Introduction
It is estimated that in the United States (U.S.) alone, approximately 2.5 million cases of traumatic brain injury (TBI) occur each year. However, this is likely an underestimation, as this number only reflects those patients that presented for clinical care and received an official diagnosis (Voss et al. 2015). It is estimated that 1.6 to 3.8 million sports-related concussions occur in the U.S. per year (Harmon et al. 2012). This discrepancy in reported numbers of TBIs and sports-related concussions reflects the difficulties associated with recognizing, assessing, and managing sports-related concussions. When defining the terms of concussion and TBI, the consensus among experts is that they both represent a change in brain function from a traumatic force (Menon et al. 2010). However, the classic definition of a concussion is a TBI that involves a traumatic force transmitted to the head, face, neck, or elsewhere as a result of a direct head impact or indirect body impact, while a TBI itself is "an alteration in brain function, or other evidence of brain pathology, caused by an external force (Daneshvar et al. 2011). The current definition of a sports-related concussion, according to the Concussion in Sport Group (CISG), is a concussion that involves the following four criteria: 1) A direct or indirect trauma anywhere on the body with a force transmitted to the head; 2) Rapid (seconds to minutes) or delayed (minute to hours) symptom presentation, typically with spontaneous resolution; 3) Negative standard neuroimaging (computerized tomography (CT) or magnetic resonance imaging (MRI)), reflecting a functional rather than structural injury; 4) With or without loss of consciousness, with stepwise resolution of symptoms (McKeithan et al. 2019). One of the overlaps between a sports-related concussion and a TBI is based off the Glasgow come scale (GCS), which classifies the severity score. Where a concussion overlaps with a TBI is based off a GCS score of 13-15, which also equivalates to the score of a mild TBI. While there does exist this overlap between a mild TBI and sports-related concussion, according to the CISG, a mild TBI differs from a concussion because any positive imaging can no longer be classified as a concussion, regardless of whether both of them are classified as having the same severity(McKeithan et al. 2019).
Sustaining a concussion can result in a multitude of physical, cognitive, and psychosocial impairments; however, cognitive deficits have the greatest impact on daily functionality (Kersel et al. 2001). Though evidence suggests that individuals are able to recover from many of these impairments within the first year following concussion (Draper and Ponsford 2008), recovery of complete cognitive capability can take years after the initial injury depending on the severity (Kennedy, Clement, and Curtiss 2003; Ruttan et al. 2008; Whitnall 2006).
Cognitive deficits, which is the impairment of an individual’s mental processes that lead to knowledge, include multiple, broad domains such as attention, verbal and visual memory, visual perception, and executive function (Ashton, Donders, and Hoffman 2005). Each domain is further categorized into individual elements. Previous studies on impairment in attention following concussion demonstrate that several sub-types of the domain are commonly impaired, including focused attention (ability to maintain attention despite surrounding distractions), sustained attention (attention sustained over a duration of time), selective attention (attention devoted to one singular object and/or task), divided attention (ability to maintain attention on multiple objects and/or tasks), and alternating attention (ability to alternate attention between multiple objects and/or tasks) (Slovarp, Azuma, and LaPointe 2011; Vakil 2005). Similar to the findings on attention, multiple studies have found impairment in the domains of verbal and visual memory following concussion (Ashton, Donders, and Hoffman 2005; McKenna et al. 2006; Schwarz, Penna, and Novack 2009). While not as much research has focused on the cognitive domain of visual perception, at least one recent study has demonstrated an impairment of visual perception following concussion (Henry and Crawford 2004). The executive functioning domain is of particular importance, as measures of executive functioning have been found to be strong predictors of functional outcome (Henry and Crawford 2004). The most studied subtype of executive functioning, verbal fluency, has been consistently found to be impaired in patients with a concussion (Henry and Crawford 2004). In a meta-analysis by Henry et al. that examined 30 studies published between 1986 and 2002 with the purpose of assessing verbal fluency following concussion, the authors found that patients in the concussion group performed significantly worse on tests of verbal fluency compared to non-concussion controls (Henry and Crawford 2004).
The majority of published research on cognitive deficits following concussion has focused on examining these deficits at specific time points (e.g., days, weeks, months, or years post-injury). There is a paucity of research that has collectively analyzed cognitive deficits across multiple time points with a broader perspective on the overall effects since initial concussion. As such, the purpose of this study was to examine cognitive deficits following concussion/TBI in the acute, intermediate, and long-term time period after sports-related concussions. We hypothesized that all cognitive deficits examined would be functionally worse in patients with a concussion in the acute period and that, despite cognitive functionality improving in the intermediate and long-term period, deficits would persist.
Methods
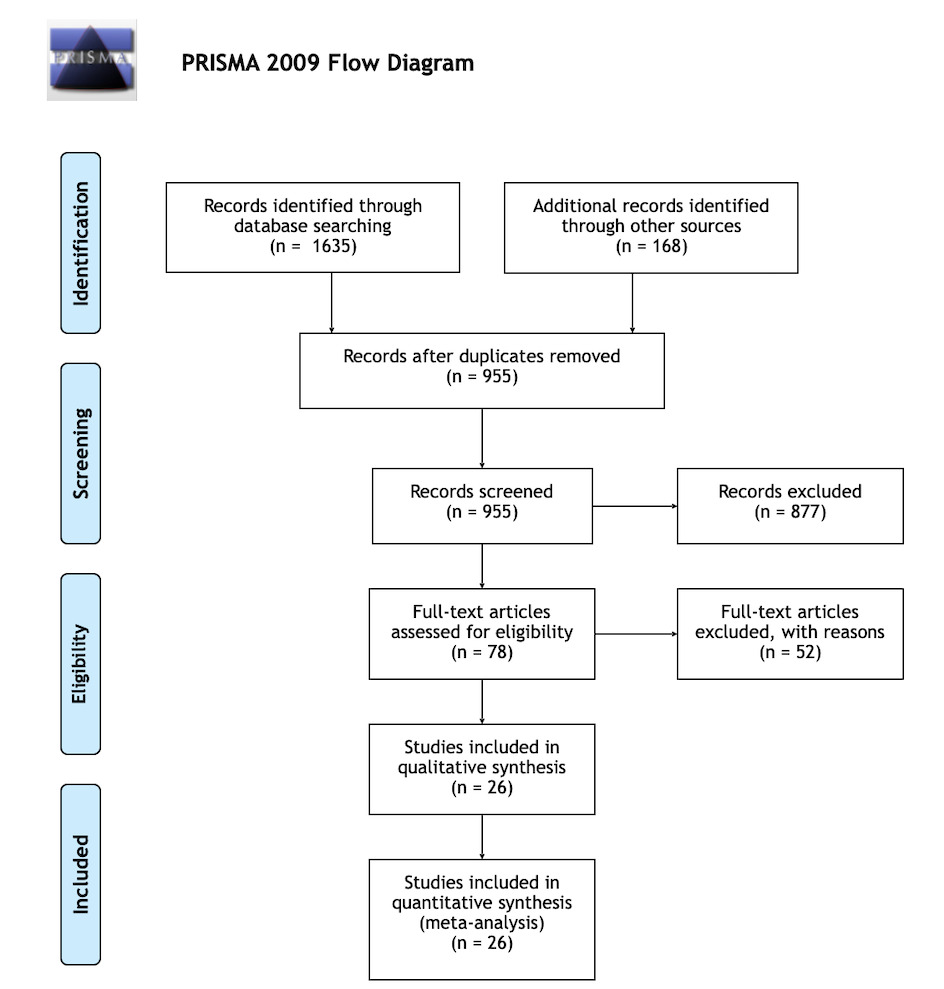
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Review (PRISMA) guidelines (Page et al. 2021). Three separate search engines were used: Pubmed, Psychinfo, and Web of Science. Articles written in the English language only were acquired from the inception of the database to February 2022, and were considered for inclusion. Search terms included: (“recovery of function” or “symptom” and “resolution” or “improvement” or “symptom improvement”) and (“mild” or “moderate” and “closed head injury” or “traumatic brain injury”) or (“contrecoup injury” or “brain concussion”) or (“post-concussion syndrome”) and (“cognitive dysfunction(s)”).
Each of the articles considered for this study were extracted using EndNote (Philadelphia, PA). Duplicates were removed. Titles and abstracts were screened by two of the co-authors (L.K.C, S.A.O) based on the inclusion and exclusion criteria. Studies were included if they met the following criteria: 1) focused primarily on cognitive deficits, 2) clearly stated time points (e.g., days, weeks, months, years) following the injury, 3) provided explanations of the severity of the participant’s injuries, and 4) written in the English language. Studies were excluded if they 1) were based solely on subjective measures of cognitive impairment (questionnaire-style study), 2) measured non-cognitive deficits (skull fractures) only, 3) were single case reports, 4) were systematic reviews, or 5) were studies with nonhuman subjects. The remaining articles underwent a full-text screen by the same two co-authors. Data was reviewed to provide a qualitative review. For each article that met the inclusion criteria, the risk of bias was independently rated by two authors using the Cochrane Risk of Bias template, which was aimed at determining any biases in sequence generation, allocation concealment, blinding of participants, blinding of outcomes, assessing any incomplete outcomes, outcome reporting, and any other sources of biases that may have been evident.
The selected studies all examined cognitive deficits across different time periods, ranging from a few days to multiple years following sport-related concussion. In order to properly assess the overall effects of concussion on cognitive deficits, the articles included were divided into three time periods. The acute period examined cognitive deficits at 1-14 days following concussion, the intermediate period examined cognitive deficits from two weeks to 1 year following concussion, and the long-term period examined cognitive deficits greater than 1 year post concussion. The following information was also extracted from each of the studies: male:female ratios, average age, and athletic status of the participants.
Results
After the initial database search, 1,635 studies were identified and 168 additional records were screened from the reference lists of those studies. After removing duplicates, 955 studies remained. 877 were excluded based on title and abstract, leaving 78 articles that underwent full text review. Twenty-six (26) studies met all criteria and were included. Figure 1 demonstrates the database search and screening process. Using the Cochrane Risk of Bias template, it was determined that 0 of the 26 studies displayed risk of bias.
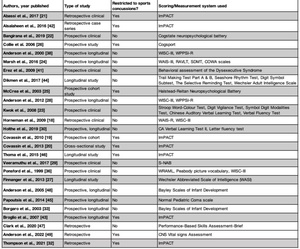
A total of 4,534 patients were involved in the studies. 84.5% (3831/4534) of patients were male, the average age was 21.0 years, and 64.5% (2925/4534) were athletes at either the high school, collegiate or professional level. Ten of twenty-six (38.4%) studies were separated into control groups versus concussed groups, while nine of twenty-six (34.6%) compared baseline scores to post-injury scores. Four (15.4%) focused on the initial injury’s severity, based on whether patients lost consciousness following the head trauma; three (11.5%) focused on patients with complicated versus uncomplicated concussions, and one (3.8%) study separated patients into symptomatic versus asymptomatic groups. Ten of 26 (38.5%) studies were solely restricted to sports related concussions, of which 7 (26.9%) used the Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT) scoring system (Table 1). Sixteen of 26 (61.5%) studies examined concussions following trauma to the head in a setting besides sports (e.g., automobile accidents) or included concussions caused by sports-related injuries plus another traumatic setting. The Glasgow Coma Scale (GCS) was also used in 8 (30.7%) of these studies to measure severity of injury.
Twenty-five of 26 (96.1%) included studies noted the presence of cognitive deficits at some time point following a concussion (Table 2). During the acute time period (i.e., 1–14 days post-concussion), patients experienced impairments in verbal memory, visual memory, speed of processing, verbal comprehension, perceptual organization, and attention. In the intermediate time period (2 weeks–1-year post-concussion), impairments were seen in visual attention, sustained attention, working memory, psychomotor speed, and executive function. During the long-term period (>1-year post-concussion), impairments could still be seen in executive function, intellectual ability, verbal comprehension, verbal memory, attention, visuo-spatial construction, and processing speed (Table 3). Horneman et al. evaluated children and adolescents 10 years after initial concussion as a result of motor vehicle accidents, sports, or injury from falls and found that this group had lower values in verbal learning and memory, visuospatial memory testing, and verbal processing speed compared to uninjured control subjects who were matched for both age and sex (Horneman and Emanuelson 2009). These patients also showed impairments in executive function (i.e., attention, working memory, and mental flexibility), as well as in verbal intelligence and verbal processing capacity compared to controls.
In 2010, Covassin et al. evaluated verbal and visual memory, processing speed, and reaction time 3- and 10-days post-concussion in 76 high school athletes participating in baseball, softball, basketball, cheerleading, football, gymnastics, hockey, soccer, and wrestling (Covassin, Elbin, and Nakayama 2010). The authors found deficits in reaction time, verbal memory, and motor processing speed. Additionally, they noted that it took, on average, 21 days to return to baseline measurements (Covassin, Elbin, and Nakayama 2010). A 2013 study by Covassin et al. evaluated cognitive deficits 3- and 10-days following injury in 165 high school and collegiate athletes participating in a variety of sports (football, softball, baseball, softball, volleyball, cheerleading, lacrosse and ice hockey) (Covassin, Crutcher, and Wallace 2013). The authors found that athletes experience cognitive deficits in visual memory and motor processing speed 3 days post-concussion and verbal memory and reaction time 10 days post-concussion (Covassin, Crutcher, and Wallace 2013).
In 2017, Abbassi et al. used the ImPACT test to evaluate both male and female high school athletes participating in the sports of football, ice hockey, basketball, and softball and found that 20% of those that experienced a concussion still had deficits in at least one cognitive domain 15 days post-injury (Abbassi and Sirmon-Taylor 2017). Bangirana et al. evaluated cognitive domains 6 months post-concussion injuries as a result of motor vehicle accidents and accidental trauma (Bangirana et al. 2019). This study focused on patients ages 1–69 and found that 8 of 81 (9.9%) patients with concussions displayed deficits in psychomotor speed, 1 (1.2%) patient had deficits in both visuo-motor skills and visual learning and memory, 13 (16%) had deficits in visual attention, 6 (7.4%) had deficits in working memory, and 4 (4.9%) had deficits in spatial problem solving (Bangirana et al. 2019).
In 2008, Kwok et al. studied cognitive deficits three months after an initial concussion in 31 patients ages 18–65 and found that overall cognitive functions were impaired in patients with mild concussion compared to non-concussion patients with respect to processing speed, attention, memory, and executive functions (Kwok et al. 2008). Further, a study by Marsh et al. evaluating cognitive deficits in adults 5 years post-concussion found that 28 of 71 (39%) patients had impairments in attention and 32 (45%) in verbal memory (Marsh, Ludbrook, and Gaffaney 2016). These deficits were least evident in immediate memory, seen in only 16% of patients (Marsh, Ludbrook, and Gaffaney 2016). McCrea et al. evaluated cognitive function in over 1,600 collegiate football players following concussions and found that cognitive impairment was most severe at the time of injury. Less severe deficits persisted five days post-injury and resolved, on average, by day seven (McCrea et al. 2003).
In addition to studying the presence of symptoms following a concussion, some of the included studies evaluated cognitive deficits when a patient was still reporting symptoms of concussion versus asymptomatic subjects. Collie et al. found significant differences among injured Australian footballers in reaction time, divided attention, and learning and memory accuracy in those reporting symptoms 11 days after the initial evaluation, while the asymptomatic athletes had deficits only in divided attention in the 11 days following their injury (Collie 2006).
Other studies separated the groups based on injury severity using the GCS (Finnanger et al. 2013; V. Anderson et al. 2012). Finnanger et al. demonstrated that at 12 months post-concussion in both adolescent and adult patients, those with moderate GCS scores (9–13) performed significantly worse than controls on executive function only (Finnanger et al. 2013). Patients who scored severely (GCS 3–8) performed worse than controls on the motor function, processing speed, verbal memory and executive function domains. Anderson et al. evaluated children who experienced a concussion from trauma (falls, motor vehicle accidents, sports, etc.) and identified mild cognitive deficits 10 years post-injury, but there was no correlation between the severity of the injury and the cognitive deficits that were recorded (V. Anderson et al. 2012).
Another distinction within the included studies was between complicated (abnormal intracranial findings on CT, such as depressed skull fracture, edema, and hemorrhage) and uncomplicated (normal CT) injuries. Veeramuthu et al. demonstrated that complicated concussions resulted in poorer outcomes with regards to cognitive function 6 months following the injury (Veeramuthu et al. 2017). Significant differences were found in attention, executive function, and overall performance when studying the complicated cases, while only attention and overall performance decreased in those with uncomplicated injuries (Veeramuthu et al. 2017). A 2019 study by Holthe et al. separated patients into complicated vs. uncomplicated groups (based on the presence vs. absence of intracranial findings on MRI or CT) and observed cognitive deficits in both groups (Holthe et al. 2019). However, the authors noted that patients under the age of 40 and those with a lower level of education (under 12 years of education) tended to have less improvement compared to older patients. Younger patients were found to have more pronounced deficits in executive function, which they attest to the possibility that those of an older age may have higher levels of education and higher work demands (Holthe et al. 2019).
Discussion
The main finding of this systematic review was that deficits were seen across all domains of cognitive function in the acute, intermediate, and long-term period following a concussion. Cognitive deficits are more likely to manifest in the acute period following concussion. However, in instances where the concussion is severe, many of these deficits persist for weeks, months, or years. According to Panwar et al., the majority of those who sustain a concussion will typically resolve their symptoms within 1-4 weeks; however, up to 20% of concussion symptoms will persist for longer than 3 months, which is defined as post-concussion syndrome (Panwar et al. 2020). It was also noted in the study by Thompson et al. that retired athletes with a history of concussions were found to have “atrophy of the hippocampus, mild cognitive impairment, depression and poorer self-reported health” (Thompson et al. 2021).
Previous studies have demonstrated that, regardless of the severity, individuals most strongly exhibit cognitive deficits in the acute time period following initial concussion (Borgaro et al. 2003; Macciocchi et al. 1996; Maddocks and Saling 1996; Ponsford et al. 1999). In a year-long study by Slovarp et al., participants who had sustained a severe concussion either via sport, motor vehicle accident, or a violent blow to the head, were compared to those without a concussion and asked to complete two visual tasks that assessed the cognitive domain of attention (Slovarp, Azuma, and LaPointe 2011). The authors found that patients experienced deficits in all subsets of the attention domain for cognitive deficits in the period directly after concussion. Similarly, in a study by Schwarz et al., both verbal and visual memory impairment were evident acutely after a concussion (Schwarz, Penna, and Novack 2009). Henry et al. also demonstrated impairments to domains of executive functioning shortly after sustaining a concussion (Henry and Crawford 2004), while McKenna et al. demonstrated impairments to the domain of visual perception in the acute period following concussion (McKenna et al. 2006). The current systematic review also demonstrates that the acute period following concussion is the phase in which cognitive deficits are most evident. It is important that physicians take the proper precautions to ensure athletes have a full recovery and avoid allowing athletes to return to sports until they are completely asymptomatic and do not demonstrate any further deficits.
Much of the research regarding cognitive impairments following concussion is focused on the acute time period after initial injury, while fewer studies have evaluated whether impairments continue into the intermediate time period. For athletes that have sustained a more severe concussion, it is much more likely that cognitive deficits will persist beyond 2 weeks (ie the acute period) (Panwar et al. 2020). Borgaro et al. examined cognitive abilities in 28 patients at 40 days post-concussion and found that for those who were classified as having a “complicated” concussion (i.e., showing evidence of intracranial brain pathology), deficits still existed for the cognitive domains of speech/language, attention/concentration, and visuo-spatial awareness (Panwar et al. 2020). While our systematic review found similar deficits to those by Borgaro et al., additional cognitive deficits in the intermediate period following concussion were seen in the domains of psychomotor speed and executive function.
While many of the symptoms and cognitive impairments in patients with a concussion resolve well before 1-year following a concussion, those with a moderate to severe concussion will often experience long-term residual impairments (V. Anderson et al. 2000; Holthe et al. 2019). Jonsson et al. evaluated 8 patients who had sustained a severe concussion at a mean age of 14 years old (Jonsson, Horneman, and Emanuelson 2004). The authors found that at 1-, 7-, and 14-years post-concussion, patients continued to show impairment in attention, working memory, and verbal learning. They concluded that sustaining a concussion at an earlier age was associated with longer term impairment (i.e., more likely to have persistent deficits up to 14 years post initial concussion), which was likely due to early brain damage limiting the formation of new cognitive intelligence/products over a person’s growth span (Jonsson, Horneman, and Emanuelson 2004). A similar study by Jaffe et al. evaluated 3-year neuropsychological recovery in children who sustained a severe concussion (Jaffe et al. 1995). The authors found that, although there was recovery of cognitive functionality, those who sustained a severe concussion still exhibited deficits in the domains of executive function, attention, and memory. The articles in this systematic review support much of the previous research on concussion. Severity of concussion has the most significant impact on the occurrence and duration of cognitive impairments across a variety of cognitive domains. Cognitive deficits are most severe in the acute period following severe concussion and can persist in the weeks, months, and years afterwards. Additionally, studies have observed the etiology of post-concussive syndrome, which is defined as concussion symptoms lasting longer than 3 months, being linked to female gender, younger age, psychiatric history or a previous diagnosis of chronic pain syndrome (Permenter, Fernández-de Thomas, and Al 2022). With these considerations and the present study’s findings, a patient who is diagnosed with post-concussive syndrome is more likely to experience cognitive deficits including attention, verbal memory and executive function. As a medical provider, it is important to take into consideration these findings to better develop post-concussion and neurological rehabilitation for patients.
There are several limitations to this study. First, some relevant studies could have been excluded during screening despite the authors’ best efforts to include all appropriate search results. Additionally, it is possible that there were other neurocognitive domains discussed in the excluded studies, besides the selected ones for this study. Second, in the studies included, there were inconsistencies in the cognitive deficits that were examined during each of the time points. In the acute period (1–14 days post-concussion), 10–14 different cognitive domains were studied. However, in intermediate (2 weeks–1-year post-concussion) and long-term (>1-year post-concussion) periods, the number of domains evaluated was reduced to 3 (executive function, attention, and memory) in many of the studies. Therefore, it’s difficult to determine if all cognitive deficits witnessed in the acute period following concussion continue in the intermediate and long-term. Finally, there was variability in the methodology of the included studies, which limited the ability to compare some of the results and develop a meta-analysis.
Conclusion
Cognitive deficits were seen across all the domains in the acute, intermediate, and, in more severe cases, long-term time periods following an initial concussion. Based on the included studies, a sports related concussion could result in cognitive deficits in the domains of visual memory, verbal memory, processing speed, executive function, and reaction time. This study also demonstrated that most athletes typically experience cognitive deficits for only days to weeks following a sports related concussion, but symptoms can continue to be present for months or years following the injury, which could be attributed to severity of injury or multiple concussions. This understanding, especially in regard to the severity of each injury, should be taken into consideration when determining a return-to-play protocol for each athlete. By understanding that symptoms and cognitive deficits following concussions are highly variable, physicians and athletic trainers could develop more individualized return-to-play schedules for athletes.


.jpeg)





.jpeg)