Introduction
Rugby is one of the most popular sports in the world, boasting 405 million fans across 85 countries, with popularity increasing by 18% between 2018 and 2019. The sport is physically demanding, with frequent periods of high-intensity activity such as sprinting and tackling at high speeds being integral to match play (Williams et al. 2013). This exposure to high impacts, often amplified at elite professional levels, has resulted in rugby having one of the highest reported incidences of injury at the professional level even amongst contact sports, with rates higher than American Football (Willigenburg et al. 2016). Lower limb injuries are particularly common, with meta-analysis and prospective cohort studies documenting high rates of occurrence (Williams et al. 2017, 2013; Toohey et al. 2017).
Previous studies, such as Viviers et al., have demonstrated that rugby players often incur multiple injuries precluding them from match participation, with some studies such as Moore et al. differentiating recurrent injuries (same site, same type as index injury) from other subsequent injuries (different site and/or different type compared to index injury) (Moore et al. 2017; Viviers, Viljoen, and Derman 2018). Moore et al. specifically noted variations in the frequency of recurrent injury compared to subsequent injury (Moore et al. 2017). Sustaining multiple secondary injuries has been shown to have negative consequences on continued participation in sport in elite professional athletes across multiple disciplines, emphasizing a greater need for improved risk stratification for both recurrent and subsequent injury (Williams et al. 2017).
A prospective cohort study by Williams et al. quantified subsequent injuries and categorized them based on both type and risk to the player, finding lower limb injuries were the most common type of subsequent injury and neck muscle strains, ankle joint capsule strains, and cervical nerve root injuries carried the greatest risk of harmful effects (Williams et al. 2017). The authors also documented that injury recurrence was most likely to occur within two months of play. However, no studies to date have differentiated the overall risk of subsequent injuries compared to recurrent injuries, nor have they collated data regarding secondary injuries following specific types of index injury.
An understanding of the incidence and etiology of injury is an integral part of injury prevention (MacQueen and Dexter 2010). To that end, the purpose of this study was to review and collate epidemiological data specific to recurrent and subsequent injuries in male amateur/professional rugby players world-wide, assessing risk of injury both overall and following specific types of index injuries in an effort to identify risk factors.
Methods
This study was performed following the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) checklist, a 27-item checklist which specifies criteria for reporting including background, search strategy, methods, results, and conclusions (Liberati et al. 2009).
Literature Search
PubMed, CINAHL plus, Embase, and Web of Science databases were searched from January 1, 1974 through October 1, 2020. Keywords used were ((“Football” [Mesh].) OR (rugby)) AND ((recurrent injury) OR (subsequent injury)) in PubMed, (‘rugby’/exp OR rugby) AND (recurrent AND (‘injury’/exp OR injury) OR subsequent) AND (‘injury’/exp OR injury) in Embase, rugby AND (subsequent injury OR recurrent injury) in CINAHL Plus, and TOPIC: (rugby) AND TOPIC: (subsequent injur* OR recurrent injur*) in Web of Science. Search terms were chosen according to database specificities and to maximize search results. Two co-authors independently performed the database search. Following the initial search, abstracts and titles were screened to identify studies that discussed rugby injuries. Those studies were selected for full text review.
Studies were included if they met the following criteria: (i) study population consisted of male rugby players; (ii) study used “time-loss” as an injury definition—i.e., only injuries that resulted in a player missing games or practice were quantified; (iii) study included data on both subsequent injury count and recurrent injury count or provided sufficient information to extrapolate that data; (iv) study was written in English. Exclusion criteria was based primarily on the type of study—meta-analyses, systematic reviews, case reports and case series were excluded from consideration, but sources used in meta-analyses and reviews returned by the search were investigated for potential inclusion. Unpublished studies were not considered.
Assessment of Study Quality
Study quality was assessed independently by two reviewers using the “Strengthening the Reporting of Observational Studies in Epidemiology” (STROBE) statement (von Elm et al. 2014). Studies were categorized based on the percentages of fulfilled items from the 22-item STROBE checklist, with values of <50, 50–80, and >80% indicating poor, moderate, or good, respectively, as per Olmos et al (Olmos et al. 2008).
Data Extraction
Studies that met inclusion criteria were assessed for level of play, number of players involved, total injury count, and number of incidences of recurrent injury. Rates of total, subsequent, and recurrent injuries overall, and data regarding count and rates of injury following specific index injuries, were recorded when available. As the definition of subsequent injury was not consistent between papers, reviewers defined a subsequent injury as any injury following an initial injury that was not recurrent (same site and type of injury). For the purposes of this paper, recurrent injuries were considered separate from subsequent injuries for comparison (i.e., if a paper listed recurrent injuries as a subcategory of subsequent injuries, recurrent injuries were subtracted from the total number of injuries).
Data Analysis
Following data extraction, studies were divided into an adult group (age 18+) and a pediatric group (ages 0–18), as one study by Archbold et al. focused solely on pediatric patients, while another study by Garraway et al. differentiated pediatric and adult populations (Archbold et al. 2018; Garraway and Macleod 1995). Injury proportions were calculated for both recurrent and subsequent injuries. Injury incidence risk—defined as the number of injuries divided by the total number of players in one season—was also calculated for index, recurrent, and subsequent injuries to provide an overall representation of the likelihood of a player incurring a specific type of injury over the course of one season. For each group, the difference between incidences of subsequent and recurrent injuries was then compared for significance using 95% confidence intervals (CI).
Results
Database searches returned 1,242 studies containing searched keywords. The search process was then continued through PRISMA guidelines, illustrated in figure 1.
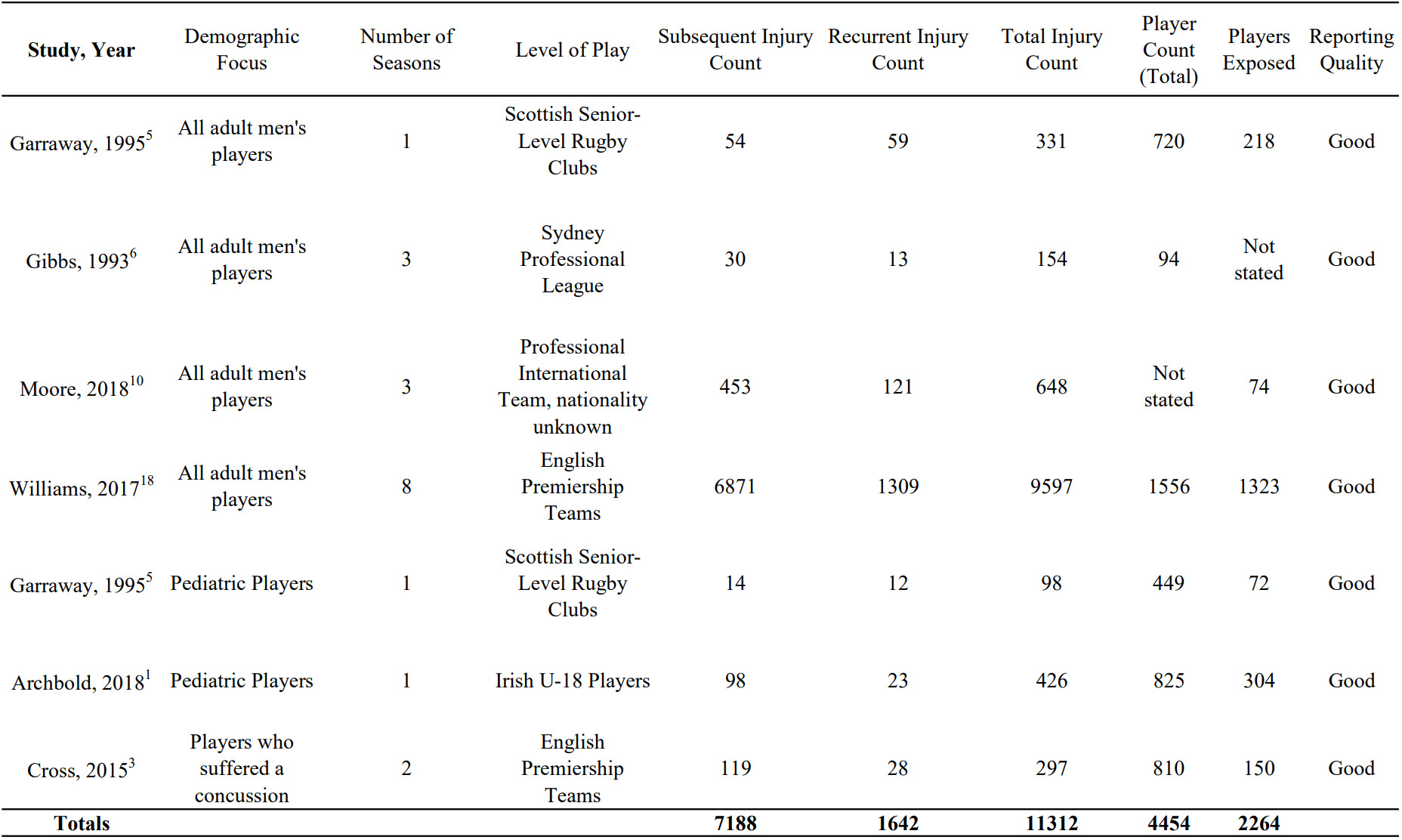
Of these, 319 were excluded as duplicates, leaving 923 studies. 162 of the 923 studies (17.6%) were selected after title and abstract screening. Following exclusion and inclusion criteria, 6 studies (0.65%) were selected for review (Table 1). Of the included articles, 5 (0.54%) discussed overall injury epidemiology, with subject groups consisting of adult males only (3) (0.33%), adult and pediatric males (1) (0.1%), and pediatric males only (1) (0.1%) (Archbold et al. 2018; Garraway and Macleod 1995; Gibbs 1993; Moore et al. 2017; Cross et al. 2015; Williams et al. 2017). One study (0.1%) by Cross et al. evaluated recurrent and subsequent injuries related to concussions as index injuries (Cross et al. 2015).
Using “time-loss” as an injury definition allowed a larger selection of studies, but yielded two separate subcategories of time-loss injuries. In adult players, Garraway et al. and Gibbs et al. defined time-loss injuries as those that resulted in a player missing a subsequent match or at least a full week of training exercises, while Moore et al. and Williams et al. defined time-loss as missing at least 24 hours of rugby training/matches (Garraway and Macleod 1995; Gibbs 1993; Moore et al. 2017; Williams et al. 2017). Archbold et al. evaluated the risk of injuries in pediatric players in 28 Irish schools using the 24-hour injury definition to quantify injuries (Archbold et al. 2018). Cross et al. documented recurrent and subsequent injuries following concussions as the sole index injury in English premiership teams, also using the 24-hour injury definition (Cross et al. 2015).
Adults
All four studies evaluating adult male rugby players provided sufficient data to calculate subsequent and recurrent injuries as proportions of total injuries (Garraway and Macleod 1995; Gibbs 1993; Moore et al. 2017; Williams et al. 2017). Data from studies using similar definitions of time-loss injury were combined—i.e., data from Garraway et al. and Gibbs et al. were combined and data from Moore et al. and Williams et al. were combined. The two studies that used the “missed-match” definition of injury reported 485 total injuries, meaning only injuries resulting in at least 1 missed match were quantified (Garraway and Macleod 1995; Gibbs 1993). In these studies, the proportion of subsequent injuries as a function of total injuries was 17% (95% CI: 0.14–0.21), while that of recurrent injuries was 15% (95% CI: 0.12–0.18), with no significant difference between the two (Gibbs 1993; Garraway and Macleod 1995). When 24-hours was used as a threshold for time-loss—i.e., an injury was quantified if it resulted in at least 24 hours away from any team-related activity—the proportion of subsequent injuries as a function of total injuries increased relative to recurrent injuries (Moore et al. 2017; Williams et al. 2017). Of the 10,245 total injuries reported by the 2017 and 2018 studies, 71% were subsequent (95% CI: 0.71–0.72), while 14% were recurrent (95% CI: 0.13–0.15) (Williams et al. 2017; Moore et al. 2017).
Pediatrics
Subsequent and recurrent injury proportions were also calculated for rugby players <18 years old. The two studies concerning pediatric players showed a similar trend to that of adult players, but with a smaller discrepancy between the two different injury definitions. The study using the 24-hour injury definition by Archbold et al. reported 426 total injures, where 23% were subsequent (95% CI: 0.19–0.27) and 5% were recurrent (95% CI: 0.03–0.08), while the study using the missed-match definition by Garraway et al. reported 98 total injuries, of which 14% were subsequent (95% CI: 0.07–0.21) and 12% were recurrent (95% CI: 0.06–0.19) (Archbold et al. 2018; Garraway and Macleod 1995; Willigenburg et al. 2016).
Concussions
Cross et al. followed professional rugby union players for two seasons to investigate concussion incidence (Cross et al. 2015). They reported subsequent and recurrent injury data focusing on concussions as an index injury, using 24-hours as the definition of time loss. Of 297 total injuries incurred by 810 players over 2 seasons, 40% (119/297) (95% CI: 0.34–0.46) were subsequent injuries other than a concussion and 9% (28/297) (95% CI: 0.06–0.13) represented recurrent concussions (Cross et al. 2015).
Incidence Risk
Adults
Given that the two studies using a 24-hour time-loss definition had such high occurrences of injury (incidence proportion >100%) due to a less stringent definition, only the two studies using missed matches as a time-loss definition provided meaningful data regarding incidence risk (Garraway and Macleod 1995; Gibbs 1993). The Gibbs et al. paper followed players for three seasons, and sufficient data was provided to calculate the number of injuries and number of players per season (Garraway and Macleod 1995; Gibbs 1993). Incidence risk was 40% for index injuries (determined as a function of player count), 22% (95% CI: 0.17–0.26) for recurrent injuries, and 26% (95% CI: 0.21–0.30) for subsequent injuries. These two studies also included total injury rates, with 485 total injuries among 814 total players exposed to 19,704 hours of match/training time corresponding to a one-season injury risk of 46% and a rate of 21 injuries per 1000 player-hours (Table 2) (Garraway and Macleod 1995; Gibbs 1993).
Pediatrics
Both studies with data on pediatric players were used to calculate incidence risk separately. For the Garraway et al. paper defining injury as an event causing the player to miss at least one match, incidence risk was calculated to be 16% (95% CI: 0.13–0.19) for index injuries, 17% (95% CI: 0.08–0.25) for recurrent injuries, and 19% (95% CI: 0.10–0.29) for subsequent injuries (Garraway and Macleod 1995). When using the 24-hour definition of time-loss, incidence risk was calculated to be 37% for index injuries, 8% (95% CI: 0.05–0.11) for recurrent injuries, and 32% (95% CI: 0.27–0.37) for subsequent injuries (Table 3) (Archbold et al. 2018).
Concussions
Reporting incidence proportion/risk using total injuries from the concussion-index study provides an incomplete estimate of risk as only subsequent/recurrent injuries following a previous concussion were recorded. However, an estimate of secondary injury risk was calculated by combining subsequent and recurrent injuries and dividing by the number of index injuries. Among 150 players exposed (i.e., players returning after a concussion), 147 (119 subsequent, 28 recurrent) subsequent/recurrent injuries were incurred corresponding to a secondary injury risk of 98% (95% CI: 0.96–1.00), with a subsequent injury risk of 79% (95% CI: 0.73–0.86) and a recurrent injury risk of 19% (95% CI: 0.12–0.25).
Discussion
This meta-analysis demonstrated the overall incidence of subsequent injury in adult and pediatric male rugby players to be significantly higher than recurrent injury when the threshold for quantifying an injury was 24 hours away from team related activity. Results varied depending on the definition of injury used. Studies using the 24-hour threshold definition reported a 57% difference between subsequent and recurrent injury (Moore et al. 2017; Williams et al. 2017). On the other hand, studies using the “missed-match definition” demonstrated only a 2% difference between subsequent and recurrent injury (Garraway and Macleod 1995; Gibbs 1993). With the missed-match definition, an injury sustained during practice the day before the match would be counted, but an injury sustained resulting in lost practice time but not missed matches would not be counted. The discrepancy between subsequent injury results may therefore be due to severity—more severe injuries resulting in more time lost would be quantified by all studies, but minor injuries resulting in one day of missed practice would only be quantified by studies using the 24-hour threshold. The relatively similar recurrent injury rates between the two definitions—14% for 24-hours, 15% for match loss—suggests that the severity of recurrent injuries is less variable than subsequent injuries, and when recurrent injuries occur, they are more likely to result in more time away from team activity.
Pediatric players had a similar trend to their adult counterparts: subsequent injuries had a higher incidence compared to recurrent injuries using the 24-hour definition of time loss, with no difference when using the match-loss definition. Notably, when using the missed-match definition of injury, there were similar incidences of subsequent (17% vs. 14% in adult and pediatric players, respectively) and recurrent injury (15% vs. 12%, respectively) when compared to adult players, suggesting that more severe injuries resulting in increased time off have similar incidence rates among adult and pediatric rugby players. There was a large discrepancy between subsequent injury rates in pediatric players and adults when considering the 24-hour definition of injury—71% for adults, and 23% for pediatric players, which may suggest that children may suffer fewer minor subsequent injuries than adults.
Cross et al. evaluated the risk of subsequent injuries in male adult rugby players who sustained a concussion over 2 seasons of professional play (Cross et al. 2015). Rugby players with a concussion as an index injury had a subsequent injury incidence risk of 79% (95% CI: 0.34–0.46), significantly higher than the 26% (95% CI: 0.21–0.30) incidence risk for all forms of index injury. The incidence risk of a repeat concussion was 19% (95% CI: 0.12–0.15), which was lower than the incidence risk of recurrence across all types of index injury (22%; 95% CI: 0.17–0.26). These data suggest that concussions in rugby players impact the risk of subsequent injury to a larger extent than other index injuries, and that subsequent injury following a concussion may be more of a risk than sustaining a recurrent concussion.
Many factors may contribute to the increase in subsequent injuries seen after concussions. A study of 14 male and 13 female amateur rugby players by Bussey et al. reported altered head acceleration and cervical muscle tone in players who had previously suffered a concussion 12–24 months (10) prior and 24 or more months (7) prior, which may increase sensitivity to further injury (Bussey et al. 2019). Previous studies discuss the neuropsychiatric and cognitive effects of sustaining a concussion in adult and pediatric athletes across multiple sports, although there is little data on the resulting effect of these changes on injury incidence (McAllister and McCrea 2017; Shrey, Griesbach, and Giza 2011; Zuckerman et al. 2015; Curry et al. 2019).
When considering risk as a function of player count and using match-loss as the definition of injury, risk of an adult male rugby player sustaining a subsequent injury was slightly less than the risk of sustaining a recurrent injury, with the difference between the two falling between 95% confidence intervals. Interestingly, for pediatric players, there was a significant difference of 24% (p<0.05) between recurrent injury risk and subsequent injury risk when using the 24-hour time loss definition, but no significant difference between risk in studies using the match-loss definition. This suggests that pediatric players may be at a higher risk for more severe subsequent injuries than adults.
Limitations
There are several limitations to this study. First, there may be variation between injury incidence rates due to different injury definitions. One potential avenue of investigation is exploring variations in severity of subsequent injuries. Second, only two studies were identified that evaluated subsequent and recurrent injury rates in rugby players under the age of 18, quantifying less than 600 injuries, limiting the statistical power of the analysis (Archbold et al. 2018; Garraway and Macleod 1995). Similarly, only one study evaluated subsequent and recurrent injuries following concussions, resulting in fewer data points with a greater possibility of sampling bias (Cross et al. 2015). Additionally, our analysis here focuses on previously determined definitions of recurrent and subsequent injuries, and cannot offer specific information to aid in treatment or prognosis of specific rugby injuries. However, when considering adult players and defining injury as a 24-hour time loss, there is a clear difference between subsequent injury occurrence and recurrent injury occurrence in men’s professional rugby.
Conclusion
Time-loss criteria when defining injury plays a significant role when considering the difference between subsequent and recurrent injury incidence in male rugby players at multiple ages and levels of play. The type of index injury also influences the overall risk of both subsequent and recurrent injuries, and further investigation into incidence of secondary injury after specific types of index injury is warranted. The findings of this study suggest that in order to ensure player safety and longevity, injury prevention strategies should not focus solely on recurrent injuries, as they make up only a portion of secondary injuries.