Introduction
Total hip arthroplasty (THA) and total knee arthroplasty (TKA) are commonly performed using either general or spinal anesthesia (Herndon et al. 2021). Spinal anesthesia is reported to have some advantages to general anesthesia for TJA, including decreased cost, shorter length of stay (Turcotte et al. 2020), fewer complications and infections, and improved pain management (Matsen and Chen 2015). Due to these improved outcomes, spinal anesthesia has become the preferred anesthetic technique for many orthopedic surgeries over the past decades (Kamel, Ahmed, and Sethi 2022).
Evolution in total joint arthroplasty towards an outpatient procedure with quicker recovery has involved changing traditional perioperative medications. In efforts to minimize deleterious side effects of medications that can impact recovery and discharge, providers trend towards reducing medication dosing and type to the least amount necessary (Cooper et al. 2019). Therefore, it is prudent to ask whether patients are too lightly anesthetized during surgery in terms of remembering the experience of surgery. Likewise, it is important to know if that memory is a net negative, neutral, or a net positive on the patient the surgical event.
Anesthetic awareness occurs when patients can recall their surroundings or sensory perception during surgery. Awareness can occur despite proper anesthetic management and is often not associated with pain, although some patients do experience pain (Sandhu and Dash 2009). While anesthetic awareness may be experienced in 1-2 out of 1000 patients who receive general anesthesia (Paziuk et al. 2020; Sebel et al. 2004; Sandin et al. 2000; Bischoff and Rundshagen 2011), little data is available on the incidence of awareness that occurs in patients receiving regional anesthesia. Mashour et al (2009) found in a retrospective study of 116,478 patients that the rate of intraoperative awareness during regional anesthesia was 0.03% and was not statistically different from general anesthesia. However, they rejected the conclusion that the incidence of awareness was the same in anesthetized and sedated patients, concluding that the resolution of their retrospective study was too low to accurately capture an incidence. Mashour et al (2009) add that prospective approaches would better assess the incidence of awareness. Even more unsettled than the incidence of awareness in general surgery is its incidence in unambiguously louder and more physically stimulating orthopaedic surgery total joint arthroplasty cases. Furthermore, concerns about recall of auditory and physical sensations during hip and knee arthroplasty surgery is a common reason given by patients requesting general anesthesia.
The purpose of this study is to determine the incidence of auditory and physical sensory recall among patients having arthroplasty surgery and its risk factors, comparing general and neuraxial anesthesia, and assessing the impact of recall on patient satisfaction of the surgical event. We hypothesize a greater incidence of recall with neuraxial anesthesia and a negative impact of recall on patient satisfaction.
Methods
After obtaining approval from our institutional review board, we prospectively enrolled 164 consecutive patients undergoing primary or revision hip or knee arthroplasty between March 2017 and November 2017. Three surgeons and 25 anesthesiologists in an urban academic university hospital setting provided care. No patients were excluded from this study.
Type of anesthesia, intravenous fentanyl and midazolam doses, pre-operative diagnosis, type of surgery, anesthesia duration, and surgery time (morning vs afternoon case) as well as patient demographics such as age, BMI, sex, comorbidities, American Society of Anesthesiologists classification (ASA class) (“ASA Physical Status Classification System” 2014) were collected from the medical record. Although neuraxial anesthesia is the preferred method for anesthesia for hip and knee arthroplasty at our institution, the anesthesia type and bolus drug totals given to each patient were individualized to the patient by anesthesiologist preference.
After surgery when alert and non-drowsy, each patient was asked if they experienced any sensory recall during surgery (yes or no), specifically asking whether they recalled any instrument sounds like sawing or hammering. They were also asked about recall of physical sensations like impaction or leg manipulation. For each question, if answered in the affirmative, they were then asked how that recall impacted their overall level of satisfaction of the surgery experience (improved, worsened, or no effect).
Statistical Analysis
Statistical analyses were done with SPSS (version 28.0, SPSS Inc., Chicago, IL, USA). Pearson’s correlation coefficient was used to determine correlation between each variable and sensory recall. A binary logistic regression model was used to identify risk factors for sensory recall. Differences were considered statistically significant if p < 0.05.
Results
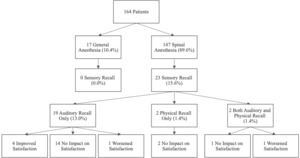
Seventeen (10.4%) patients received general anesthesia and 147 (89.6%) patients received spinal anesthesia. No patients with general anesthesia had sensory recall. Demographic data is shown in Table 1, and operative data is shown in Table 2. Of the 164 patients surveyed, 23 patients (14.0%) had sensory recall: 19 (11.6%) had auditory-only recall, 2 (1.2%) had physical-only recall, and 2 had (1.2%) both. The overall incidence of sensory recall among the 147 patients with spinal anesthesia was 15.6% (Table 3), with 13.0% auditory-only, 1.4% physical-only, and 1.4% both.
Seventeen (73.9%) of 23 patients with sensory recall reported no impact on satisfaction with the overall surgical experience; 14 had only auditory recall, two had only physical recall, and one had both auditory and physical recall. Two (8.7%) patients with sensory recall reported worsened satisfaction (1 had only auditory recall and 1 had both auditory and physical recall). Four (17.4%) patients with sensory recall, all auditory only, reported that the recall had improved their satisfaction with the surgical experience (Figure 1).
There was a weak correlation between spinal anesthesia and sensory recall (r = 0.163, p = 0.037) (Table 4). On logistic regression, we found that decreasing age (p=0.032, 95% CI, 0.894–0.995) and smaller doses of midazolam (p = 0.009, 95% CI, 0.283–0.832) were significant risk factors for sensory recall (Table 5). Other demographic or operative parameters including gender, BMI, number of comorbidities, ASA class, intravenous fentanyl doses, pre-operative diagnosis, type of surgery, anesthesia duration, and surgery time were not found to correlate to or be significant risk factors for recall.
Discussion
A prospective study of 164 patients receiving THA or TKA was conducted to investigate the rates of sensory recall under general and spinal anesthesia, and how recall impacts patient satisfaction. The overall rate of recall for arthroplasty patients was 14.0%. Our results showed that no patients with general anesthesia had recall, while 15.6% of patients who receive spinal anesthesia experienced recall. Of the patients who experienced recall, 73.9% report no impact on satisfaction, 8.7% reported worsened satisfaction, and 17.4% reported improved satisfaction.
General surgical literature reports rates of recall under general anesthesia between 0.1-0.2% (Paziuk et al. 2020; Sebel et al. 2004). While most studies report an extremely low rate of awareness during general anesthesia, Domino et al (1999) reported that 1.5% of general anesthesia patients had recall and Medrzycka-Dabrowska et al (2017) found a 4% rate of awareness among patients that received “light” anesthesia or general anesthesia without hypnotic agents and narcotic relaxants. These studies bring attention to the variability in baseline incidences in anesthesia awareness and how it may affect patient outcomes. While our results showed 0% recall for patients receiving general anesthesia, only 17 patients in our study received general anesthesia, so small sample size limits our ability to accurately assess recall under general anesthesia. However, among patients receiving spinal anesthesia that underwent total joint arthroplasty, 15.6% experience recall, 150x greater than reported in general surgery patients having general anesthesia (Paziuk et al. 2020; Sebel et al. 2004; Sandin et al. 2000; Bischoff and Rundshagen 2011). Mashour et al (2009) asserts that sedated patients are often aware of their surroundings and speaking with the anesthesiologist, predicting that the rate of recall among sedated patients is higher than patients receiving general anesthesia. Our data supports this prediction and matches the accepted idea that patients under spinal anesthesia are more likely to have awareness that patents under general as described by the ASA (“Waking up during Surgery - Made for This Moment,” n.d.).
To our knowledge, no previous research has been conducted on how intraoperative awareness impacts patient satisfaction. While the majority of patients reported no change or improved satisfaction, some patients did report worse satisfaction due to recall. However, the incidence of this was low with about 1.2% of all patients reporting worse satisfaction due to recall. Awareness while under anesthesia has been shown to have potential psychological consequences such as PTSD causing anxiety, depression, and sleep disorders (Mędrzycka-Dąbrowska et al. 2017). Strategies to potentially reduce the rate of and potential harmful consequences of anesthesia awareness include putting headphones on the patients during surgery and administering proper doses of medication specific to each patient (Mędrzycka-Dąbrowska et al. 2017). A factor that may contribute to satisfaction is the expectation for level of consciousness set by anesthesia providers. Differences between expected levels of consciousness under general and regional anesthesia may be unclear to patients (Esaki and Mashour 2009), so providers should set appropriate expectations as another strategy to lower rates of worsened satisfaction (Mędrzycka-Dąbrowska et al. 2017).
Kerssens et al (2009) conducted a study that used the bispectral index, a monitor of hypnotic state, to measure the likelihood of recall during surgery in orthopedic patients. It was found that using bispectral index during surgery to decrease each patient’s level of hypnosis resulted in a decreased likelihood of having recalling words that were said during surgery. This measure is another potential method to reduce the rate and potentially harmful effects of having sensory recall during surgery.
We found that lower doses of midazolam, a benzodiazepine, were a significant risk factor awareness while under anesthesia. Benzodiazepines are known for producing sedative effects through enhancing the effects of Gamma Amino Butyric Acid (GABA), an inhibitor of the CNS (Rudolph and Knoflach 2011). Specifically, midazolam is known to produce anterograde amnesia which results in a lack of recall of events occurring after drug administration and in this case during surgery (Beracochea 2006). We believe this increased likelihood of developing anterograde amnesia explains the association we found between lower doses of midazolam and increased recall. Our findings were consistent with Miller et al (1996) who found that intraoperative awareness was lower following increased midazolam administration.
A limitation of our study was that significantly more patients received spinal anesthesia than general anesthesia, so our small sample size for general anesthesia limits our ability to accurately find the rate of recall among patients receiving general anesthesia. A second limitation was that the type of anesthesia and drugs administered to each patient varied and were individualized to fit the patient’s needs, meaning there was no randomization as spinal anesthesia is the preferred anesthesia method, which may affect the results. A third limitation was that this study was done at a single academic institution, so our results may not be generalizable to other institutions as the teaching environment may have caused patients to be more or less susceptible to sensory recall.
In conclusion, our data showed higher rates of recall among regional anesthesia than general anesthesia. However, for the majority of patients who experience recall, satisfaction was not worsened. Although we focused on instrument sounds, our high rate of sensory recall serves as a reminder to also be mindful of conversations in the operating room.