Introduction
Extra-articular distal humerus fractures are uncommon and account for 3-6% of all fractures (Ekholm et al. 2006; Epps and Grant 1991; Buhr and Cooke 1959). Adequate reduction often requires operative intervention consisting of open reduction and internal fixation (ORIF) or total elbow arthroplasty (TEA); however, despite proper fixation, patient satisfaction is often lacking (Ekholm et al. 2006; Epps and Grant 1991; Buhr and Cooke 1959; Obremskey et al. 2003; Lauder and Richard 2020; Aitken and Rorabeck 1986; Rose et al. 1982; Anglen 2005; Jupiter and Mehne 1992). Furthermore, the operative intervention of these fractures is time-sensitive in an effort to restore alignment and range of motion (ROM) of the shoulder and elbow (Self et al. 1995; Waddell, Hatch, and Richards 1988; O’Driscoll 2005). This is imperative as several factors can increase the morbidity associated with distal humerus fractures, including the degree of comminution and bone demineralization. This becomes ever more pressing as we note the substantial increase in fragility fractures within the past 50 years—as well as the subsequent morbidity associated with these injuries (Palvanen et al. 1998, 2003; Kannus et al. 2002; Curtis et al. 2017) despite the plethora of available treatment options (Curtis et al. 2017; Giangregorio et al. 2006; Kanis et al. 2014). Thus, as patients continue to have suboptimal results with medical treatment, we must develop new approaches to combat these fractures surgically. Herein, we present a unique fixation method to aid orthopaedic surgeons in addressing these fractures. Our case explicitly highlights the use of 1.25x150mm (skinny) K-wires and dual plating to operatively manage a comminuted, displaced, low transverse distal humerus fracture in a 78-year-old female.
Case
A 78-year-old, right-hand dominant female presented to the emergency department after a ground-level fall with right elbow pain and decreased range of motion. Her pertinent medical history was remarkable for hypertension, intentional tremor treated with deep brain stimulator placement, osteopenia, previous ORIF of bilateral distal radius fractures, as well as alcohol and tobacco use. Physical examination revealed significant lateral right elbow swelling, pain at the elbow with wrist rotation, and limited range of motion secondary to guarding. The right upper extremity was neurovascularly intact throughout all motor and sensory distributions. Radiographic examination revealed a comminuted extra-articular distal humerus (Figure 1). Given the extent of the comminution and bone demineralization, there was concern that traditional ORIF with plate and screw fixation would not sufficiently capture the comminuted fragments. Therefore, utilizing a slight modification of the technique established by Olson et al (Olson and Dyer 2021)., dual locking plates were used in conjunction with skinny K-wires to achieve fractures fixation.
Surgical description
The patient was placed in the supine position on the operating table with the operative extremity flexed 90 degrees and placed across her chest. Utilizing a posterior incision, a triceps-sparing approach to the distal humerus was taken, creating a medial and lateral window. The fracture was identified as a comminuted low transverse fracture just distal to the olecranon fossa. The fracture was then manually reduced. Once anatomic alignment was achieved, provisional 1.25x150mm K-wires were placed to attach the disarticulate piece to the metaphyseal bone. A posteromedial distal humerus plate was secured with locking screws yielding a satisfactory reduction of the medial column. Skinny K-wires were subsequently placed in a lateral to medial fashion through the trochlea under direct fluoroscopy, thus securing the comminuted fragments. The wires were then bent along the lateral side of the contour toward the shaft and cut short in the metaphyseal bone lesion. The wires were secured in the same technique as Olson, with the subtle change of shortening the wires prior to administration of the plate, intraoperative images shown in figure 2. A posterolateral distal humerus plate was applied to the lateral epicondyle, securing the 1.25-mm k-wires beneath. The lateral plate was subsequently secured with locking screws. Intraoperative range of motion was assessed, and final C-arm radiographs revealed a satisfactory reduction of the articular fragment to the shaft with restoration of the underlying articular surface. Upon completion of the procedure, a soft dressing and ace wrap was applied to the operative extremity.
Results
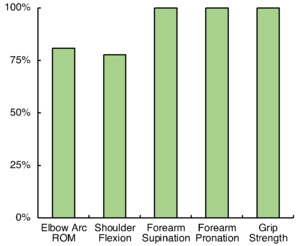
The patient began physical therapy six days after operative fixation, focusing on passive range of motion. Utilizing the contralateral upper extremity as a baseline: pain, range of motion, edema, and grip strength measures were trended (Figure 3). The patient self-reported her ability to perform activities of daily living (ADL) on a weekly basis. By postoperative week four the patient demonstrated substantial improvement in all tested categories, with graduation from therapy at postoperative week seven. At this point, she reported a 91% reduction in pain as well as the ability to use her right upper extremity for a majority of ADLs. Her grip strength had returned to baseline with a substantial reduction in edema of the affected extremity. Her total elbow range of motion was 81% of her non-injured extremity (117º elbow arc of motion). Additionally, the patient tolerated therapy and displayed successful bone healing on serial radiographs without the need for hardware removal or re-operation. Complete fracture healing was achieved at postoperative month five, as evidenced by radiographic examination (Figure 4).
Discussion
Several surgical options are currently employed to treat low transverse distal humerus fractures. Yet, there are still many challenges to ORIF of said fractures, including complex fixation, post-operative stiffness, and fracture nonunion (Epps and Grant 1991; Buhr and Cooke 1959; Obremskey et al. 2003; Anglen 2005; Jupiter and Mehne 1992; Tejwani et al. 2009; Prasarn et al. 2011; Rajput et al. 2016). The incorporation of implanted K-wires for a distal humerus fracture was first suggested by Kamrani et al. in 2012 when they reported on 19 patients who underwent “pin and plate fixation” for AO 13. A.1, and C.1-C.3 fractures (Kamrani et al. 2011). Following that report, Abdoli et al. reported on 14 patients, adapting the “pin and plate fixation” technique for distal humerus articular fractures (Abdoli, Farhoud, and Kamrani 2020). Both Kamrani’s and Abdoli’s studies demonstrated successful healing and early mobilization of the elbow. However, they reported significant complications, with a reoperation rate of 42.1% (8/19) and 50% (7/14) for Kamrani and Abdoli, respectively. In both Kamrani’s and Abdoli’s technique, the wires were bent on the lateral side and secured to the bone by a 3 or 4 hole plate, leaving a majority of the wires uncovered by the plate. Both Kamrani’s and Abdoli’s high reoperation rate stemmed from prominent wires, skin irritation, wire migration into the joint, and symptomatic hardware from their olecranon osteotomy fixation. Despite this, both studies illustrated a substantial return of elbow function with a total mean arc motion total of 99° for Kamrani and 97° for Abdoli in cohorts with an average age of 46 and 36, respectively (Kamrani et al. 2011; Abdoli, Farhoud, and Kamrani 2020).
In 2021, Olson et al. first described their skinny wire and locking plate fixation technique in 30 patients with comminuted intra-articular distal humerus fractures. Olson reported excellent functional results in the cohort with an average age of 59. 26% of their patients had known osteoporosis, and most of the fractures resulted from a ground level fall. In their technique, the fractures were anatomically reduced, and multiple skinny wires were placed to secure the fragments. These wires were then bent as they exited laterally, molded to the shaft and a secured beneath a lateral plate that covered a majority of the wire. For plate selection, they used only a lateral plate in 10% (3/30), bicolumnar plating in 81% (24/30), and bicolumnar + posteriolateral plating in 9% (2/30) of cases. Olson’s skinny K-wire and locking plate fixation technique showed 100% fracture union and average arc elbow motion of 102°. Their technique only resulted in a 35% (11/30) reoperation rate, with 8 having symptomatic hardware leading to its removal (Olson and Dyer 2021; Dryer 2020).
The case presented herein was designed to confirm Olson’s skinny K-wire and locking plate fixation technique, with a few key modifications in an attempt to reduce the reoperation rate. The triceps-sparing approach eliminated the complications that Olson, Abdoli, and Kamrani faced related to their olecranon osteotomy. To reduce hardware prominence, posterolateral and posteromedial plates were selected rather than direct lateral and medial plates. In the procedure, the order of plate and wire placements was also adjusted. After achieving anatomic reduction, a posteromedial plate was used to secure the medial column. This provided some stability of the fracture while skinny wires were implanted, ultimately reducing the total number of wires needed to secure the comminuted fragments. As Olson described, the wires exited laterally were bent to the contour of the distal humerus, however, in this case, the wires were shortened before the posterolateral plate was used to secure them to the lateral column. While these are slight modifications, reducing the number of wires, shortening the length of the wires outside of bone, and plate selection were all done in an effort reduce the overall hardware burden for the patient. For this patient, there was no skin irritation, no concern for pin migration, and no reported symptomatic hardware. Radiographic evidence of fracture healing coincided with the 78-year- old patient’s timely reduction in pain and quick recovery of ROM. Olson, Kamrani, and Abdoli reported follow-ups at a year or longer demonstrating elbow arcs of 102°, 99°, and 97° respectively, while this case demonstrates an arc of 117° after just seven weeks of recovery (Olson and Dyer 2021; Kamrani et al. 2011; Abdoli, Farhoud, and Kamrani 2020).
While this report demonstrates a successful case for this patient, it does not provide the opportunity to statistically compare the outcomes due to an overall low power with an n-value of one. A greater number of cases would be required to adequately assess the quality of outcomes from this technique. Given this, we plan to follow with a case series to further establish this modification of the skinny K-wire and dual-locking plate fixation method as a viable treatment option for distal humerus fractures.
Conclusion
The skinny k-wire and dual locking plate fixation technique was designed by Olson et al. to provide a structurally sound option for treating significant comminution distal humerus fractures. This study demonstrates a slight modification of this technique that yielded an expedited recovery time, significant improvement in pain, restoration of range of motion, and preserved overall function. Successfully treating a 78-year-old woman with a low transverse distal humerus fracture with minimal minimizing postoperative complications such as the need for reoperation or salvage procedures.
Thus, we find skinny K-wire and dual plate fixation to be a viable treatment option for distal humerus fractures complicated by comminution and bone demineralization. While a larger patient cohort is needed to fully access this procedure—we believe it is necessary to share this slightly modified technique in the interim with the orthopaedic community—to aid in treating patients with complex, comminuted, and/or demineralized distal humerus fractures.
This article will be in press until the end of 2023.




_and_final_placement_af.png)






_and_final_placement_af.png)



