Introduction
Traumatic proximal tibiofibular joint (PTFJ) dislocation is a rare knee injury, constituting less than 1% of all injuries to the knee (Harvey and Woods 1992), predominantly due to the inherent stability of the articulation (Aladin, Lam, and Szypryt 2002). The PTFJ is a plane type synovial joint composed of the tibial facet on the posterolateral aspect of the tibial condyle and the fibular facet on the medial upper surface of the head of the fibula (Sarma, Borgohain, and Saikia 2015). This stability is most prominent during extension of the knee; an unstable knee is seen when the joint is held in flexion with the foot internally rotated and plantarflexed, and it is in this position that dislocations of the PTFJ typically occur (Giachino 1986). Most often, the posterior proximal tibiofibular ligament is ruptured, while the lateral collateral ligament and the biceps femoris tendon are not involved (Oksum and Randsborg 2018). This case report is unique in that the lateral collateral ligament also required surgical repair this patient. In 1974, Ogden defined the primary function of the joint as dissipation of lateral tibial bending moments and tensile, rather than compressive, weight bearing (Ogden 1974b). Ogden also described a classification for pathologies of the PTFJ which includes subluxation (Type I), anterolateral dislocation (Type II), posteromedial dislocation (Type III), and superior dislocation (Type IV) (Ogden 1974b). Type II is the most frequently documented injury of this classification, accounting for roughly 85% of cases, and is often associated with ligamentous injury and peroneal nerve palsy (Sarma, Borgohain, and Saikia 2015). Type III is associated with a direct blow to the fibula head, whereas Type IV is almost always associated with a tibial shaft fracture (Aladin, Lam, and Szypryt 2002). A significant amount of force is often necessary to cause a dislocation of the PTFJ, and as such, PTFJ dislocations are often associated with other potentially distracting injuries, which may contribute to the relatively low rate of recognition and diagnosis. A systemic review by Rajan et al. found that PTFJ dislocation had a high rate of associated open fractures (70.6%) – similar to the 76.7% rate found by Herzog et al. – vascular injury (29.4%), and preoperative peroneal nerve deficit (41.2%) (Rajan, Ramski, and Romeo 2022; Herzog, Serrano-Riera, and Sagi 2015), all of which are characteristic of high-energy, limb-threatening injury. The PTFJ dislocation in this case was consistent with an Ogden Type III dislocation, which occur in 10% of PTFJ dislocations and as stated above, are most often the result of direct trauma to the fibular head (Aladin, Lam, and Szypryt 2002; Ogden 1974a). The diagnosis of acute PTFJ dislocation is primarily a clinical one, and should be considered in any patient presenting with acute-onset lateral knee pain after an aggressive torsional or direct-impact trauma to a flexed knee (Van Seymortier et al. 2008).
As of yet, there is no published definitive algorithm concerning detailed management of PTFJ dislocations. Attempted closed reduction has been described as an initial approach for a majority of cases for Ogden Types I and II dislocations (Aladin, Lam, and Szypryt 2002), whereas open reduction internal fixation is often the initial course of action for Ogden Types III and IV dislocations (Van Seymortier et al. 2008). This case report describes the method of internal syndesmotic fixation of the PTFJ with two Arthrex Tightropes and primary repair of the LCL using 4.75 SwiveLock anchor following ORIF of the tibia with a Stryker T2 alpha tibial intramedullary nail (IMN). Particular attention is brought to the orientation of the TightRopes fixation in order to achieve ideal PTFJ relocation.
Case Report
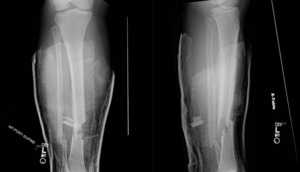
The patient involved in this case was a 23-year old male with no previous past medical history. He was brought to the emergency department via ambulance after a motorcycle crash during which he was struck by a car traveling roughly 60 miles per hour. The patient stated that he flipped over the bike and landed on his right leg with immediate pain, deformity, and bleeding. In the emergency department he was found to have an open right tibia fracture, at which time the orthopedics department was consulted. Two wounds were identified over the anterior aspect of the midshaft of the tibia. An additional open wound was identified over the posterior aspect of the tibia measuring approximately 1 cm x 5 cm in the horizontal direction. Patient was noted to have deficits in sensation and motor in the common peroneal nerve (CPN) distribution with 3/5 motor and 1/2 sensation responses. Dorsalis pedis and posterior tibial pulses were palpated and 2+ with cap refill less than 2 seconds. The compartments remained compressible and pain was well controlled. Imaging following reduction and immobilization demonstrated displaced distal one-third shaft fractures of the tibia and fibula (Fig. 1, Fig, 2).
Within 24 hours, the patient underwent ORIF of the tibia with a Stryker T2 alpha tibial nail (11 mm x 360 mm). Intraoperatively, significant laxity of the PTFJ was noted, and postoperative x-rays of the knee confirmed posterior, medial, and distal migration of the fibular head consistent with Type III PTFJ dislocation (Fig. 3, Fig. 4). As PTFJ dislocation was not recognized pre-operatively, and was thus not addressed in operative planning, it was determined that the best course of action for the patient was to return to the operating room for surgery at a subsequent date, which was done on post-op day 4 from the initial surgery. Prior to the second surgery, the patient was noted to still have a 3/5 motor and 1/2 sensory exam to the CPN distribution.
The patient was brought to the OR, where he was prepped and draped in the normal sterile fashion. Once dissected to the proximal fibula, there was noted to be significant soft tissue disruption at the PTFJ with the fibular head displaced posteromedially approximately 3 cm. The popliteus and biceps femoris tendons were identified and found to be intact. The lateral collateral ligament was avulsed off of its fibular insertion, making this an atypical presentation of a PTFJ dislocation (Oksum and Randsborg 2018). At this time, careful dissection was performed in order to identify the common peroneal nerve (CPN). The CPN was carefully dissected then tagged with a single vessel loop for easy identification and visualization throughout the case. The CPN was determined to be under a significant amount of tension with the posteromedial dislocation of the proximal fibula. This tension appeared to significantly relax after the PTFJ was manually reduced. Proper identification and protection of the nerve was done diligently, as there have been reports of postoperative common peroneal nerve palsy in patients preoperatively neurologically intact (Rajan, Ramski, and Romeo 2022).
With the nerve protected, open reduction of the proximal tibiofibular joint space was performed using manual manipulation and a large pointed reduction clamp. This reduction was provisionally held with a 2.6 mm K-wire, which was oriented by starting the guidewire posterolaterally on the fibular head and ending anteromedially on the tibia, staying orthogonal in order to create a fixation perpendicular to the anatomic alignment of the PTFJ. Two guidewires were then placed as stated above in a parallel fashion. A cannulated drill was used to drill through all four cortices along the guidewires, after which two Arthrex TightRope fixation devices were placed. A separate medial incision was made to assist with flipping of the tightrope buttons on the medial tibial cortex to assure that they sat flush without irritation of the pes anserine. Once both buttons were confirmed to be flipped and flush with the medial tibial cortex, the tightropes were tightened to the fibula, after which the 2.6 mm provisional K-wire was removed. Fluoroscopy was utilized one additional time to confirm an adequate reduction of the PTFJ and proper placement of the TightRope buttons. A #2 FiberWire was used to perform a Krackow stitch to the lateral collateral ligament. The #2 FiberWire was secured to the proximal aspect of the fibula using a 4.75 Arthrex SwiveLock. The wounds were copiously irrigated and closed in a layered fashion using 0 Vicryl, 2-0 Vicryl, and staples, then dressed with Xeroform, gauze, and Tegaderms. The patient was afterwards placed into a knee immobilizer to be locked in full extension for 4 weeks, followed by physical therapy. On postoperative day 1, the patient was noted to have improvement to 4/5 motor and 2/2 sensation to the CPN distribution. On postoperative day 8, the patient had full return of motor and sensation in the CPN distribution.
DISCUSSION
Proximal tibiofibular joint dislocation is relatively rare, as too is literature concerning operative management. Nunes et al. published a 2019 case report detailing open fibular head reduction followed by temporary PTFJ fixation with a K-wire, which was later removed after a 5-week non-weightbearing period with full return to function after a 3-month period (Nunes et al. 2019). Oksum et al. described internal fixation of the PTFJ with open direct repair of the posterior ligamentous structures and syndesmotic stabilization with a dynamic suture button (Arthrex TightRope) (Oksum and Randsborg 2018), though this differed from this case report in that the fixation was not performed following tibial intramedullary nail (IMN) fixation. Additionally, these authors utilized two instead of one tightrope devices. Oksum described that fixation should be directed in a posteroanterior direction towards the anteromedial aspect of the tibia, which these authors agree with (Oksum and Randsborg 2018). Moscon et, al similarly described flexible syndesmotic fixation with a single Knotless Syndesmosis TightRope (Moscon et al. 2018), though again not acutely following fixation with a tibial IMN. Okoroha et al. presents a similar case report in which two suture buttons were placed in the presence of a tibial IMN (Okoroha et al. 2018), though specifications on the direction of fixation were not included. These authors agree with Oksum’s description of fixation of the fibular head in a posteroanterior direction towards the anteromedial aspect of the proximal tibia, though we believe adding an additional caudal to cephalad direction in the TightRopes to provide orthogonal fixation across the PTFJ is ideal, and should be further investigated with biomechanical studies. We also agree with Oksum that, despite the producers of the TightRope advocating that PTFJ fixation should be achieved with both two diverging TightRope implants along with an additional syndesmotic screw, fixation with a screw is too rigid of a construct to allow for optimized joint motion and may result in screw loosening or breakage. Additionally, the use of a screw may require a future surgical procedure for removal. These assertions are consistent with findings of a 2018 cadaveric study that found that repair with a bicortical suspension device is sufficient in restoring PTFJ articulation and motion (Pessoa, Alves-da-Silva, and Guerra-Pinto 2018). The complimentary movement of the PTFJ during ankle motion should also be considered when choosing fixation methods (Pessoa, Alves-da-Silva, and Guerra-Pinto 2018), and though specified at another joint, the use of syndesmotic TightRope fixation has been found to demonstrate similar efficacy to screw fixation at the distal tibiofibular joint without the potential adverse effects of screw fixation (eg, increased risk of the need for hardware removal) (Schepers 2012; Rigby and Cottom 2013).
A high index of suspicion is necessary to identify and address PTFJ dislocations. It speaks to the underrecognized nature of this type of injury that, in this case, it was first noted during surgical fixation of an associated fracture, which necessitated a second surgery. This case report, and future publications on this topic, will help bring awareness to an underrecognized and underdiagnosed joint pathology. It is our hope that future patients will benefit from receiving more thorough care and avoidance of additional surgeries, and that the described alignment of joint fixation will decrease the potential for chronic morbidity.


.jpeg)






.jpeg)





