Introduction
The thumb and its corresponding joints are really important for our day to day activities, as they permit us to perform fine and delicate movements (Signori et al. 2017). Thus any injury to this apparatus would greatly affect a patient’s quality of life. These injuries are relatively rare, with carpometacarpal (CMC) joint dislocation accounting for less than 1% of injuries to the hand (Bosmans, Verhofstad, and Gosens 2008), and fracture to the trapezium about 3% of carpal bone fractures (Walker, Greene, and Lunseth 1988; Kose, Keskinbora, and Guler 2014). There is one pattern where a thumb CMC dislocation and trapezium fracture occur together. To the best of our knowledge, this has been described in few studies with no consensus on the treatment (Walker, Greene, and Lunseth 1988; Kose, Keskinbora, and Guler 2014; Garavaglia et al. 2004; Ramoutar et al. 2009; Beekhuizen et al. 2019; Alonso and Couceiro 2018; Kohyama et al. 2018; Pina et al. 2021; Kosagi Sharaph, Saseendar, and Shanmugasundaram 2019; Morizaki and Miura 2009; Mody and Dias 1993; Kukreti and Harrington 2004; Parker, Czerwinski, and Lee 2008; Garneti and Tuson 2004; Mumtaz and Drabu 2009; Tolat and Jones 1990; Afshar and Mirzatoloei 2006; Chamseddine et al. 2009). In this article, we describe the case of a patient who had a traumatic trapezium-thumb metacarpal base fracture-dislocation, treated with closed reduction and percutaneous pinning with excellent functional and radiological results.
Case Presentation
A 25 year old male presents to the clinic for a left ankle fracture and a left thumb fracture dislocation. The patient is a cowboy. He states that his horse bucked him off and then fell on him. He had significant pain described as constant and throbbing. Aggravating factors include walking and any left hand movement. Alleviating factors include immobilization and taking pain medications.
We will omit all info pertaining to the ankle injury for the sake of the report.
On physical exam, there was swelling over the wrist and the first carpometacarpal joint. There was crepitus and a gross dislocation of the trapezium over the first metacarpal. When the thumb was stabilized, EPL, FPL, middle finger flexion and extension and intrinsic muscles of the hand were all intact. Pulses and sensation were normal. Left arm was put in a short arm thumb spica splint, and CT of the wrist was ordered, showing a Bennett fracture as well as a trapezium comminuted fracture with dislocation of the thumb metacarpal. Images of the CT are shown in Fig.1 below. We decided to proceed with closed reduction and percutaneous pinning with possible open reduction and internal fixation.
Multiple 1.1 joysticks were used to obtain a near anatomical closed reduction. Then, multiple K-wires size 1.6 and 1.1 were used to secure and fix the trapezium fracture as well as the carpometacarpal dislocation through a wire spanning the thumb metacarpal bone and the trapezium, as well as another wire spanning the thumb and the index metacarpal bones as an added measure of safety to avoid a recurrent dislocation. Closed reduction of the Bennett fracture using a 1.1 K-wire was attempted with acceptable reduction obtained. Fluoroscopic images were satisfactory in multiple planes (Fig.2). Relaxing incisions were done around the K-wires and the pins were cut close to the skin and bent. A sterile dressing was applied followed by a combined sugar-tong and thumb spica splint. The patient’s arm was placed in an arm sling. The splint and pins were removed after 4 weeks.
Repeat X rays showed good alignment and healing in progress (Fig.3) and physical therapy was started. The patient had gradual improvement in his wrist and thumb ROM with the help of physical therapy.
At his follow up 14 weeks post op, the patient was back to work, with pain rated at 2/10, described as intermittent that worsens with prolonged activity with slight stiffness on thumb extension. At 20 weeks post op the patient was asymptomatic and working without restrictions.
Discussion
Trapezium fracture and Carpometacarpal dislocation are each rare hand injuries. Their combination is even less prevalent but has been described in few reports in the literature. Significant trauma to the radial wrist is usually the culprit. Two mechanisms of injury have been described for this rare entity: dorsoradial impaction and indirect axial load (Beekhuizen et al. 2019; Kukreti and Harrington 2004; Strauch, Behrman, and Rosenwasser 1994).
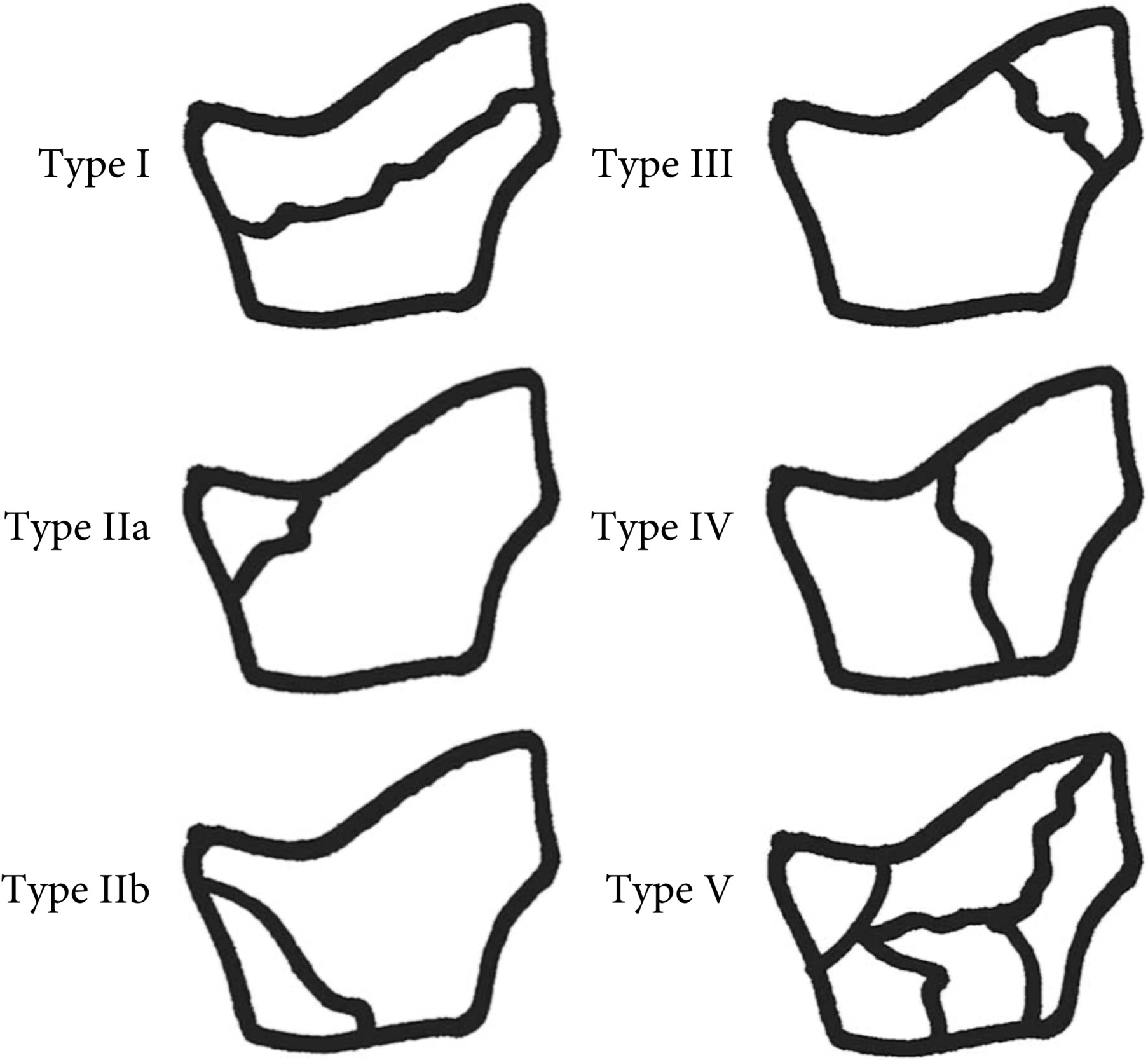
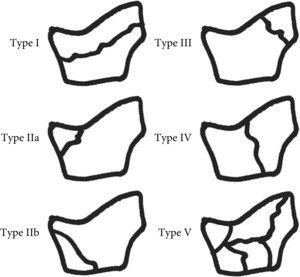
Trapezium fractures are easily missed since routine hand and wrist radiographs are at times not enough to properly visualize the trapezium. Robert’s view, which is a true AP view that visualizes the thumb carpometacarpal joint, is helpful as well as a wrist computed tomography scan which is considered the gold standard imaging modality for this injury (Kose, Keskinbora, and Guler 2014; Ramoutar et al. 2009; Pina et al. 2021). These fractures are classified according to Walker et al., who studied a series of 10 trapezium fractures (Fig.4). Most reported cases of trapezium fractures along with carpometacarpal dislocation were of types IIa, IIIb or IV (Kose, Keskinbora, and Guler 2014). As for carpometacarpal dislocation itself, it was found that the radial collateral ligament is the primary restraint against dorsal dislocation (Kose, Keskinbora, and Guler 2014). Since the combination of both injuries is scarce in the literature with a handful of cases described, there is no consensus on the best treatment. Described management options include conservative, closed reduction, closed reduction with external fixation, closed reduction with percutaneous fixation and open reduction and internal fixation (Kose, Keskinbora, and Guler 2014; Beekhuizen et al. 2019; Alonso and Couceiro 2018; Kohyama et al. 2018; Pina et al. 2021; Kosagi Sharaph, Saseendar, and Shanmugasundaram 2019; Mody and Dias 1993; Kukreti and Harrington 2004; Parker, Czerwinski, and Lee 2008; Garneti and Tuson 2004; Mumtaz and Drabu 2009; Chamseddine et al. 2009; Vanschil and Desmet 1986). All with good to excellent results. There is some consensus however for isolated fracture with no displacement to be treated conservatively, and to surgically treat those with displacement or with associated dislocation (Pina et al. 2021). In addition, there are no long term studies on these injuries (Kose, Keskinbora, and Guler 2014), with all short term results considered good to excellent. However, Kohyama et al. reported the development of thumb carpometacarpal joint osteoarthritis documented by radiological findings after 2 years for a case treated with open reduction and internal fixation despite good functional results (Kohyama et al. 2018). This emphasizes that more long-term studies should be done to prevent the development of such complications.
In our case, the patient had a traumatic event that caused a Walker type V trapezium comminuted fracture along with a 1st MC Bennett fracture-dislocation. The surgeon opted to perform a closed reduction with percutaneous pinning using K wires. Latest follow up at 4 months post op showed excellent radiographic and functional results.
Conclusion
Trapezium fracture with thumb CMC dislocation is a rare entity but it has been described in the literature. No consensus exists on the best treatment for such cases. We presented a case with such diagnosis treated with closed reduction and percutaneous pinning with excellent results. This shows that this approach is a feasible, less invasive and effective option. However, long term studies are needed to monitor for the development of joint osteoarthritis and other complications.





.jpeg)





.jpeg)