Introduction
Total knee arthroplasty (TKA) in the setting of arthrofibrosis or the preoperatively stiff knee can present a set of difficult problems that challenge both the patient and surgeon (Aglietti et al. 1989). It has been demonstrated that one of the most important predictors of post-operative range of motion (ROM) is preoperative ROM. Therefore, these patients are inherently at risk for worse outcomes (Gatha et al. 2010; Ritter et al. 2003). With approximately 70° of knee flexion needed to perform the swing phase of the gait cycle, 90° for descending stairs, and approximately 110° for cycling, limited knee ROM can severely inhibit functionality for basic activities (Hsu et al. 2012). Multiple approaches for exposure of the stiff knee have been described (Barrack 2000). However, extensile approaches have been associated with inferior clinical outcomes (Hsu et al. 2012). Despite these challenges, outcomes of TKA in the stiff knee are generally considered good as patients have significant recovery in pain scores, ambulatory status, and in ROM compared to their debilitated preoperative status (Choi et al. 2020).
The literature is sparse regarding the utilization of robotic assisted surgery in the context of the preoperatively stiff knee. Prior literature has demonstrated the utility of robotic-assisted TKA (raTKA) to reduce alignment outliers and improve gap balance postoperatively compared to conventional TKA (Song et al. 2013). However, this has been described in the context of knee deformity rather than stiffness. raTKA may allow the surgeon to achieve balance and appropriate ROM more often with bony cuts alone, rather than with soft tissue releases which have been associated with worse patient reported outcomes (Vigdorchik et al. 2022).
Here, we report a case of a patient undergoing primary TKA with severe osteoarthritis (OA) and severely limited preoperative ROM of only 5 degrees. The use of a modern FDA-approved robotics system in conjunction with a dynamic gap balancing software allowed us to determine the degree of residual soft tissue tightness following bone preparation and prevent extensive soft tissue releases, resulting in correction of the patient’s preoperative deformity and restoration of ROM.
Case Report
A 71-year-old female with a past medical history of rheumatoid arthritis (RA) and bilateral hip replacements presented with three years of right knee pain and stiffness. Prior to initial presentation, the patient sustained a patellar dislocation that was closed reduced, and treatment in a knee immobilizer for two weeks. Subsequently, the patient developed marked stiffness and pain that significantly affected her quality of life. She was managed conservatively with anti-inflammatory medications, physical therapy, and multiple intra-articular steroid injections for three years. She actively participated in preoperative physical therapy, but failed to achieve significant functional improvement in pain or range of motion.
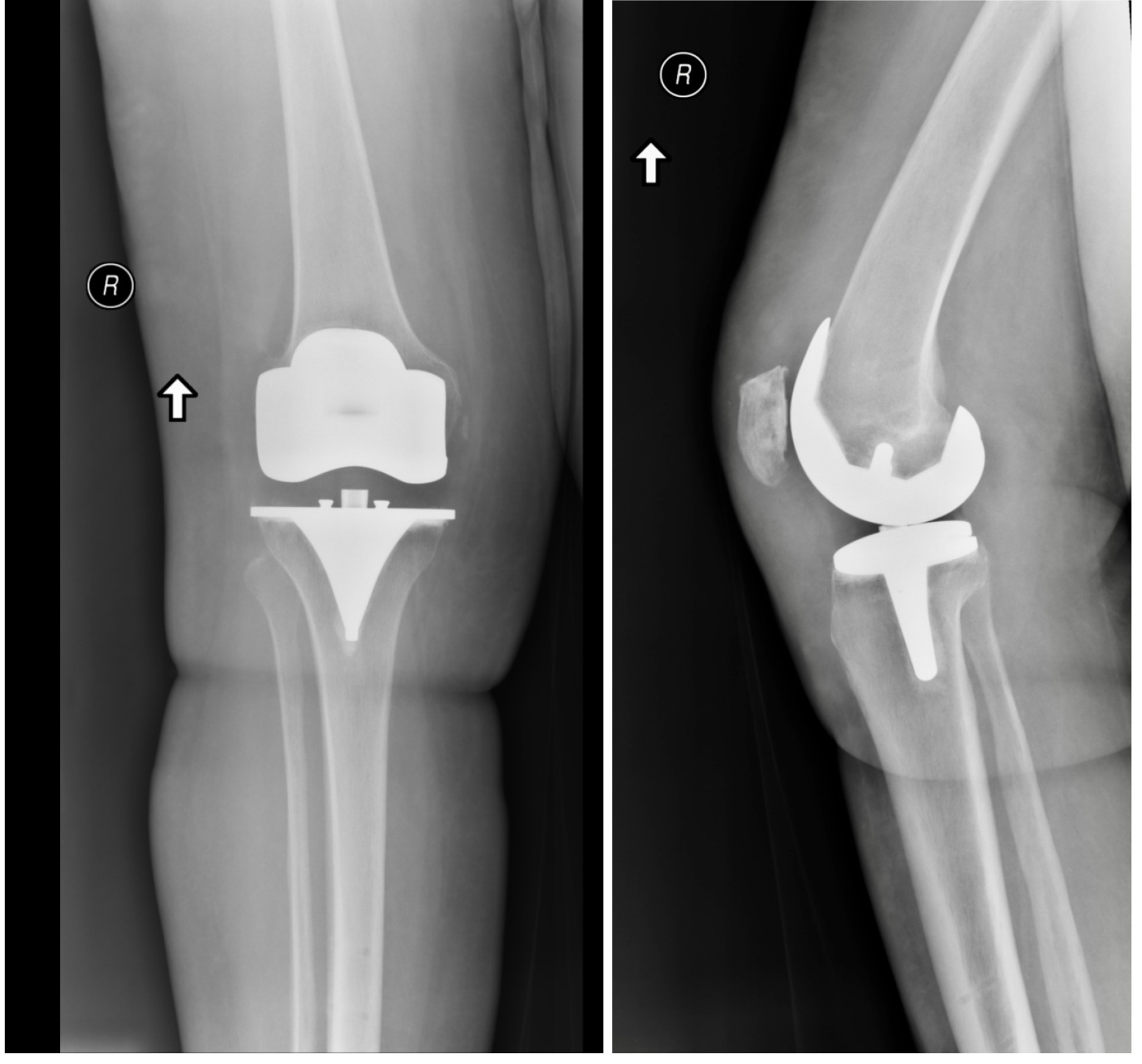
On physical exam of the right knee there was a valgus deformity and extreme stiffness, with a range of motion (ROM) of 0 to 5 degrees. She could walk short distances with substantial discomfort. She otherwise had full painless range of motion of both hips and the left knee. AP, lateral, and sunrise radiographs of the right knee (Figure 1) revealed Kellgren and Lawrence grade 4 OA with tricompartmental involvement, marked joint space narrowing with 11° valgus deformity, marginal osteophytosis, and subchondral cystic changes. After failing non-operative measures, she elected to proceed with robotic assisted right total knee arthroplasty.
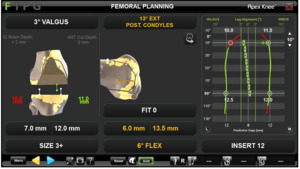
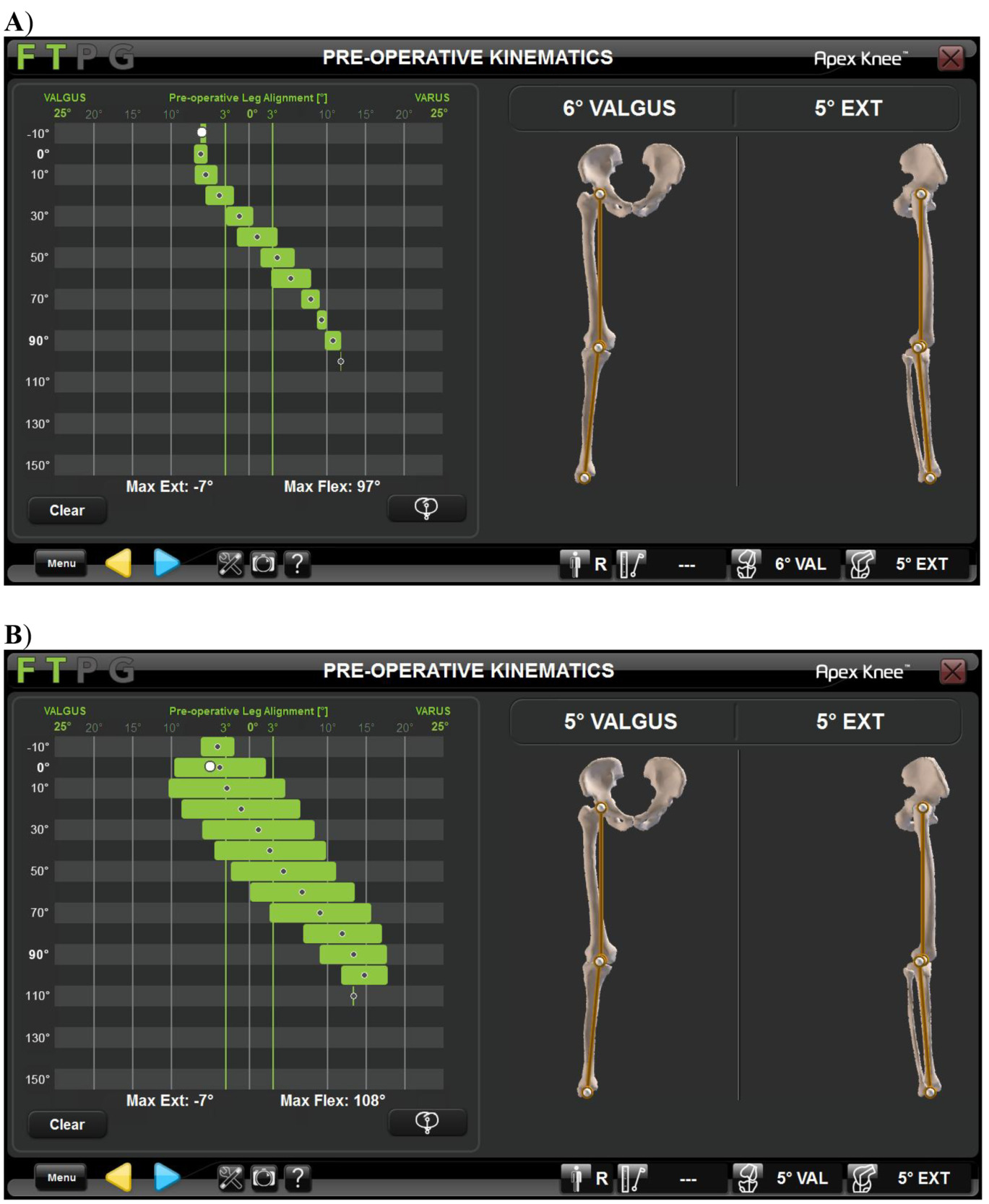
The patient underwent institutional standard perioperative protocol and spinal anesthesia. The right knee was gently manipulated to break up adhesions. After approximately 5 minutes, a range of motion of 0-45 degrees was achieved. A standard medial parapatellar approach was performed with additional release and resection of abundant soft tissue scarring and adhesions. The PCL was resected as a part of the surgeon’s typical operative workflow. Subsequently, the knee was able to achieve a ROM of 0-110 degrees. The OMNIBotics computer navigation system (OMNIBotics Robotic Total Knee Replacement System (OMNIBotics Corin USA, Raynham, MA)), was utilized as previously described (Scanlon, Passano, and Koenig 2022). A short video of the OmniBotic and BalanceBot technique is available at https://vimeo.com/321724524. Pre-resection kinematics were established, defining a final valgus deformity of 6° and range of motion of 0-108 degrees (Figure 2).
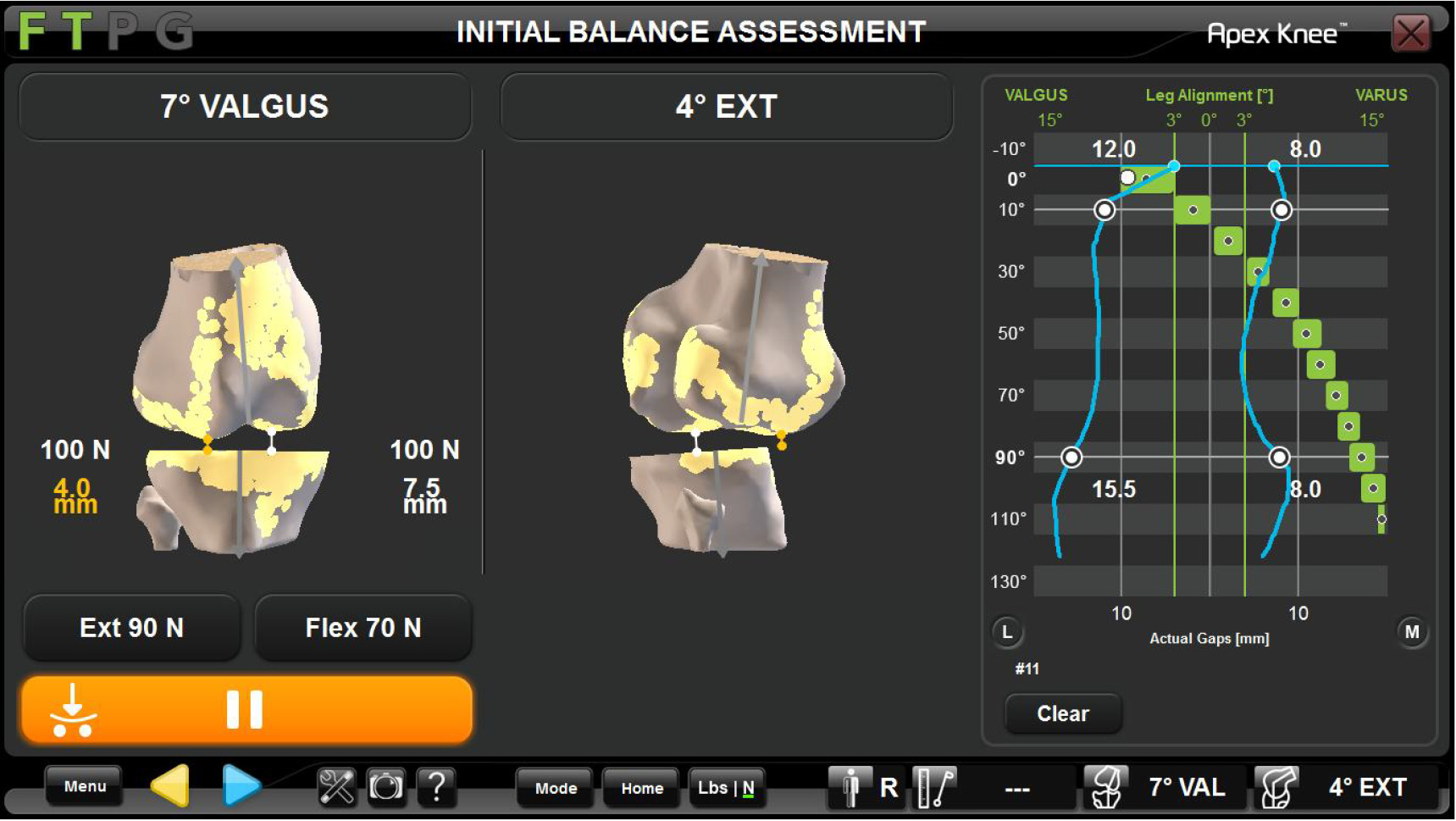
Under intraoperative visualization, the femur appeared significantly internally rotated to about 8 degrees. This was considered and utilizing the Omnibiotics computer navigation system, the components were predictively balanced. Multiple component positions were trialed to attain appropriate balance, ROM, and stability. The predictive gap balancing technology helped determine that placing the femoral component in 13° of external rotation in reference to both the TEA and PCA, and the tibial component with 3° posterior slope allowed for excellent stability throughout range of motion. Therefore, this position was chosen (Figure 3-4). Final bone cuts were measured 6mm for the tibia, 7mm for the lateral distal femoral condyle, 12mm for the medial distal femoral condyle, 6mm for the lateral posterior femoral condyle, and 13.5mm for the medial posterior femoral condyle. The 3+ femoral component thickness measures 9mm distally and 11mm posteriorly.
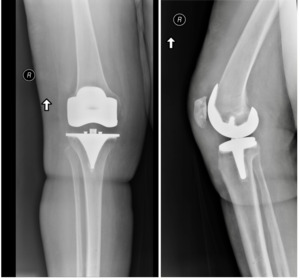
Once the plan was finalized, bone cuts were made and a size 3 tibia, 12 mm ultra-congruent poly, size 3+ femur, and 29 x 8 patella were trialed. Final assessment showed 2-degree valgus alignment and a range of motion 0-141 degrees with excellent stability throughout. Final prostheses were cemented using standard technique and a final range of motion showed 0-141 degrees without any external pressure (Figure 5). The wound was closed in standard fashion and patient was discharged to recovery in stable condition.
Postoperatively, the patient underwent standard postoperative protocols and was discharged to home. In addition, the patient was supplied with a continuous passive motion machine (CPM) with instructions for use 2-4 hours per day set from 0-90° with increasing ROM as tolerated.
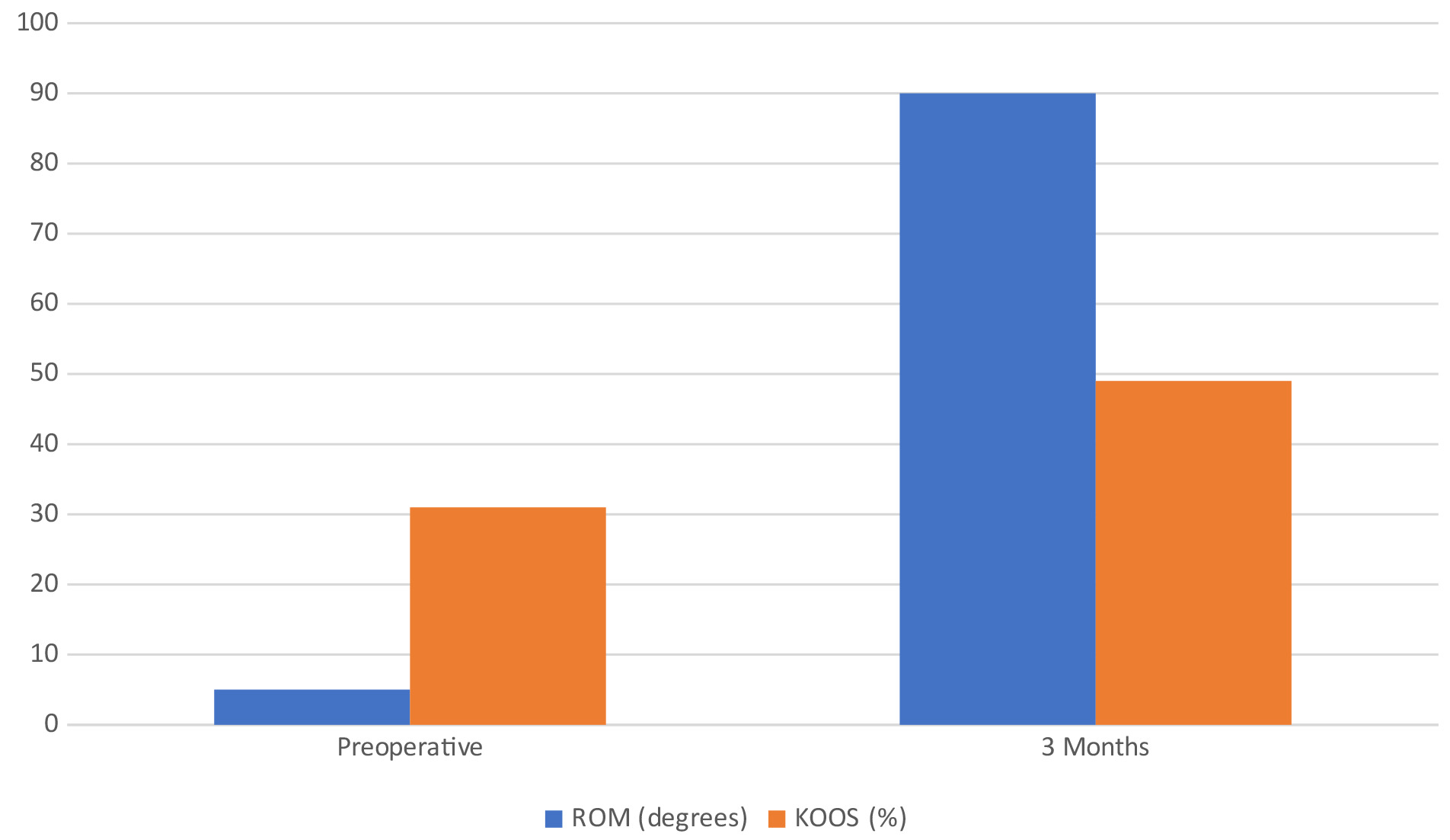
The patient was seen at standard postoperative intervals. After two weeks, active range of motion was 0 to 35 degrees, improving to 0-45 degrees at 6-weeks, and 0-90 degrees at 3 months (Figure 7). She continues working on range of motion, strengthening ambulation and balance, and will return for routine follow ups.
Discussion
The stiff knee, as defined by a ROM less than 50 degrees, can be debilitating for a patient (Aglietti et al. 1989). There are many known causes which are often seen in combination including, but not limited to, severe OA, RA, psoriatic arthritis, complex regional pain syndrome, severe pain, posttraumatic arthritis, neuromuscular disorder, prior infection, and prior surgery (Malkani et al. 2016). While the pathoanatomy of the extension contracture is variable, it is most often multifactorial and can be related to fibrosis and adhesions of the medial and lateral parapatellar retinacula and patellofemoral joint. Intra-articular pathology including adhesions both within and deep to the quadriceps musculature, as well as shortening of the rectus femoris itself, have also been described (Malkani et al. 2016; Bellemans et al. 1996). Attempting TKA with severely limited preoperative ROM can be a technical challenge and lead to a multitude of intraoperative complications including patellar tendon rupture, tibial tubercle avulsion, flexion-extension mismatch, component malposition, and collateral ligament avulsion (Malkani et al. 2016). Difficulty with soft-tissue balancing is also a common challenge with the preoperatively stiff knee. Here, we present a case of a patient with severely limited preoperative knee ROM. We were able to achieve adequate exposure through manipulation and standard medial parapatellar approach. Utilizing raTKA with predictive gap balancing technology, femoral cuts were digitally planned after tibial resection. The femur was noted to have 8 degrees of internal rotation deformity prior to resection. The predictive gap balancing technology allowed the surgeon to digitally manipulate femoral component position and assess resulting stability and ROM. We believe this tool assisted the surgeon in cutting and placing the patient’s femoral component in relative 13 degrees of external rotation for a net 5 degrees external rotation. This allowed the patient to achieve excellent intraoperative ROM and gap balance after final prostheses implantation.
Stiff knees can often require additional exposure techniques to allow for enough access to successfully perform TKA. Multiple techniques exist ranging from the quadriceps snip, V-Y quadriceps turndown, medial collateral ligament slide to the medial femoral peel, medial epicondyle osteotomy, and tibial tubercle osteotomy (Garvin, Scuderi, and Insall 1995; Arsht and Scuderi 2003; Barrack et al. 1998; Whiteside 1995; Whiteside and Ohl 1990). In 2000, Barrack et al described a stepwise extensile approach to the preoperatively stiff knee. It begins with a standard medial parapatellar incision followed by elevation of the MCL subperiosteally. After the medial and lateral gutters as well as the suprapatellar pouch are developed, if ROM is still limited, a lateral release can be performed. Finally, quadriceps snip can be performed, followed by conversion to V-Y quadriceps turndown if necessary (Barrack 2000). As stated above, our patient did not require advanced exposure techniques. However, the surgeon’s preoperative plan was to proceed in a stepwise fashion and to perform V-Y quadriceps turndown if needed.
Despite the challenges in performing TKA in preoperatively stiff knees, results are generally successful in restoring a functional ROM. The risk of residual postoperative stiffness is related to preoperative flexion less than 50 degrees (Aglietti et al. 1989). Our patient only had a 5° pre-operative arc of motion, even after an extensive trial of “Pre-Hab” therapy. Complication rates are significantly higher in these patients, and outcomes are considered worse than TKA in patients with preoperatively flexible knees (Rajgopal, Ahuja, and Dolai 2005; McAuley et al. 2002; Montgomery et al. 1998). Rajgopal et al reported on 84 knees with preoperative stiffness and ROM ranging from 0° to 20°. Authors were able to achieve a significant increase in mean postoperative ROM to 75 degrees with a mean 9-year follow up (Rajgopal, Ahuja, and Dolai 2005). Winemaker et al. compared outcomes in 134 stiff knees with preoperative ROM less than 80 degrees and a matched cohort of non-stiff knees with ROM greater than 100 degrees. The stiff knee cohort experienced a significantly larger improvement in range of motion from baseline when compared with the non-stiff knees. However, the total range of motion achieved was slightly less. There were similar reported outcome scores with regards to both groups (Winemaker et al. 2012). Our patient was able to achieve a 12-week ROM of 0-90 degrees with an improvement in their knee injury and osteoarthritis outcome score (KOOS) of 18% over that period (preoperative: 31%, 3-months postoperative: 49%) (Figure 7). Considering the patient’s excellent intraoperative ROM, there is optimism the patient will have continued restoration and maintenance of ROM and quality of life with further therapy.
In addition to more extensile approaches, various surgical techniques have been described to improve patient outcomes in stiff knees. Boettner et al. attempted to address the stiff knee by increasing the flexion gap in posterior stabilized (PS) TKA. They performed 98 TKAs in patients with <80 degrees of preoperative ROM. All patients received PS TKA with 2mm increased flexion gaps. They found mean ROM increased from 67 degrees preoperatively to 114 degrees post operatively (p<0.001), with no reported flexion instability (Boettner et al. 2020). Multiple additional studies have suggested increased ROM and higher outcome scores with increased flexion gaps (Higuchi et al. 2009; Ismailidis et al. 2016; Matsumoto et al. 2017); however, they did not specifically investigate preoperatively stiff knees. Similarly, in our case, a slightly larger flexion gap, by 1-2 mm, was planned and executed with raTKA. Furthermore, we utilized a dynamic gap balancing tool in conjunction with raTKA. The gap balancing tool allows surgeons to determine the degree of residual soft tissue tightness following bone preparation and guide performance of titrated soft tissue releases if needed. This can result in correction of the patient’s preoperative deformity and restoration of ROM, which can be verified and validated in real time prior to implantation of the final components. Regarding the current case, the gap balancing tool helped establish the patient’s virtual bony cuts and balance, including cutting the femur in 13 degrees of external rotation, without necessitating further soft tissue releases. To our knowledge, increasing femoral external rotation to increase ROM in a preoperatively stiff knee has not been previously described and is more likely directly related to her preoperative deformity than her stiffness. However, it is difficult to extrapolate to subsequent patients.
To the authors’ knowledge, the use of robotic-assisted TKA (raTKA) to address the preoperatively stiff knee has not been specifically addressed in the literature. It has been suggested that the use of raTKA has reduced post-operative stiffness and rates of manipulation under anesthesia (MUA) (Malkani et al. 2020; Dabuzhsky, Neuhauser-Daley, and Plaskos 2017). However, outcomes of raTKA in preoperatively stiff knees have not been reported. It is possible this result could have been achieved via manual instrumentation; however, the authors believe the use of robotic assistance in conjunction with a predictive gap balancing tool allowed the surgeon to manipulate femoral bone cuts to generate a reliable, excellent result with a well-fitting and appropriately balanced prosthesis in a stiff knee with marked deformity.
Conclusion
The preoperatively stiff knee presents significant challenges in TKA. We describe the use of raTKA with predictive gap balancing which led to excellent intraoperative ROM and soft tissue balance in a patient with extremely limited preoperative ROM. The use of raTKA in the context of stiff knees has not been previously described. raTKA may offer another strategy to surgeons who face these difficult cases. We recommend further validating research utilizing raTKR in these most challenging cases with pre-operative arthrofibrosis.
Author Bios
Brandon Passano is a orthopedic surgery resident at NYU Long Island.
Conflicts of Interest Statement for Dr. Passano
Jacob Becker is a PGY-4 Orthopedic Surgery Resident at NYU Langone Long Island.
Visit Dr. Becker’s Website
Connect with Dr. Becker on LinkedIn
Conflicts of Interest Statement for Dr. Becker
Visit Dr. Koenig’s Website
Connect with Dr. Koenig on LinkedIn
Visit the Open Payments Data Page for Dr. Koenig
Conflicts of Interest Statement for Dr. Koenig





_final_dynamic_assessment_performed_with_implants_in_place_showed_3-degree_valgusal.png)






_final_dynamic_assessment_performed_with_implants_in_place_showed_3-degree_valgusal.png)