have a positive impact on efficiency in the OR.
CONCLUSION
The development of the ArthroFree device has made wireless endoscopic surgery a reality. Favorable survey scores and benefits expressed by surgeons reflect a positive opinion of ArthroFree’s design. Taken in combination, the results support the usability of the first wireless surgical camera and a high likelihood of user adoption.

_and_arthrofree_(right).jpg)
_and_arthrofree_(right).jpg)