Introduction
It is predicted that greater than 70,000 revision total hip arthroplasties (THAs) will be performed in the United States by 2030 (Schwartz et al. 2020). These cases are often challenging with higher complication rates compared to primary THA (Badarudeen et al. 2017a). Uncemented diaphyseal engaging femoral stems may be required due to significant proximal femoral bone loss and/or periprosthetic fracture (Aribindi et al. 1998). Modular stems allow for increased rotational control and more options to correct for bone loss, offset, and leg length discrepancies (Wirtz et al. 2014; Mertl and Dehl 2020).
Radiographic evaluation to assess proper sizing and monitoring of uncemented diaphyseal engaging femoral stems has not been defined. While several methods have been suggested, these measurements are performed in millimeters (mm), which inevitably vary depending on the length of the femoral stem (D’Ambrosio et al. 2020; Moriarty et al. 2020). Therefore, adjustments are necessary to compare radiographic outcomes between different length diaphyseal engaging femoral stems.
While uncemented diaphyseal engaging modular femoral stems are an important implant option in complex and revision arthroplasty, few studies assess different models of these femoral stems. Therefore, we sought to evaluate the clinical and radiographic outcomes of an uncemented diaphyseal engaging modular femoral stems when used in revision THA.
Methods
Patient Selection
Following institutional review board approval, we retrospectively reviewed 54 patients who underwent rTHA at 2 institutions between August 9, 2012 and December 17, 2017 using the diaphyseal engaging femoral stem of interest. Medical records were reviewed to assess for complications, reoperations, and implant survivorships.
Demographics
Mean age was 66.3 years (range 23-90 years) and 46.30% of patients were female. Mean body mass index (BMI) was 30.1 kilograms per meter squared (kg/m2), and 26 (48.14%) patients required a left rTHA. 21 (38.89%) patients were indicated for rTHA due to aseptic loosening, 18 (33.33%) patients for implant failure, 8 (14.81%) for periprosthetic fracture (7 Vancouver B2 fractures and 1 Vancouver B3 fracture) (Duncan and Masri 1995), and 5 (9.30%) for infection. Preoperatively, 36 (66.67%) hips were classified as a Paprosky 3a and 13 (24.07%) patients were classified as a Paprosky 3b (Aribindi et al. 1998). 8 (14.81%) hips required an extended trochanteric osteotomy for removal of the previously implanted femoral stem. 1 (1.85%) patient was characterized as having osteopenia preoperatively and 1 (1.85%) patient was characterized as having osteoporosis. Mean follow-up was 1.4 years (Table 1).
Implant Studied
All patients were implanted with the Reclaim revision femoral stem (Depuy Synthes, Warsaw, IN). The Reclaim stem is a modular diaphyseal engaging Wagner style femoral revision stem with a grit blast surface for cementless fixation and a plateau spine design for resistance to torque and subsidence. All femoral stems were implanted using powered straight reamers, which has been shown to provide superior torsional strength (Konow et al. 2022).
Radiographic Analysis
Standard anteroposterior radiographs of the pelvis and lateral radiographs of the hip were obtained in the immediate postoperative period and at each follow up visit. Radiographic assessments compared the position of the components in the immediate postoperative period and the most recent follow up. Magnification error was addressed using the known diameter of the femoral head component as reference. Canal fill ratio was calculated based on the technique described by D’Ambrosio et al, by dividing the width of the femoral component by the width of the intramedullary bone canal at the midpoint of the length of the femoral stem (D’Ambrosio et al. 2020). Subsidence and cortical contact were measured based on the techniques described by Moriarty et al for patients with available radiographs (Moriarty et al. 2020). Subsidence was measured as the difference in perpendicular distance from the tip of the greater or lesser trochanter to the shoulder of the stem at two time points. If the bony landmarks were unable to be used for measurement, then a fixed point on the femur was used for reference. Cortical contact was measured as the length of the femoral stem component in contact with the cortical bone divided by the total length of the femoral stem component in the anterior, posterior, lateral, and medial views. For the 48 patients with available anteroposterior radiographs, medial/lateral cortical contact was defined as the sum of the medial and lateral cortical contact. For the 29 patients with available lateral radiographs, anterior/posterior cortical contact was defined as the sum of the anterior and posterior cortical contact, and complete cortical contact was defined as the sum of the anterior, posterior, medial, and lateral cortical contact. All measurements were scaled to 100% to accurately compare femoral stems of different lengths.
Data Analyses
Python was used for data analysis. Radiographic outcomes were compared to other radiographic measurements using Pearson’s correlation coefficient, and to the ideal mean, using the 1-sample t-test. McNemar’s chi-square, chi-square, and related-samples t-test were used to compare values within patients. The significance level was set at p<0.05.
Results
Mean estimated blood loss was 1039.4 milliliters (mL) (range 50-3100mL) and 4 patients required transfusion of packed red blood cells intraoperatively. There was 1 patient who sustained an intraoperative femur fracture and the patient recovered successfully without the need for revision. Mean length of stay was 4.6 days (range 2-21 days) and 16 (29.63%) patients were discharged directly home (Table 2).
Postoperative periprosthetic infection occurred in 4 patients and was the most common complication and the most common indication for further revision. 1 patient required further revision for evacuation of a postoperative hematoma. The patient then required an additional revision more than 90 days postoperatively for a periprosthetic infection. 1 patient sustained an ipsilateral tibial plateau fracture shortly after rTHA that was treated nonoperatively. This patient later required further revision for periprosthetic infection of their rTHA over 90 days postoperatively. 1 additional patient had a pulmonary embolism and multiple ischemic infarctions and 1 patient died of unknown etiology in the immediate postoperative period (Table 2). Patients who sustained a postoperative complication were significantly older (67.67 years vs 66.15 years, p<0.001), weighed more (36.02 vs 29.33 kg/m2, p<0.001), had higher blood loss (1350.0 vs 993.90 mL, p<0.001), and longer length of stay (6.67 vs 4.31 days, p<0.001). These complications were not related to the indication for surgery (p=0.08), gender (p=0.32), laterality (p=0.22), Paprosky classification (p=0.32), bone mineral density (p=0.55), whether an extended trochanteric osteotomy was performed (p=1.00), or discharge disposition (p=0.94). There were no revisions for aseptic loosening or failure of the diaphyseal engaging femoral stem.
Radiographic Analysis
Canal fill ratio was less than 100% (mean=85.85%, range=69.1-96.0%, p<0.001). Medial/lateral cortical contact was less than 100% (mean=73.33%, range=36.3-97.9%, p<0.001). Anterior/posterior cortical contact was less than 100% (mean=69.56%, range=30.8-90.4%, p<0.001). Complete cortical contact was less than 100% (mean=71.74%, range=42.2-88.1%, p<0.001). Subsidence was higher than 0.0 mm (mean=2.07mm, range=0.4-7.6mm, p<0.001).
Extended trochanteric osteotomies were associated with a lower canal fill ratio (p=0.04). Whether an extended trochanteric osteotomy was performed was not associated with subsidence (p=0.78), medial/lateral cortical contact (p=0.43), anterior/posterior cortical contact (p=0.41), or complete cortical contact (p=0.79).
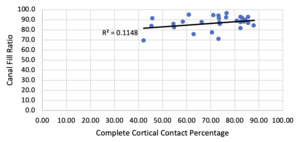
Canal fill ratio positively correlated with medial/lateral cortical contact (r=0.45, p=0.001, Figure 1), but not anterior/posterior cortical contact (r=0.17, p=0.37), complete cortical contact (r=0.34, p=0.07, Figure 2), or subsidence (r=0.08, p=0.58). Medial/lateral cortical contact positively correlated with anterior/posterior cortical contact (r=0.48, p=0.01, Figure 3). Complete cortical contact did not correlate with subsidence (r=0.13, p=0.50). Subsidence was not associated with medial/lateral cortical contact (r=0.17, p=0.23) and anterior/posterior cortical contact (r=0.02, p=0.93, Table 3).
Discussion
While multiple case reports have been published stating that this modular diaphyseal engaging stem was implanted during rTHA (Duensing, Stanley, and Bolognesi 2021; Saunders et al. 2020; Elsheikh and Gul 2019; Johnston et al. 2022; Merchant, Kelly, and Quinlan 2014), in which all patients had a successful recovery, few studies have reported outcomes of this revision femoral stem. Several studies do report outcomes of using several different stems within the same cohort, making it difficult to draw conclusions about any singe stem (Katakam et al. 2021; Parry et al. 2018; Wood et al. 2019).
Hancock et al. retrospectively reviewed 48 revision THAs using the same femoral stem as our study with mean 1 year follow-up (Hancock et al. 2018). Compared to our study, Hancock et al. found a higher incidence of postoperative periprosthetic infections (7.41% vs 10.42%), dislocations (0.0% vs 4.2%), revision for subsidence (0.0% vs 2.08%), and lower mean subsidence (2.07mm vs 1.1mm) (Hancock et al. 2018). Pawar et al. found a lower rate of reoperation for recurrent infection (3.51% vs 7.41%), but a higher rate of dislocation (5.26% vs 0.0%, Table 2) and higher subsidence (4.5 mm vs 2.07mm) (Pawar et al. 2022). We found no incidence of mechanical failure of this stem at mean 2-year follow-up, while Pawar et al. had 1 incidence of mechanical failure at 8 months postoperatively (Pawar et al. 2022). While our study identified that an extended trochanteric osteotomy was associated with a lower canal fill ratio (p=0.04), we similarly found on associated with between performing an extended trochanteric osteotomy and subsidence (p=0.78) (Pawar et al. 2022).
While canal fill ratio and cortical contact are established methods of radiographic analysis, our study demonstrated that these methods can be successfully converted to percentages, so that diaphyseal femoral stems of different lengths can be compared (D’Ambrosio et al. 2020; Moriarty et al. 2020). While the radiographic measurements were significantly less than 100% (p<0.001), we did not expect 100% canal fill ratio or cortical contact due to the tapered design of the femoral stem.
Previously published literature has demonstrated strong correlations between canal fill ratio and cortical contact with postoperative subsidence (D’Ambrosio et al. 2020; Moriarty et al. 2020). However, our study showed no correlation between canal fill ratio and subsidence (p=0.58), medial/lateral cortical contact and subsidence (p=0.23), anterior/posterior cortical contact and subsidence (p=0.93), or complete cortical contact and subsidence (p=0.50). In addition, our study showed lower rates of overall complications (11.11%), postoperative infection (7.41%), aseptic loosening (0.0%), and dislocation (0.0%) compared to previously published studies (Badarudeen et al. 2017b; Kenney et al. 2019). This is even in the setting of canal fill ratio (p<0.001), medial/lateral cortical contact (p<0.001), anterior/posterior cortical contact (p<0.001), and complete cortical contact (p<0.001) less than 100% (Table 3). Therefore, it is important for surgeons to be aware that this uncemented diaphyseal engaging femoral stem may be well fitting despite relatively low radiographic canal fill ratios and cortical contact percentages.
Limitations to this study include small sample size of 54 patients and no instances of aseptic loosening. While this prevents us from evaluating our radiographic methodology in assessing for aseptic loosening, it demonstrates the success of this uncemented diaphyseal engaging femoral stem in the setting of severe femoral bone loss and rTHA.
Conclusion
This uncemented diaphyseal engaging femoral stem had a low complication rate (11.11%) when used for revision THA. While canal fill ratio, medial/lateral cortical contact, anterior/posterior cortical contact, and complete cortical contact was less than the expected mean of 100%, all of these radiographic measurements were not correlated with subsidence. It is important for surgeons to know that this uncemented diaphyseal engaging femoral stem can be well fitting despite relatively low canal fill ratios and cortical contact.