Introduction
Orthopedic residency requires intense manual skills training across multiple disciplines and subspecialties. Currently, most hands-on learning sessions are available using cadaver labs and simulations. The limitations of these learning opportunities are high cost and only available to single session. Theoretical and practical expertise is needed when learning new concepts; repetition and hands-on experiences have been proven to improve competency (Sattar et al., n.d.). Simulated procedures using virtual reality (VR) allow for portable, collaborative and consistent training and evaluation to assess, correct, and improve the operative skills of orthopedic residents in a realistic and engaging learning environment. Studies have shown that VR simulators have demonstrated content, face, and construct validity; in other words, the software demonstrates the relevant steps to the procedure, realistically reflects what is seen in an operating room, and is able to distinguish different skill levels (Feeley, Feeley, et al., n.d.; Feeley, Turley, et al., n.d.). There have been studies that demonstrated improvement in technical skills and patient outcomes in short term follow up in cases for minimally invasive spinal surgery where VR, augmented reality (AR), and mixed reality (MR) surgical simulators have a role in training (Lohre, Wang, et al., n.d.). Immersive VR can be used to supplement and augment procedural training and reduces the time it takes for trainees to learn specific skills (Lohre, Bois, et al., n.d.). Immediate translation of surgical skill from immersive VR to the operating room shows the efficacy of skill transfer and patient safety in addition to cost-effectiveness (Lohre, Leveille, and Goel, n.d.).
Case Description
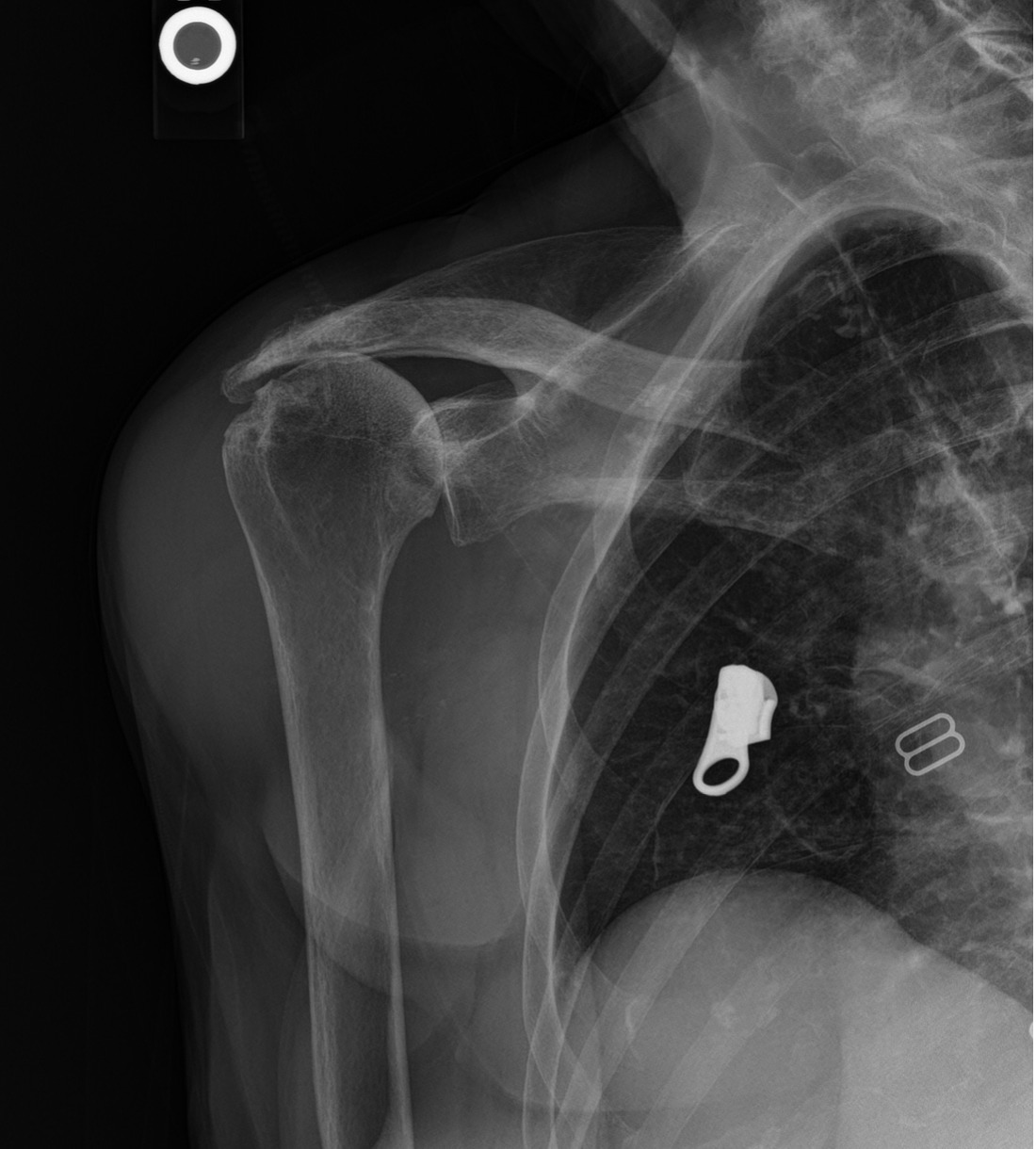
An 81 year old right hand dominant female with a history of rheumatoid arthritis presented with atraumatic end-stage right glenohumeral arthritis. She was noted on her initial visit to have clinical and radiographic findings consistent with severe rotator cuff arthropathy (fig. 1) with limited shoulder range of motion and restrictions in her functional scores and activities of daily living. After a discussion with the patient she initially elected to trial conservative management, however she only received partial transient relief at best. After failing many months of activity modifications, formal physical therapy, a subacromial bursal aspiration for a large symptomatic bursal cyst, and two subacromial injections, she finally elected to proceed with operative intervention in the form of a right reverse total shoulder arthroplasty.
The attending on this case was a board-certified, fellowship trained orthopedic surgeon and is a high-volume shoulder replacement surgeon, performing roughly 65-70 shoulder replacements per year. The resident working on the case was a third year orthopedic resident who was rotating through the hand and upper extremity service at the time. He had only assisted in 2-3 reverse total shoulder replacements prior to this surgery, and this was his first that required a glenoid augment, so his initial comfortability level with this case was fairly low.
Imaging
Pre-operative x-rays and CT of the right shoulder showed significant glenohumeral joint degenerative changes with Hamada grade 4B rotator cuff arthropathy, significantly high riding humeral head, and significant superior glenoid wear, as well as a chronic acromion fracture. (fig. 1&2)
Preoperative Plan
The patient’s imaging and clinical findings were thoroughly reviewed and discussed between the attending and resident a few days before the surgery was scheduled. With her rotator cuff arthropathy and wear pattern we elected to perform a reverse total shoulder arthroplasty through a standard deltopectoral approach using the with the addition of a superior glenoid augment. The operative plan was practiced and executed in the virtual reality setting by the resident and attending in the week leading up to the real surgery, which is discussed further below.
Operative Results
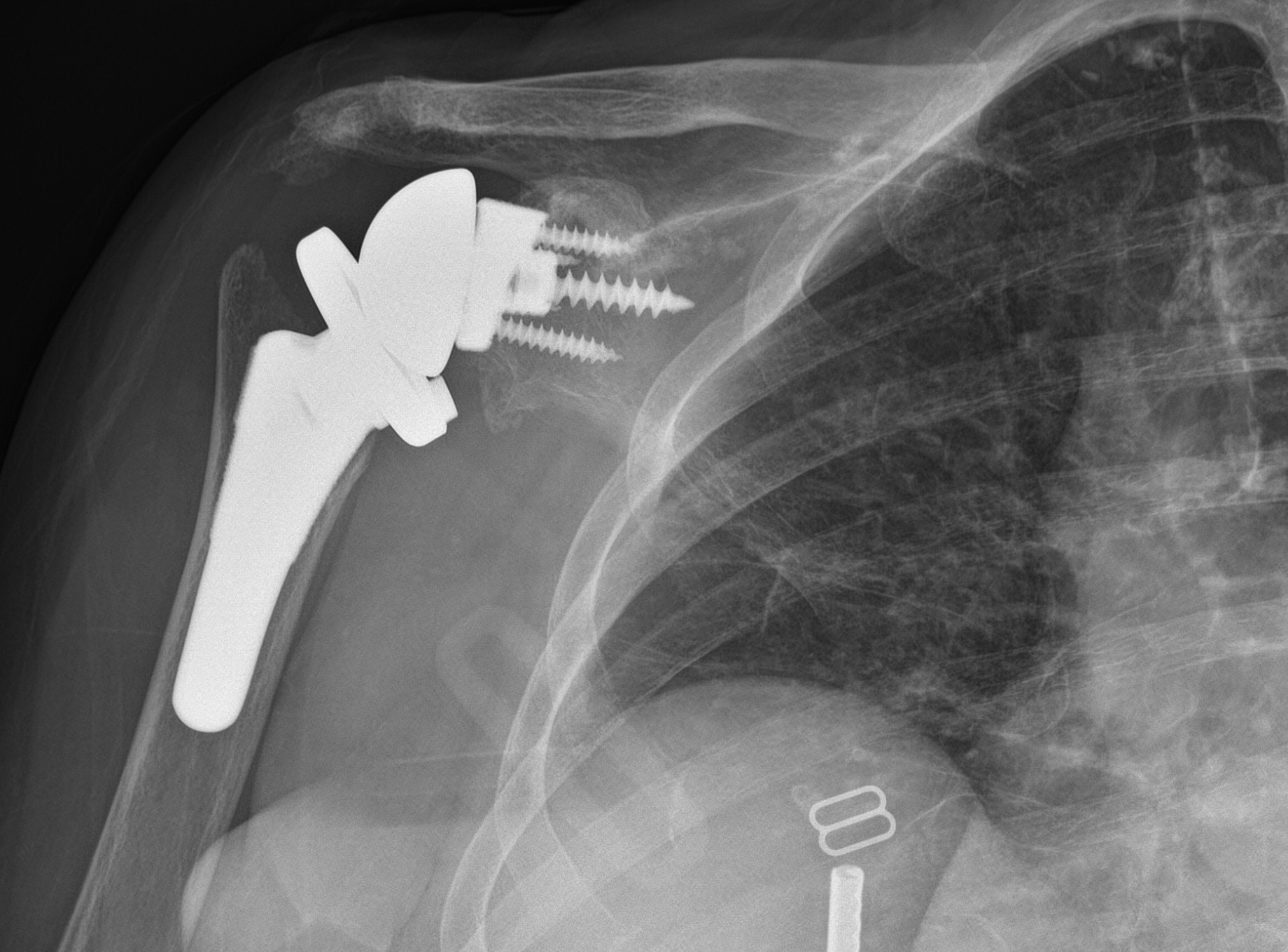
The patient’s post-operative course has been unremarkable. She is healing well with no clinical or radiographic evidence of hardware issues (fig. 3). She is now over 2 months out from her procedure and her reported pain, range of motion, and functional scores have all significantly improved. She has suffered no complications to this point.
Discussion
In the week leading up to the surgery, the resident and attending went through a trial run of the case using a virtual reality surgical software on an immersive virtual reality headset in which both were able to work in the same virtual space for coaching and teaching. They chose the reverse total shoulder module on the virtual reality software that corresponded to the implant system they were planning to use on the real patient, and even were able to choose a glenoid with similar wear patterns to most closely replicate the details of the actual surgery. The resident performed all steps of the operative case in this virtual reality setting under the guidance and coaching of the attending. Any mistakes or corrections could be made in real time by simply re-starting the necessary procedural step in the module and advancing to the next step once ready. After a couple of successful runs through procedure together, the resident took one headset home to continue practicing the procedural steps and techniques before assisting in the live surgery later that week. He then assisted with the live surgery, performing many of the same steps in this real space that he had in the virtual space.
The pre-operative virtual practice for the case was felt to be extremely valuable by both the attending and resident. From the resident’s perspective, he was able to initially run through the procedural steps in a slow, controlled, risk-free environment with the attending present and without the constraints of the patient’s time under anesthesia, operating room costs, staffing, etc. This allowed for coaching, teaching, and controlled failure and error correction without risking patient harm. As an example of this, on the first virtual attempt the glenoid guidewire was advanced far too anterior which could have been disastrous to a live patient. In this controlled setting, however, this mistake was able to be discussed and corrected without repercussions. The resident was then able to continue practicing the procedure on his own in the virtual setting over the following days leading up to the real case until he felt comfortable with the steps and techniques. Being able to make and correct mistakes, learning the procedural steps, and picking up helpful tips and tricks from the attending advanced the resident much further along the learning curve than would otherwise have been possible.
From the attending’s standpoint, this guided pre-surgical preparation allowed for a greater sense of trust and confidence in the resident during the actual case. Since they had already walked through the case together methodically, there was far more comfortability in allowing him to perform many of the steps of the case under his supervision. Additionally, the nuances of that specific attending’s techniques were able to be discussed and practiced ahead of time, which cut down significantly on the intra-operative discussion and guidance and allowed for smooth transition and increased efficiency in the live surgery.
The virtual reality software allowed for controlled teaching and guidance through a surgical procedure with opportunities for subsequent unlimited practice runs while still maintaining a level of realism that is otherwise hard to come by. There was clear immense benefit on many levels to both the attending and resident participating in the case in terms of shorter resident learning curve and greater attending confidence in the trainee, with added benefit to the patient and hospital through a more efficient operative experience with minimal added risk. As this technology continues to grow and case variety continues to expand, one can only imagine the continued benefits to surgical training.