Introduction
Distal biceps ruptures occur in 1.2-2.5 per 100.000 persons year (Safran and Graham 2002), mostly due to an eccentric elbow contraction against load (O’Driscoll, Goncalves, and Dietz 2007). Smoking, weight training and anabolic steroids are very well-known risk factors (Safran and Graham 2002; Alentorn-Geli, Assenmacher, and Sánchez-Sotelo 2017). Clinical presentation is usually constant: sudden “pop” with weakness with elbow flexion and supination (Srinivasan, Pederson, and Morrey 2020). Ultrasound or magnetic resonance provide information of tendon retraction (Alentorn-Geli, Assenmacher, and Sánchez-Sotelo 2017). When delays in diagnosis occur, tendon retraction and low-quality tissue make it almost impossible to perform a repair. Reconstruction with allograft is one of the possible options, but new sterile dermal acellular matrixes have also shown good outcomes (Petrie et al. 2022)
We present a clinical case of a bodybuilder patient with a delayed distal biceps tendon rupture with a severe frayed and retracted tissue, and one year follow-up clinical photos, showing a satisfied patient with complete range of motion.
Description of the issue
We describe the case of a 34-year-old male who presented to our practice with a right biceps tendon rupture. Thirty-five days prior to his visit, our patient was weightlifting, and while bearing a heavy load he heard a “pop” and felt an immediate inability to flex his elbow. He was first attended in a general emergency department, and after no solution was given to him, he sought help at an urgent care. No diagnosis nor surgical treatment was offered for the first month, and therefore nearly six weeks into the injury he came to our facilities.
The patient was a right-handed active male who had no relevant medical history. His BMI was 32 kg/m2, and his sports activity included professional heavy weightlifting. Socially, he was a non-smoker, occasional drinker, non-drug user and with no history of quinolone use nor corticosteroids in the last six months. He did have a positive history of testosterone cypionate injection, an anabolic and androgenic steroid which due to its long half-life and ability to produce large muscular growth improvements is one of the most popular injected steroids among athletes. No previous tendon injury was reported.
Concerning physical exam, he presented with weakness for elbow flexion and forearm supination. The stump was not palpated in the antecubital fossa but proximal to the elbow crease, and the “reverse Popeye’s sign” was present (Alentorn-Geli, Assenmacher, and Sánchez-Sotelo 2017). And MRI was ordered (Figure 1), and the patient was scheduled for surgical treatment.
Results
The patient’s arm was sterilely prepped. Once anesthesia was obtained, and limb ischemia achieved, a longitudinal 3-cm incision just distal and radial to the antecubital fossa was performed. Before the incision, the stump could be palpated subcutaneously at 4-5 cm proximal to the elbow crease, which correlated with the appearance of the tendon’s MRI imaging. Therefore, it was felt that even though there was delayed presentation for this, we would be able to achieve primary repair.
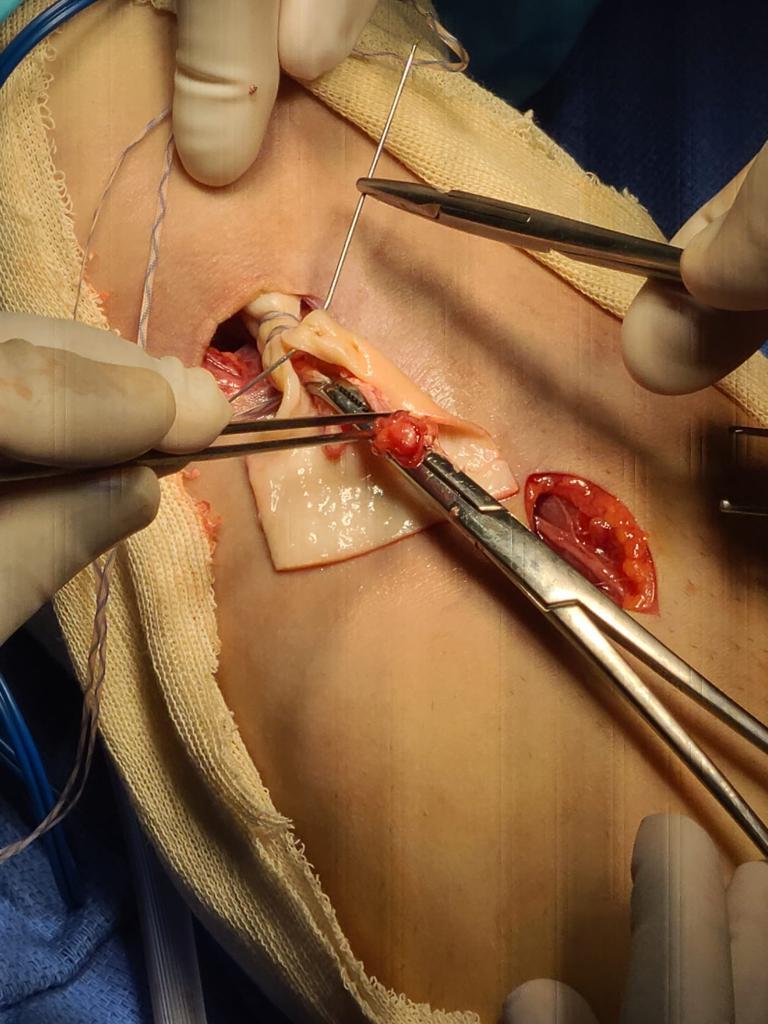
The brachialis and small vessels were identified and retracted. However, with digit exploration, biceps tendon could not be located. Incision was extended slightly and at this point, tendon was found, but unable to be pulled on with an Allis clamp, as it was noted to be quite frayed. Therefore, a second counter incision was made proximally at the level of the musculotendinous junction of the distal biceps, parallel to the antecubital crease for good cosmetic healing. The biceps tendon was noted to be markedly scarred, frayed, and rolled up in the coil (Figure 2). This is not the usual scenario where the tendon can be unwrapped and reattached to the bicep’s tuberosity. It was decided to proceed with tendon reconstruction in order to pull the biceps down distally and restore the contour of the upper arm. With this purpose, a 1.75mm thickness sterile acellular graft was used (Figure 3), entubulating the remaining frayed tendon and suturing it proximally at the musculotendinous junction with high resistance caliber-0 sutures (Figure 4). A Krackow suture was created distally in the acellular matrix (Figure 5), resulting in a final 8 millimeters width distal stump. This new tendon was then tunneled underneath the skin bridge between the proximal and distal incision in the same path of the anatomic normal biceps (Figure 6).
The scarred biceps tuberosity was identified while holding the forearm in supination. Debridement was carried out until bleeding was achieved. A central pin, followed with an 8-mm drill, was used unicortically, and a cortical button with a high resistance suture secured the reconstruction in its place. A 7-mm interference bioabsorbable screw was placed, with excellent purchase and grabbing the tendon strongly. A collagen tissue matrix was injected around the reconstruction for enhancing the healing environment (Figure 7). Hemostasis was achieved, and skin closed. The arm was held in 90 degrees of flexion with gentle supination. A postoperative control imaging was taken (Figure 8).
At this point, the elbow could completely be extended, however a thermoplastic cast was used to avoid extension further than 30º for four weeks, while early healing occurred. Wrist and hand-gripping exercises were encouraged from the beginning. In scheduled physical therapy, active passive flexion was authorized up to 90º and active extension as said, for the first six weeks. Later on, isometric exercises were introduced. Patient resumed his previous sports activity four months after surgery (Figure 9, 10).
Discussion
Early anatomical repair is the commonly accepted recommendation for distal biceps ruptures (Srinivasan, Pederson, and Morrey 2020). But, when the diagnosis is delayed, this anatomic repair becomes challenging, due to retraction, loosening of elasticity and atrophy of the stump (Darlis and Sotereanos 2006). At this point, use of allografts makes it possible. This augmentation has been published with a wide myriad of tendons, even with autogenous tendons (Hang, Bach, and Bojchuk 1996; Storti et al. 2021; Murthi et al. 2017). Cadaver allografts, mainly Achilles tendon, has shown good outcomes (Sanchez-Sotelo et al. 2002). Risk of infection has been described when using allografts in the knee (Bansal et al. 2018).
Recently, acellular dermal allografts have become a possible solution, diminishing risk infection and avoiding autograft morbidity, with a great biomechanical profile (Conroy et al. 2017; Barber, Herbert, and Coons 2006). These biological scaffolds allow vascular ingrowth, fibroblasts proliferation and host cells, while providing a good structural support (Barber et al. 2012). They have been used in ankle’s tendons ruptures (Rapley, Crates, and Barber 2010).
As has been indicated in our clinical case, this acellular dermal matrix achieves satisfactory suture strength, allowing complete range of motion and even performing heavy demanding sport practice.