Introduction
Rotator cuff tears are one of the top causes of concerns seen by orthopedists. Over 1 million rotator cuff repairs are performed in the United States each year (“Orthopedic Soft Tissue Repair Market: Global Industry Analysis, Size, Share, Growth, Trends & Forecast, 2015-2030” 2022). Studies have found that up to 94% of large and massive tear rotator cuff repairs fail, with the majority failing as early as six months (Galatz et al. 2004; Iannotti et al. 2013). Symptoms are variable and can include nighttime pain, decreased strength, and difficulty performing daily activities. Initial diagnosis may include a physical exam with x-ray to assess the level of osteoarthritis, co-commitment fractures, and “high-riding” of the humeral head indicating advanced rotator cuff arthropathy. Furthermore, advanced imaging may be obtained using MRI or CT Arthrogram. Treatment may vary depending on tear size, fatty degeneration, muscle atrophy, type of tendon tear, and the level of retraction of the rotator cuff.
Case Report
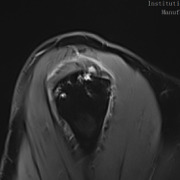
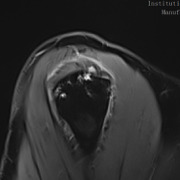
This 48-year-old male is a right hand dominant, nonsmoker with an active lifestyle. This patient presented with excellent range of motion and passing inactive range. Upon examination, strength presented at 5/5 rotator cuff, mild tenderness over the proximal long head of the biceps, but positive for subacromial impingement testing. Imaging revealed a skeletally mature individual with an intact glenohumeral joint space without signs of osteoarthritis and an intact acromial-humeral height distance (Figures 1-3).
Upon initial examination, the patient was treated with a home exercise program, anti-inflammatory Meloxicam over two weeks, and a subacromial cortisone injection with a follow up at six weeks. At six weeks follow-up, the patient symptoms improved slightly after injection and anti-inflammatory medication, but the patient continued to experience pain and difficulty sleeping. An MRI was ordered for further examination.
The MRI revealed an anterior full-thickness supraspinatus tear from the origin with mild retraction and moderate delamination. Fluid signal was seen within the mid-substance of the supraspinatus tendon medial to the location of full thickness tear. Subchondral cystic changes in the greater tuberosity were also observed at the insertion site. (Figures 4 & 5)
Treatment
After a failed conservative pain management treatment plan and a diagnostic MRI, the recommended treatment was arthroscopic rotator cuff repair with biologic augmentation for the rotator cuff as well as hardware augmentation for the anchors.
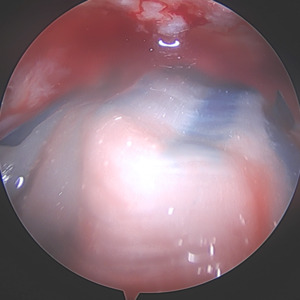
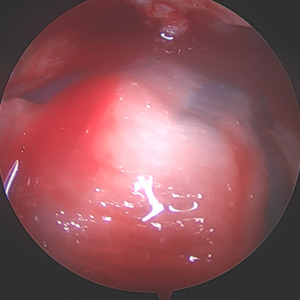
For the primary repair, a double row repair was completed. Medial anchor placement and fixation needed special consideration due to poor bone quality as a result of the subchondral cyst. To support anchor fixation, a calcium phosphate substitute (Tactoset® by Anika Therapeutics) was injected under direct visualization into the subchondral cyst and allowed to set for approximately 10 minutes. One triple-loaded medial row anchor (Healix Advance™ with Dynacord™ by DePuy Synthes) was then placed into the greater tuberosity. Six sutures were passed through the rotator cuff and tied in standard arthroscopic fashion after which two lateral row anchors (X-Twist™ by Anika Therapeutics) were placed to complete a double-row fixation of the rotator cuff tear.
Due to the delaminated nature of the tear and active work as a laborer, biologic augmentation (TAPESTRY® Biointegrative Implant by Embody) was added to support tendon healing. This biologic augmentation was chosen due to the delamination and retraction of the rotator cuff as an increased change of retear is noted when present. The arthroscopic introducer was used from the lateral portal via the cannula. Once appropriately positioned over the delaminated area, three bioabsorbable anchors were used to fixate the implant in the tendon and bone, with two anchors placed medially in the soft tissue and two anchors placed laterally into bone.
Discussion
A successful mechanical rotator cuff repair does not always translate to a healed rotator cuff. This patient is young, active and the MRI reveals two areas (tendon delamination and subchondral cysts) where we can leverage technological advancement along with arthroscopic techniques to the improve outcome.
Encountering a subchondral cyst intraoperative can be rather challenging. Do you opt for a larger anchor, buddy anchor, or a suboptimal location for the anchor? Furthermore, the question of anchor pull out may dictate the patient ‘go slow’ during the initial rehabilitation process leading to increased stiffness and pain. I decided to use calcium phosphate to augment at time of surgery prior to anchor placement because I wanted excellent anchor strength for anchor placement due to the diagnosis of a subchondral edema. This substantially increases the immediate pull-out strength of the anchor and allows me to continue my standard post operative rehabilitation protocol.
A medial row anchor was then inserted into the site of calcium phosphate placement with excellent bony purchase. This anchor is loaded with dynamic sutures that self-tension for continuous compression for at least 12 weeks. Two vented anchors (X-Twist 4.5mm PEEK) were then placed laterally to complete the double row repair. The moderate size tear with mild retraction of the tendon drove my decision to complete a double row repair. Double row repairs have been shown to have improved mechanical strength, contact pressure on the repair site, and rotator cuff footprint restoration. The dynamic nature of the sutures is especially important for retracted tears to help maintain the contact pressure to the tuberosity during the initial stages of healing. Any laxity in the suture can lead to increased retear rates.
I chose to include biologic augmentation due to the extensive delamination seen on the preoperative MRI as well as intraoperative findings. Several preoperative patient risk factors (age, BMI, smoking, diabetes) may be reviewed when considering biologic augmentation of a tear due to increased risk of retearing or poor healing. The bioaugmentation used is a highly aligned, porous collagen implant which supports formation of new tendon-like tissue. The alignment and significant porosity of the implant allows for increased cell proliferation and remodeling. The implant covers a wide surface area and can be precisely placed arthroscopically over the area of concern. Another benefit of the bioaugmentation implant is that it may increase tendon thickness during healing, which could allow for better post-operative results. Furthermore, using it to augment the tendon does not require any additional post-operative protocols outside of the standard protocol.
Unlike other collagen implant fixation, this system allows the implant to be fixated with bioabsorbable anchors which can be used in both tendon and bone. The dual anchor inserter does not require any bony prep work before inserting the anchors into bone, allowing for an efficient workflow. Additionally, the system includes the streamlined delivery of the pre-loaded implant to the arthroscopic space on the implant.
It is important to note that using the biologic implant will incur additional cost to the total cost of the surgery and may increase OR time. However, the average time to implant is approximately five minutes.
This patient was able to obtain an arthroscopic rotator cuff repair with augmentation at areas of concern. The subchondral cyst was able to be augmented with calcium phosphate prior to anchor placement. The retracted tear was then fixated to the tuberosity using dynamic sutures, thus allowing for rotator cuff footprint restoration. A biointegrative Implant was then used arthroscopically to fixate over the area of extensive delamination to support tendon healing. Post-operative protocol was the same as a standard rotator cuff repair. For my protocol, I call for a sling for three weeks followed by physical therapy with active, assisted range of motion, passive range of motion, and strengthening exercises.
At four months post-op, the patient was able to return to his activities of daily living, which include weightlifting and work.






.png)








.png)




