Background
Fractures involving the tibial plafond commonly result from high energy mechanisms and can be difficult to manage when complicated by significant comminution and severe traumatic disruption of the surrounding soft tissue envelope (Mauffrey et al. 2011; Borrelli and Ellis 2002; Sirkin and Sanders 2001). Plafond fractures can be devastating injuries for this reason, and in many cases can result in a permanent change in both limb mechanics and function. These injuries account for 5-7% of all tibial fractures, which in most cases are treated with delayed definitive operative management. The goal of open reduction with internal fixation is to restore anatomic alignment of the joint surface and correct the involved metaphyseal component into a position that preserves mechanical alignment (Mauffrey et al. 2011; Bedi, Le, and Karunakar 2006; “Surgical Treatment of Distal Tibia Fractures: A Comparison of Medial and Lateral Plating” 2009; Topliss, Jackson, and Atkins 2005). Crucial, though, is the management of the soft tissue injury. Current recommendations focus on external stabilization of the plafond temporarily followed by reconstruction with a plate and screw construct once the soft tissue becomes amenable to fixation (Mauffrey et al. 2011). Occasionally, the swelling may be minimal, and in the presence of a positive wrinkle sign, some surgeons will elect for early definitive fixation. Despite advancements in implants and fixation techniques, bony union may prove to be difficult in some patients with poor bone quality or those who develop an infection (Özpolat 2021; Simpson and Tsang 2017; Egol et al. 2009). Septic nonunions are a devastating outcome, requiring subsequent procedures to irrigate and debride all infected tissue in an effort to prevent osteomyelitis (Özpolat 2021; Qiu et al. 2017). If osteomyelitis develops, all involved bone must be removed, often resulting in significant bony voids which can be a very challenging problem to correct (Qiu et al. 2017). Historically, distraction osteogenesis, bone transfer, and cadaver allografts have been used to span this negative space, however, the Masquelet technique (MT) has emerged as an alternative option for reconstruction (Hatashita et al. 2020; Careri et al. 2019; Alain C. Masquelet and Begue 2010).
The MT is a two-stage procedure. The first stage consists of a thorough debridement and placement of a cement spacer. The body will recognize the cement as a foreign body, leading to the formation of a membrane around the cement. The second procedure is performed 4-8 weeks later where the cement is replaced with fresh bone graft while maintaining the pseudomembrane (A.C. Masquelet et al. 2000). Several studies have shown the effectiveness of the MT in the treatment of osteomyelitis (Qiu et al. 2017; Careri et al. 2019; Tong et al. 2017; Morelli et al. 2016). It has since been utilized for the treatment of many long bone fractures with significant bone voids.
To our knowledge, no studies have explored the outcomes of intentional maintenance of the cement spacer following the first stage of the traditional MT or cement augmentation (CA). In previously reported cases, the patients who fail to undergo the second stage are those who have been lost to follow-up or failed treatment requiring amputation (Assal and Stern 2014; A. Masquelet et al. 2019; Karger et al. 2012).
The use of Polymethylmethacrylate (PMMA) cement in fracture augmentation has been a growing topic of interest, with multiple studies demonstrating enhanced fracture stability and positive outcomes (Sune Larsson and Bauer 2002; Bartucci et al. 1985; Kiyoshige, Takagi, and Hamasaki 1997; Muhr, Tscherne, and Thomas 1979; Schatzker, HAʼERI, and Chapman 1978; Goodnough et al. 2021; Oh, Park, and Jo 2017; S. Larsson 2006). Polymethylmethacrylate (PMMA) has been the gold standard for arthroplasty because it can provide lasting multidirectional stability since it is not reabsorbed by the body (Kammerlander et al. 2016; Russell and Leighton 2008). In each of these cases, the cement is left in-place permanently.
The following study describes a case of a successful reconstruction of a septic nonunion tibial plafond fracture utilizing an intentional maintenance of a PMMA antibiotic spacer as definitive treatment.
Case Presentation
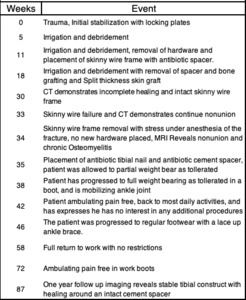
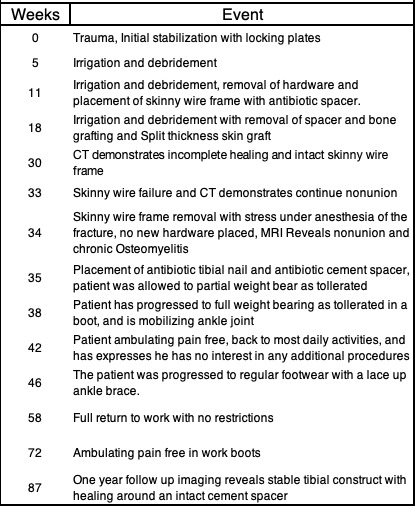
A 51-year-old morbidly obese, non-smoking male with a past medical history of type 2 diabetes, stage 3 chronic kidney disease, hypertension, and a previous gastric bypass surgery presents to the emergency department with a right ankle injury after a ground level fall while intoxicated. Radiographic imaging in the emergency department revealed a comminuted right distal tibial shaft fracture with extension into the tibial plafond, and an associated nondisplaced distal fibular fracture (Figure 1). At the time of orthopedic consult which was less than 24 hours after the initial injury, physical exam revealed the leg neurovascularly intact with no fracture blisters forming on the skin. At that time the soft-tissues were deemed amenable to immediate fixation and the patient was taken the same day for definitive ORIF using a dual locking plate construct (figure 2).
Six weeks later, the patient presented with wound necrosis with abscess formation involving the anterolateral incision (Table 1). The patient was taken back to the operating room for irrigation and debridement (I&D) with wound vac placement. Appropriate antibiotics were determined from the intraoperative cultures that were positive for P. mirabilis, K. oxytoca and E. faecalis. At this point an interdisciplinary team was established for his care, including the infectious disease team who managed his antibiotics, starting him on IV Zosyn for 6 weeks to be followed by Augmentin. Since presented with blood glucose of 194 and 121 for his first two procedures, the medicine team had a meeting with him to discuss possible changes.
Eleven weeks after his initial procedure, repeat radiographic imaging was concerning for minimal healing and he was noted to have persistent drainage from the wound vac.
At this time, care was transferred to a fellowship-trained orthopedic traumatologist as there was concern for deep infection resulting in delayed and compromised fracture healing. Since the patient was still showing clinical signs of infection and no healing observed on films, it was elected to undergo a second irrigation and debridement with removal of hardware and placement of a skinny wire frame external fixator. An excisional debridement of all nonviable bone had been performed at this time. An antibiotic cement spacer mixed with 1.4g gentamicin and 1g vancomycin had been inserted into an extra-articular bone void measuring approximately 3x2x2 cm. While maintaining the midsubstance of the incision open, the edges of the previous incision were closed primarily and a wound vac was placed. Appropriate antibiotics were again determined from the intraoperative cultures, this time positive for C. striatum.
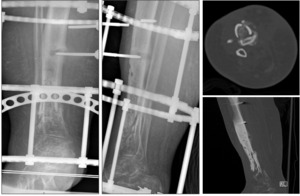
At the eighteen weeks, radiographic imaging continued to show signs of nonunion. There was discussion at this time that the delayed union was in part due to lack of structural support (Figure 3). The decision was made to undergo repeat I&D with removal of cement spacer and bone grafting in an attempt to stimulate union, followed by definitive coverage of the wound with a split thickness skin graft (Figure 4).
At thirty weeks, a CT scan demonstrated incomplete fracture healing with incomplete incorporation of the bone graft (Figure 5). The decision was made to maintain non-weightbearing and the skinny-wire frame to allow continued healing.
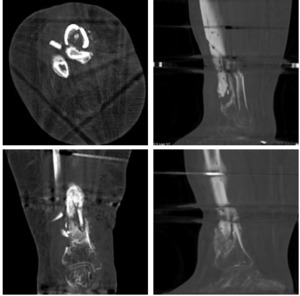
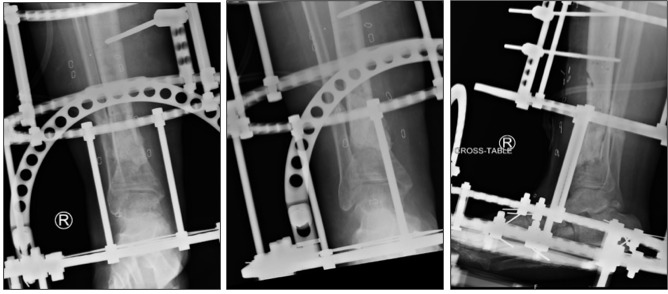
At thirty-three weeks, the patient presented to the emergency department with substantial right lower extremity pain and fevers. Subsequent radiographic imaging revealed he had broken one of the pins on his external fixator (figure 6). The external hardware was subsequently removed the next morning, giving the patient a hardware holiday while the definitive treatment was planned. MRI imaging revealed continued tibial nonunion and chronic osteomyelitis (Figure 7). Approximately one week later, the patient was taken for another I&D with excision of nonviable bone, placement of antibiotic coated tibial intramedullary nail, and placement of antibiotic cement spacer in the remaining tibial void measuring 7x3x3 cm (Figure 8). The patient was allowed partial weight bear postoperatively. Appropriate antibiotics were again determined from the intraoperative cultures by the infectious disease team, and at this time were positive for S. lugdenensis and S. agalactiae. He had made progress controlling his diabetes, as his most recent hemoglobin A1c was 4.5. Discussion with the patient was that this was a limb salvage procedure in an attempt to avoid amputation and that typically the cement spacer needs removal at a future date and replacement with bone graft.
At thirty-eight weeks, four weeks after the most recent surgery, the patient was reported that he was ambulating well in a walking boot and his pain was significantly improving. At this point there was a discussion about the appropriate next steps. The patient was informed that in most situations, the bone cement is removed and replaced with bone graft 1-2 months after placement. While the antibiotic cement spacer allows for slow elution of antibiotics, it is not traditionally intended to provide permanent structural support.
At forty-two weeks, eight weeks after the most recent surgery, the patient had felt his best since the initial trauma, reporting that he had no pain as he ambulates full weight bearing in a boot, and that his activity level had returned close to his normal baseline. At this time, the patient was not interested in any additional surgeries, and elected to postpone the second procedure with plans to exchange the cement for bone graft only if needed.
By eighty-seven weeks, one year after the most recent surgery, the patient is ambulating pain free in his regular work boots without assistive devices, has fully returned to work as a physical laborer, and reports he is completely back to his normal life. Most recent radiographic images demonstrate a stable tibial construct with healing of the ¾ cortices surrounding an intact cement spacer (Figure 9).
Discussion
Since it was first described in 2000, the Masquelet technique has been successfully implemented and utilized for the management of long bone fractures with large bone voids. Following the original publication, literature has demonstrated an overall success rate of 86% (478/554 defects) for the MT18. This two-stage approach is similar for cement augmentation used for smaller defects, and the end result of replacing cement with bone graft is the same for each technique. The case presented highlights an adaptation of the traditional two stage approach. The patient achieved a functionally stable and mechanically appropriate lower extremity that was infection and pain free, without the need to undergo an additional procedure to remove the cement spacer and replacement with bone graft.
Authors have shown the adaptability of the MT to be used for other indications beyond its traditional use. Hatashita et al showcased the ability to use the MT in the acute setting, demonstrating its success in the treatment of seven patients in Japan with open tibial shaft fractures (Hatashita et al. 2020). Khaled et al combined the Masquelet and Ilizarov techniques in thirty-two patients in Egypt with septic tibial nonunion, and they found that 94% (30/32) of cases had a successful reconstruction with no recurrence of the infection (Khaled, El-Gebaly, and El-Rosasy 2022). Qui et al compared the usage of a cement spacer vs cement beads in the MT for forty patients in China with post traumatic osteomyelitis. Their results showed no difference between antibiotic spacer and antibiotic beads. Ultimately concluding that antibiotic cement spacers in the MT are an effective method of infection control for post traumatic osteomyelitis (Qiu et al. 2017). To date, no study has shown a clear correlation between an increased procedure interval in the MT and worsening outcomes (Alford et al. 2021). Assal et al demonstrated a successful Masquelet second stage 8 years after the placement of the antibiotic spacer (Assal and Stern 2014).
The case here presented involved a 51-year-old morbidly obese male with medication controlled Type 2 Diabetes Mellitus who presented with a severely comminuted distal tibial shaft fracture with extension into the tibial plafond. The mechanism of injury was a low energy fall from a ground level fall while intoxicated, however, the fracture pattern demonstrated a bony response that more closely resembled injury from a higher energy mechanism with significant comminution and intraarticular extension. Given the degree of injury, the approach to the patient was initial operative stabilization. The patient presented to the emergency department on and was taken to the operating room the same evening. As is the case with all pilon fractures, the patient’s immediate soft swelling was significant, but likely in part masked by chronic bilateral lower extremity edema for which he was on 40mg of lasix daily. The approach to fracture stabilization required utmost respect for the soft tissue envelope involved, however due to the lack of an appreciable difference in the degree of swelling relative to the contralateral extremity, the decision was made to undergo definitive open reduction with internal fixation. Care was taken to avoid extensive soft tissue stripping throughout the procedure, however, In the context of the patient’s medical comorbidities and the immediacy of his injury, temporary stabilization with an external fixation during the index procedure may have been warranted to allow soft tissue healing and provide a more receptive environment for definitive fixation. Perhaps this may have reduced his risk of soft tissue complications after the initial surgery. Additionally, perioperative optimization could have been a focus to try to reduce complications. Preoperative optimization is difficult in the setting of traumatic fractures. Postoperatively, though, a focus on improved nutrition and alcohol/tobacco cessation may have been a worthwhile conversation with all providers involved in his care, given the social history, medical comorbidities and health status, and subsequent events that resulted in his traumatic injury.
The patient’s specific case highlights the use of an antibiotic cement spacer in combination with a tibial nail to augment fixation of a tibial plafond fracture nonunion. The unique aspect of this case, however, is the retention of the cement spacer as definitive treatment without planned removal of the cement and bone grafting the void. We believe both the tibial nail and the cement both provide structural and weight bearing stability with minimal evidence of radiographic or clinical change at one year postoperatively. Four weeks after the procedure, the patient was able to bear full weight on the extremity in a boot, and returned to work with no restrictions by twenty-three weeks. He has returned to all normal activities, ambulating pain free, without ever having to have undergone the second stage procedure. At this time, his imaging demonstrated bony bridging of ¾ cortices, which aligns with many publications that use bridging of 50% or 2 cortices as the standard for healed 32-34. This case, combined with the studies presented above, suggest that as a variation of cement augmentation or the Masquelet technique, a tibial nail could be inserted with the cement spacer in the first stage as an appropriate definitive fixation, and the second stage could be postponed indefinitely or performed years later if deemed necessary.
Conclusion
The Masquelet technique and cement augmentation have consistently been shown to be a successful option in the treatment of nonunion and bony voids. The technique is a multiple staged procedure with a lengthy recovery period. This case demonstrated successful variation of these techniques. The addition of the tibial nail in the first stage of our case allows for greater initial stabilization and would allow for a longer interval between the first and second stage procedures. With documented success of the Masquelet second stage years after the first procedure, we believe this variation adds stability to CA or MT, allowing it to be performed as a one stage procedure with the option to replace the cement with bone graft at any point in the future if needed.