Introduction
A bucket handle tear is a type of meniscus tear that usually occurs in the medial knee compartment. The medial meniscus is a more rigid crescent-shaped piece of fibrocartilage that acts as a shock absorber and secondary stabilizer in the knee joint (Fox, Bedi, and Rodeo 2011).
Bucket handle tears can be caused by a sudden twisting or pivoting motion of the knee, such as might occur during sports or a fall. They can also happen in the background of advanced degenerative arthritis, which can occasionally cause gradual meniscus tearing with a bucket handle configuration (Wright et al. 2010).
Symptoms of a bucket handle tear can include pain, swelling, and locking of the knee. The pain is typically worse when the knee is bent or twisted. Swelling can occur in the knee joint. Locking of the knee occurs when the torn piece of meniscus gets caught in the intercondylar notch, preventing the knee from bending but mostly from completely extending (Raj and Bubnis 2022).
Treatment for a bucket handle tear depends on the severity of the tear and the patient’s age and activity level. In some cases, the tear can be treated with nonsurgical means, if there are no mechanical symptoms mainly in older or low-demand individuals. However, In most other scenarios, surgery may be necessary to repair the tear as a joint-conserving measure or to resect it in salvage situations (Doral et al. 2018).
The two most common types of surgery for bucket handle tears are arthroscopic surgery and open surgery or a combination of both.
Arthroscopic Surgery
Arthroscopic surgery is a minimally invasive procedure that is performed through small incisions in the knee. The surgeon establishes access to the joint through a viewing portal and performs the procedure through a working portal. Arthroscopic surgery is usually the preferred option for bucket handle tears because it is less invasive and has a shorter recovery time than open surgery.
Open Surgery
Open surgery is a more invasive procedure that is performed through a larger incision in the knee. The surgeon repairs the tear directly. Initially, this technique was considered the gold standard of meniscus repair. However, with the evolution of arthroscopic techniques and meniscal suture devices, the solely open technique is falling out of favor in sports medicine.
Combined Arthroscopic and Open surgery
The surgeon can combine both techniques to have the ability to tie knots over an extracapsular approach either in an inside-out or outside-in fashion.
CASE PRESENTATION
A 17-year-old male presented to our office with his mother, complaining of right knee pain and difficulty walking. The patient reported hearing a pop in his knee while taking out the trash, which was followed by sudden onset pain and difficulty bearing weight on the affected leg. The patient is an avid basketball player with no significant medical or surgical history. The family history was negative for any musculoskeletal disorders.
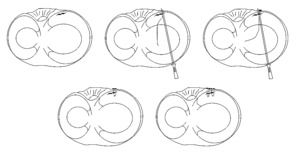
On examination, there was tenderness over the medial joint line, slight effusion of the knee, and limited range of motion from 20 to 110 degrees due to painful mechanical endpoints. Positive Mcmurray and Thessaly tests were also noted. There were no signs of neurovascular compromise. The patient was diagnosed with a bucket-handle tear of the medial meniscus. MRI findings confirmed the presence of a bucket-handle medial meniscus tear with complete displacement into the notch. (Fig. 1).
The patient was counseled about the diagnosis implications and the possible treatment options. In this case, due to his young age and the potential for long-term complications of conservative treatment, including loss of the protective function of the medial meniscus with resultant early-onset osteoarthritis, he was recommended to undergo arthroscopic surgery with meniscus repair (Weber et al. 2018).
Surgical technique
Diagnostic arthroscopic examination
The patient was brought to the operating room and given general endotracheal anesthesia in the supine position with all his bony prominences padded. Preoperative antibiotics were administered, and the right lower extremity was prepped and draped. A time-out was conducted by the staff to confirm the correct patient, procedure, and site.
The surgeon made a 1 cm incision on both sides of the patellar tendon starting with a diagnostic arthroscopy. As expected from the clinical examination and the MRI, the meniscus tear extended from the posterior horn to the body and part of the anterior horn, the torn part was flipped and trapped in the intercondylar notch (Fig2). There was as well fraying of the medial femoral condyle articular surface. The lateral meniscus was observed to be in good shape. The meniscus tear was assessed for size, location, chronicity, and pattern.
The anterior cruciate ligament (ACL) was found to be intact, and so was the patellofemoral compartment
The surgeon proceeded to successfully reduce the bucket-handle meniscus tear in extension.
Passage of inside-out sutures
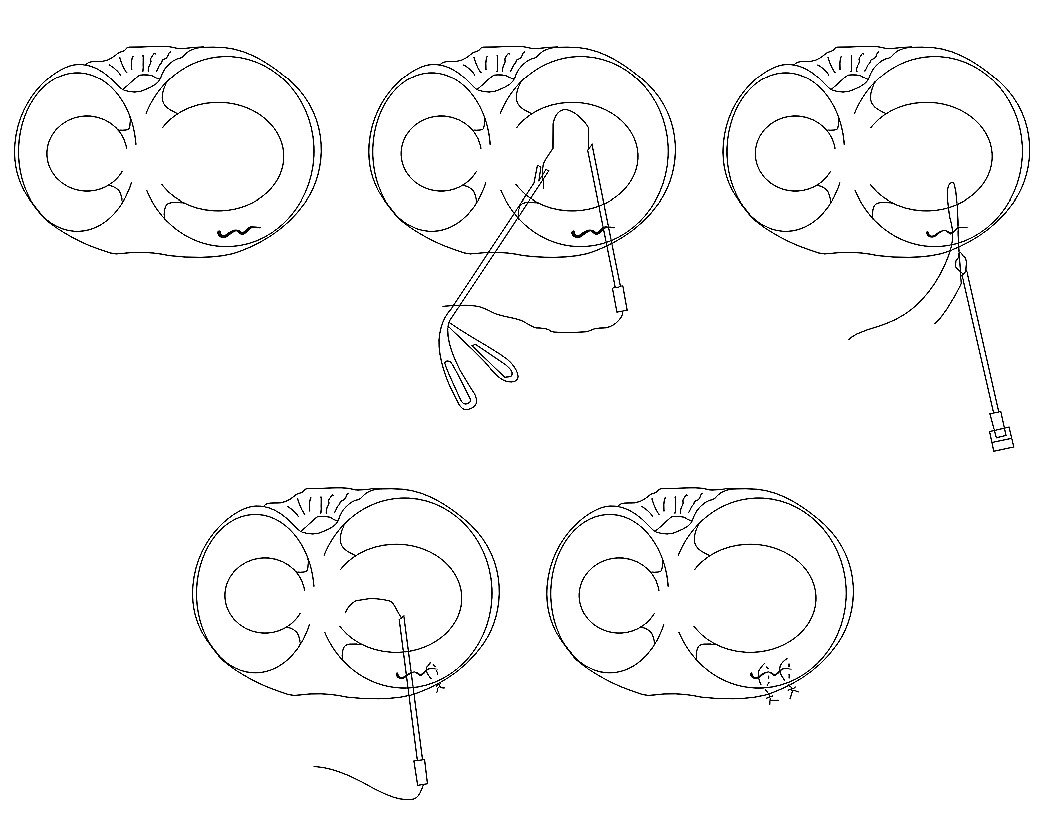
The surgeon established a medial vertical incision posterior to the medial collateral ligament. Subsequently, subcutaneous dissection was carried out until the medial retinaculum of the knee was reached, which was then opened. The gastrocnemius was retracted posteriorly, the pes anserine anteriorly, and the posterior capsule was identified using a Hennig retractor. The surgeon then resumed the arthroscopy and secured seven inside-out 2-0 FiberWire sutures switching between medial and lateral working portals depending on the angle of approach. The working sequence started from the posterior horn to the body with 5 inside-out sutures and then part of the anterior horn was repaired using 2 of the same flexible needle sutures devices in a modified outside-in technique. In fact, at the junction of the body and the anterior horn, or as we can call it in this article “the anterior corner”, it was difficult to achieve the desired angle through an inside-out approach hence the need to resort to the above mentioned modified outside-in approach that will be described in the following paragraph (Chahla et al. 2016).
Passage of outside in sutures
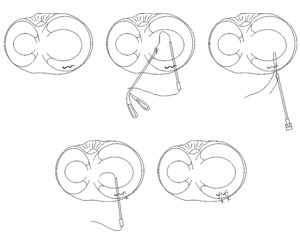
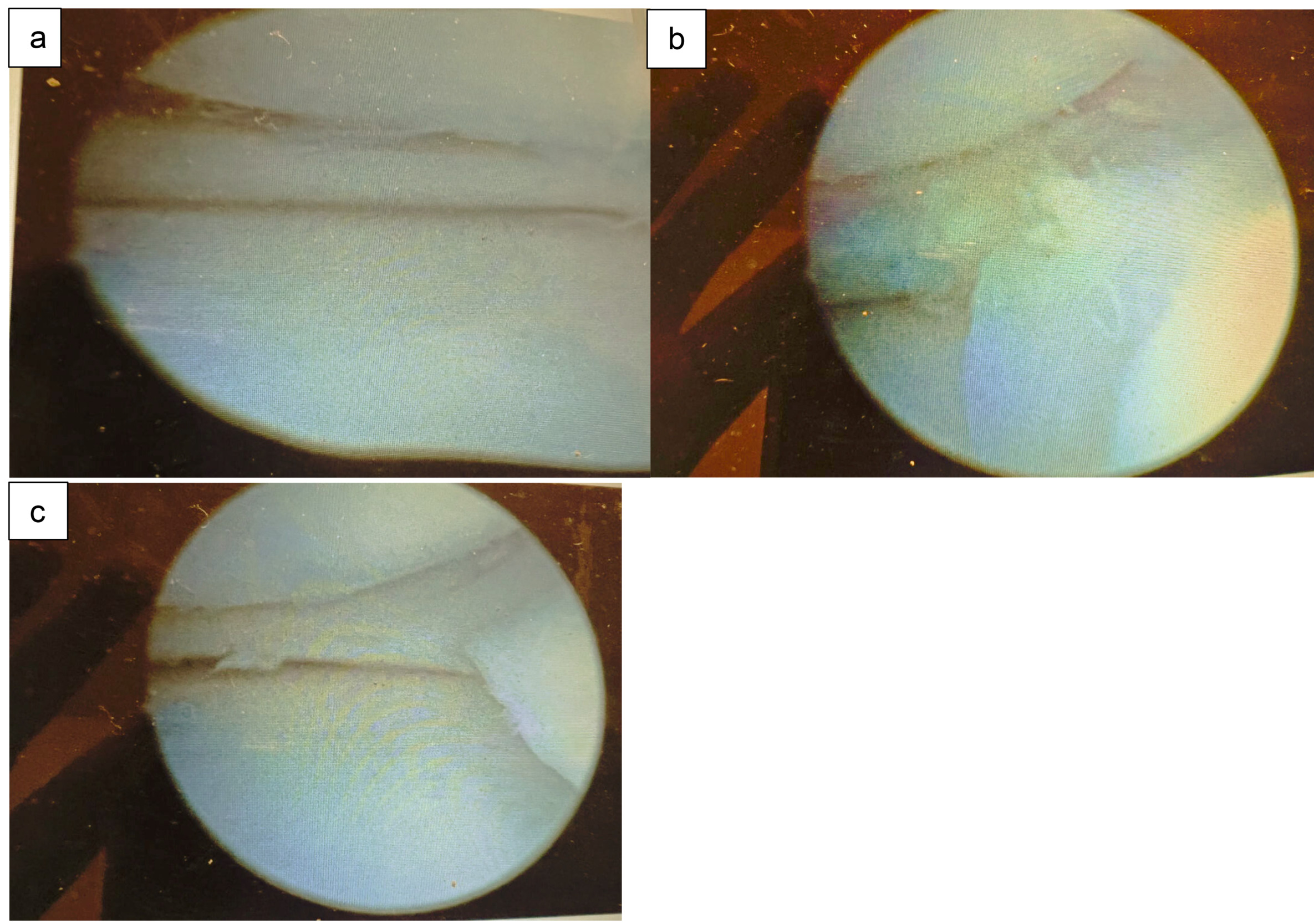
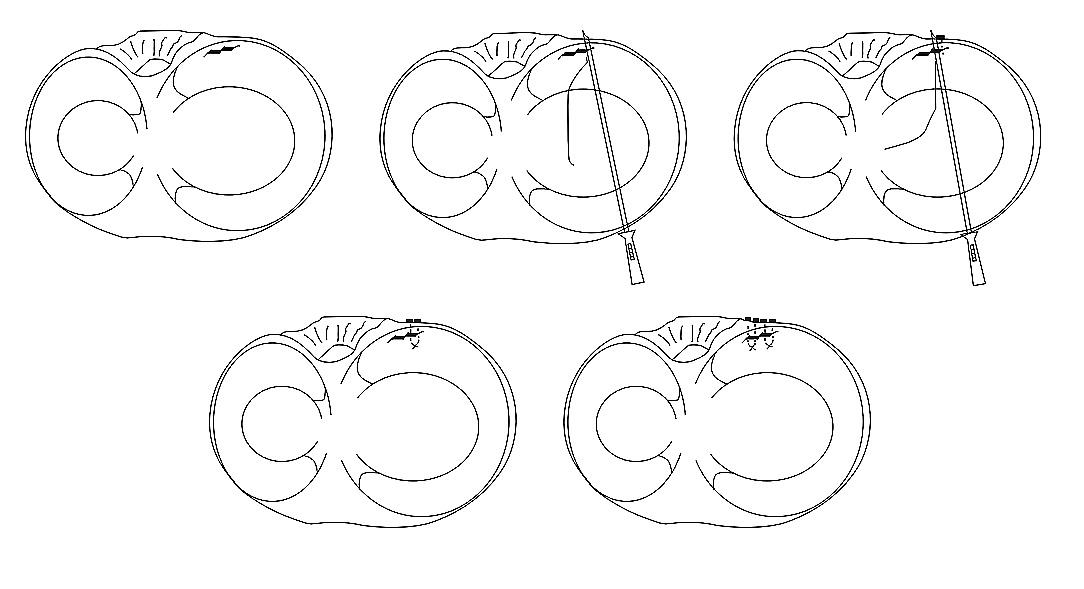
As indicated, the junction of the body and the anterior horn, or the anterior corner, was repaired using modified outside-in sutures through a novel technique. This method was done by cutting the inside-out needles short at an angle to provide a sharp end to the tip(P1). We then introduced the needles with specific angle of approach in an outside-in fashion(P2) and then we retrieved them using an arthroscopic grasper from within the joint(P3). The needles were cut off to tension the sutures and tie them using a knot pusher(P4). In addition to the inside-out and the outside-in sutures, 4 all-inside sutures were used to supplement the repair and provide better stability and reapproximation of the meniscus. (Fig. 3).
Patient follow up
At the 2-week follow-up, the patient was doing well, and the incision had completely healed. He had regained full range of motion and reported no pain or discomfort. The patient was advised to continue with his physical therapy program and to gradually increase his activities as tolerated.
At 6 weeks, he was ambulating with no assistive device, his range of motion normalized, and he was working with physical therapy on strengthening and regaining muscle control. The last follow up with the patient was at 4 months after surgery. He was pain free. He returned to work, to jogging, and to his gym workout routine. He still needs to work on his quadriceps strength. He is anticipating full return to sports at 6 months post-op.
DISCUSSION
To our knowledge, this is the first report of this new technique for repairing bucket handle medial meniscus tears. The medial meniscus anterior corner is a challenging area to repair arthroscopically. The traditional inside-out and all-inside techniques have been described, but they can be technically demanding with difficult access to certain parts of the meniscus namely the anterior corner and anterior horn. We have developed a new technique for medial meniscus anterior corner repair that is simple, reproducible, and provides secure fixation.
Inside-out meniscal repair
The inside-out repair technique is a surgical approach used to repair meniscal tears. It involves specific steps:
-
Patient Positioning: The patient is placed in the supine position on the operating table, and a tourniquet is applied to the operative knee.
-
Portal Creation: Two portals, the anterolateral and anteromedial, are created for arthroscopic access to the knee joint.
-
Posterolateral Approach: An incision is made over the lateral joint line, following the iliotibial band’s posterior border. Blunt dissection is performed to release adhesions between the lateral gastrocnemius and posterior capsule. A retractor, such as a metal spoon, is inserted to protect the neurovascular bundle.
-
Posteromedial Approach: An oblique vertical incision is made from the adductor tubercle to the posterior aspect of the tibial plateau. Careful dissection is performed to separate the posteromedial joint capsule from adhesions to the medial gastrocnemius complex. A retractor is placed to protect the popliteal vessels.
-
Meniscal Suture: The size, stability, and type of the meniscus tear are evaluated. Using a self-delivery gun with a cannula, double-loaded nonabsorbable sutures are passed into the meniscus. The sutures are placed perpendicular to the tear to restore its anatomical position. Care is taken not to overtighten the tissue during suturing.
The inside-out repair technique allows for precise placement of sutures within the meniscus, providing a strong and stable repair. It is beneficial for larger or complex meniscal tears.
All-inside meniscal repair
The all-inside meniscal repair technique involves the use of a specialized repair device, such as the FastFix 360 All-Inside Meniscal Repair System. The procedure includes the following steps:
-
Preparation: The repair site is prepared, and an arthroscopic probe is inserted through an accessory portal as a guide.
-
Device Insertion: The repair device is inserted through the anterior portal and directed to the site of fixation. The probe helps manipulate the meniscal tissue and ensures perpendicular entry of the device.
-
Meniscal Reduction: The device is used to reduce the meniscus to its original position, facilitating proper alignment for repair.
-
Anchor Deployment: Anchors are deployed to secure the repair. The device is guided around the condyle to position the anchors for vertical mattress sutures on the superior or undersurface of the meniscus.
-
Suture Tightening: The sutures are tightened, ensuring appropriate tension for stable fixation. The probe is used within the adjustable loop of the sutures to protect them from cutting through the meniscal tissue during tightening.
-
Finalization: Once the fixation is secure, the sutures are cut. Sequential superior and undersurface mattress sutures are added to suture the meniscus posteriorly to anteriorly, restoring its normal position and the meniscal flounce sign.
The all-inside technique offers the advantages of minimally invasive repair and precise fixation. It reduces the risk of damage to surrounding structures and promotes faster recovery.
Outside-in meniscal repair
The outside-in repair technique is commonly used for repairing anterior horn tears in the meniscus. The procedure involves the following steps:
-
Diagnostic Arthroscopy: A thorough evaluation of the meniscal pathology and concurrent issues is performed using arthroscopy.
-
Incision and Dissection: An incision is made on the same side of the knee as the tear, aligned with the portal. Careful dissection is performed to expose the underlying anterior joint capsule.
-
Needle Insertion: A spinal needle is inserted through the capsule, under the anterior edge of the meniscus, and through the body of the anterior horn, crossing the torn area.
-
Suture Placement: The inner cannula of the needle is removed, and a PDS suture is placed through the needle and into the joint. A second needle is passed through the capsule, underneath the meniscus, and through the body of the anterior horn. The inner cannula of this needle is also removed, and a looped suture retriever is passed through it into the joint. The free end of the previously passed suture is pulled through the looped retriever, creating a mattress suture construct to secure the anterior horn.
-
Reinforcement and Stability: Additional sutures may be added to reinforce the repair, using horizontal or vertical mattress suture configurations based on the tear’s nature. The sutures are tied to the anteromedial or anterolateral capsule with the knee flexed to 90°. Arthroscopy is performed to confirm the stability of the repair.
The outside-in repair technique provides reliable and effective treatment for anterior horn meniscal tears. It ensures stable fixation and optimal healing of the meniscus. Postoperative rehabilitation and care are crucial for successful outcomes.
Our technique does not require the use of spinal needles or PDS sutures. If used along with inside-out sutures, it does not require an accessory skin incision, which can be more morbid.
The technique helps in optimizing access to a difficult zone of the meniscus during the procedure. Namely the anterior corner which was augmented using a modified outside-in approach. Two flexible needle devices were cut short, introduced in an outside-in fashion, and retrieved through the arthroscopic portals using an arthroscopic grasper, the needles were then discarded, and the sutures were tied using a knot pusher.
In our opinion, this modification facilitates a surgeon’s inventory and workflow in a difficult meniscus case especially if it is combined with ligamentous or cartilage work.
This procedure is similar to the traditional outside-in repair technique, but it does not require the use of spinal needles, neither resorts to suture passage nor adds accessory incisions.
The inside-out needles are affordable however there is even a possibility to consult with industry professionals to manufacture shorter more rigid needles that could be used for this novel technical implementation.
Technique Limitations
This technique requires an open accessory incision for implementation.
In our case, we were able to use the same incision designed initially for an inside-out technique. The indications are usually for extensive tears including bucket handle ones. If a tear is limited to the anterior corner, the technique can be done, but we must create a dedicated incision to do it, which some surgeons consider more invasive. Otherwise, a traditional outside-in or an all inside can be entertained instead.
The other limitation is the difficulty in using the typical posteromedial incision for an anterior corner repair in obese or overweight individuals. Typically, it works well for an athletic build however it becomes more challenging to do it in larger individuals and even in certain athletes like football linemen.
Conclusions
In this particular case, a 17-year-old male presented with a bucket-handle tear of the medial meniscus. To address this, the patient underwent arthroscopic surgery with meniscus repair. During the procedure, the surgeon performed an inside-out repair for the posterior horn and body of the meniscus but faced difficulty accessing the anterior corner and horn.
To overcome this challenge, the surgeon improvised and came up with the idea of using an outside-in repair technique using the same incision. Instead of using spinal needles, the surgeon used the same long (inside-out) needles after cutting them short. This innovative approach allowed the surgeon to tension the repair from within the knee and thus obtained the desired result after meniscus healing.