Case Presentation for Arthroscopic Internal Fixation of Coracoid Fractures
Case Description: Patient is a 27 year old right hand dominant male that presented initially with right shoulder pain. He denied any specific trauma or injury to the shoulder but has radiographic evidence of a Type II coracoid fracture that has progressed to symptomatic non-union. After 6 months of attempted non operative including physical therapy and activity restriction, treatment discussion of surgical options was initiated. Patients baseline activity includes frequent exercise activity but no formal sport or powerlifting. Historically coracoid fractures go on to uneventful union. Literature supports a very high union rate with a conservative estimate of 81% or more going on to union and returning to sport at an average of 2.8 months (6). Typically surgery is reserved for patients with greater than 1 cm of displacement, or less than 1 cm of displacement but concomitant shoulder instability/SSSC disruption. In discussing this patients atypical presentation of symptomatic non union, surgical intervention was deemed beneficial after failed conservative management. CT and MRI were both performed to fully evaluate whether healing was still actively taking place or if the fracture was truly a fibrous nonunion requiring intervention All surgical options were discussed with the patient and in the end the decision was made to perform the procedure arthroscopically. While this is a novel technique previously undescribed in the literature, it focused on arthroscopic principles utilized during the arthroscopic Latarjet, which made it a very comfortable surgical approach.
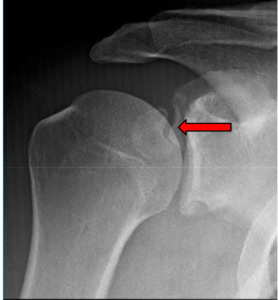
Imaging: Preoperative imaging included standard radiography using anteroposterior, Grashey, scapular Y and axillary views (Fig 1-2). After determining the presence of a coracoid fracture, advanced imaging was conducted via computed tomography with addition of 3-dimensional reconstruction. CT imaging was suggestive of a type 2 coracoid fracture nonunion (Fig 3) which was then further verified with no enhancement with T2 MRI sequences (Fig 4).
Preoperative plan: Initial preoperative plan included placing the patient in a standard beach chair configuration and completing a full diagnostic arthroscopy of the shoulder. The rotator interval would be taken down and utilization of arthroscopic Latarjet accessory portals would be used to fully identify the nonunion. If the fracture remained mobile, debridement of all fibrous tissue would be performed and a 4.5 mm cannulated screw would be used to compress across the fracture site.
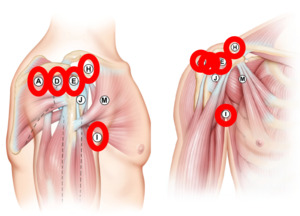
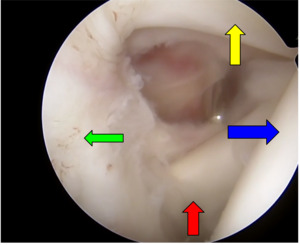
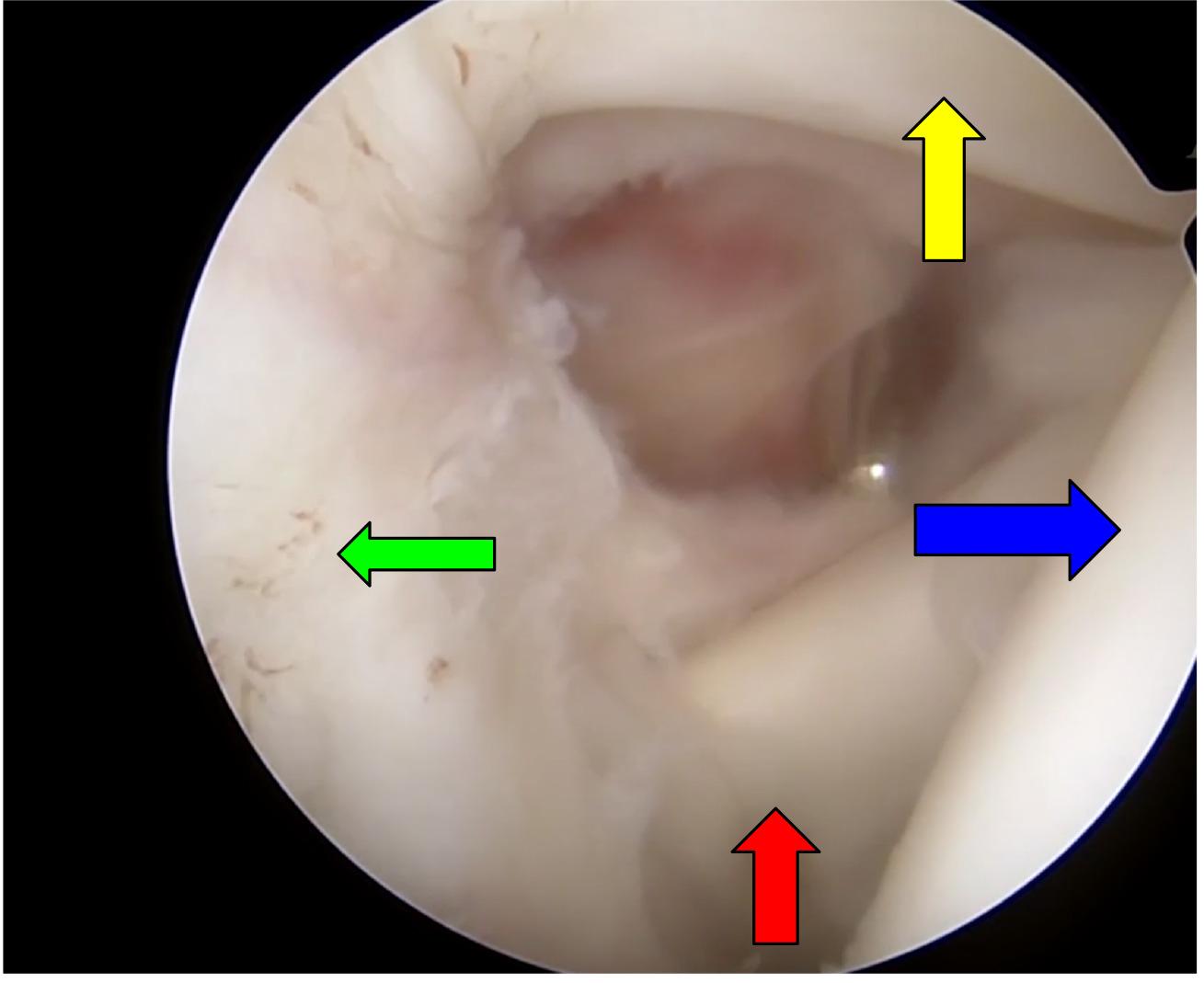
Operative Results: The patient was positioned supine in beach chair position with the assistance of a mechanical arm holder. A 30 degree scope was used during the entire procedure without need to switch to a 70 degree scope due to multiple portal use. The first portal was established as a standard posterior viewing portal (A) followed by a standard anterior portal (E) under direct visualization, Figure 5 demonstrates portal selection. From the anterior portal a thorough debridement via arthroscopic shaver and radiofrequency ablation was undergone of the rotator interval to the tip of the coracoid process (Figure 6). After visualization of the lateral coracoid was obtained, the radiofrequency ablator was used to clear the soft tissue until the coracoclavicular ligament is encountered at the anterolateral aspect of the coracoid (Figure 7). Unlike the arthroscopic Latarjet technique, the CC ligament does not need to be fully released but can be partially released for visualization. The D portal (anterolateral portal) is then made under visualization from the posterior portal and viewing is moved to the D portal. The ablator is then moved to the anterior portal to allow for clearing of the superior coracoid. The purpose of the switch of viewing to the D portal is increased visualization of the tip of the coracoid, conjoined tendon, and an en face view of the glenoid. Extra care should be undertaken when moving medially to the fracture site to avoid damage to the axillary nerve, blunt dissection can be done with the ablator to identify the axillary nerve. Next, through the D portal, the I portal (anterior inferolateral portal) can be established under direct visualization in line with the conjoined tendon for placement of the K-wire and cannulated screw. Through the I portal the ablator is inserted to remove a small portion of conjoined tendon for the K-wire insertion site and future cannulated screw. Placement of a blunt trocar is then inserted into portal E and fracture mobility is assessed. We then moved to creating portal H, insertion of a spinal needle under direct visualization in line and superior to the coracoid process. The ablator can then be used through portal H to debride the built up non union fibrous soft tissue (Figure 8). To get a full and adequate debridement of the fibrous tissue, a small amount of the pectoralis minor tendon may need to be released depending on the location of the fracture as it may act as a deforming force. After adequate debridement, a shaver or burr is used to debride bone edges to bleeding bone. A drill guide is then inserted through portal I at the tip of the coracoid process (Figure 9) while a probe is inserted through portal H to reduce and stabilize the fracture site for K wire insertion. The K-wire can be used to joystick the fracture as well while in the distal fragment. Once reduction is achieved the k wire is inserted into the proximal fragment, but not advancing too far to put the suprascapular nerve at the suprascapular notch. A cannulated drill is then passed over the K-wire in both proximal and distal fragments. A 4.5 cannulated screw is then inserted over the guidewire (Figure 10). A blunt trocar can be placed within the H portal to allow the operator to prevent/minimize rotation of the fragment during insertion of the cannulated screw. Post operative care included postoperative radiographs for reduction assessment and screw length (Figure 11). Patient placed within an abduction sling for 6 weeks, gentle range of motion was initiated at 2 weeks post op. After fracture union, the patient should return to normal activities at approximately 3 months post op.
Discussion: This case highlights the exciting opportunity that exists for arthroscopic shoulder procedures. While most coracoid fractures will never require surgical stabilization it is also important to acknowledge that when they do, minimizing morbidity should be of the highest priority. We believe Arthroscopic shoulder surgery provides better visualization and detail of anatomy compared to open procedures. It also is important to note that literature supports decreased rates of infection with arthroscopic shoulder surgery versus open shoulder surgery (10). When you combine improved visualization with lower infection risk the argument against performing this procedure arthroscopically likely comes entirely down to comfort. Our comfort comes from performing many arthroscopic Latarjet procedures, but we believe that comfort is attainable. For this specific case not only were the same portals utilized but many of the proprietary tools specific to the Latarjet set were used to complete this surgery. While this case is not as complex as an arthroscopic Latarjet it exemplifies the possibilities that inevitably come to exist only when new surgical techniques are attempted and mastered.

.jpeg)


_scan_of_a_right_shoulder._this_mri_scan_demonstr.png)





_and_scapular_y_radiograph_of_a_right_shoulder_status_post_arthros.png)
.jpeg)



_scan_of_a_right_shoulder._this_mri_scan_demonstr.png)






_and_scapular_y_radiograph_of_a_right_shoulder_status_post_arthros.png)