Introduction
Patellar tendon rupture is an uncommon injury but has severe debilitating effects on patients (Friedman et al. 2020). It most commonly occurs in patients younger than 40 years of age, with men being more affected than women (Jagow et al., n.d.). Risk factors for rupture include but are not limited to chronic renal disease, diabetes mellitus, chronic corticosteroid use, overuse injuries including tendinopathy (Hsu and Siwiec 2022).
For acute ruptures, surgical repair is considered the standard of care (Gilmore et al. 2015; Lee, Stinner, and Mir 2013; Greis, Lahaw, and Holmstrom 2005; Kovacev et al. 2015). In contrast, chronic tears treatment is more complex. Treatment consists mainly of debridement of the ruptured tendon and the use of a bridging/supplementary graft for reconstruction (Bouguennec and Colombet 2018). However, there are no high-quality studies on this matter, with most of those being case reports and case series describing different techniques performed and different grafts used in each one. The grafts used are usually autografts or allografts of the Achilles, Semitendinosus, Gracilis, contralateral bone-patellar tendon-bone and artificial materials such as LARS ligament and Leeds-Keio prosthetic ligament (Bouguennec and Colombet 2018; Maffulli, Del Buono, and Oliva 2019; Talia and Tran 2016; Naim, Gougoulias, and Griffiths 2011).
In this article, we present a case of a patient who had a chronic recurrent patellar tendon tear that has failed surgery twice. The technique performed is a V-Y quadriceps-plasty along with a patellar tendon reconstruction using tibialis anterior allograft in a triangular fashion around the tibial tubercle or as we call a Delta repair of the patellar tendon (Figure 1). A dermal allograft was used to drape our construct providing a biological scaffold. This technique is not previously described as of the time of publication of this paper.
Case presentation
Patient is a 36-year-old male who had a history of bilateral patellar tendon rupture due to basketball related injuries. He presented with a recurrent right patellar tendon rupture that occurred weeks prior to presentation where he states that he fell on his right knee and heard a “pop”. Subsequently he had trouble ranging his knee and was forced to use a cane to ambulate. At the time of evaluation, he was ambulating with crutches, his pain was rated at a 10/10 scale and was described as a constant and sharp pain around the knee. Aggravating factors include movement and all activities of daily life. Alleviating factors included painkillers and elevating the leg. The pain radiated upwards along the lateral thigh. On physical exam, swelling was present. There was a previous midline scar over the anterior knee. There was a visible patella Alta and the extensor mechanism was clinically disrupted. Knee ROM was 0-90 passively with pain at his flexion limit. The patient was not able to lift his right leg up off the examination table, there was inability to extend his knee from a flexed position no active ROM whatsoever. Extensor hallucis longus (EHL), flexor hallucis longus (FHL), tibialis anterior, gastrocnemius were all intact. Sensation was intact and +2 distal pulses.
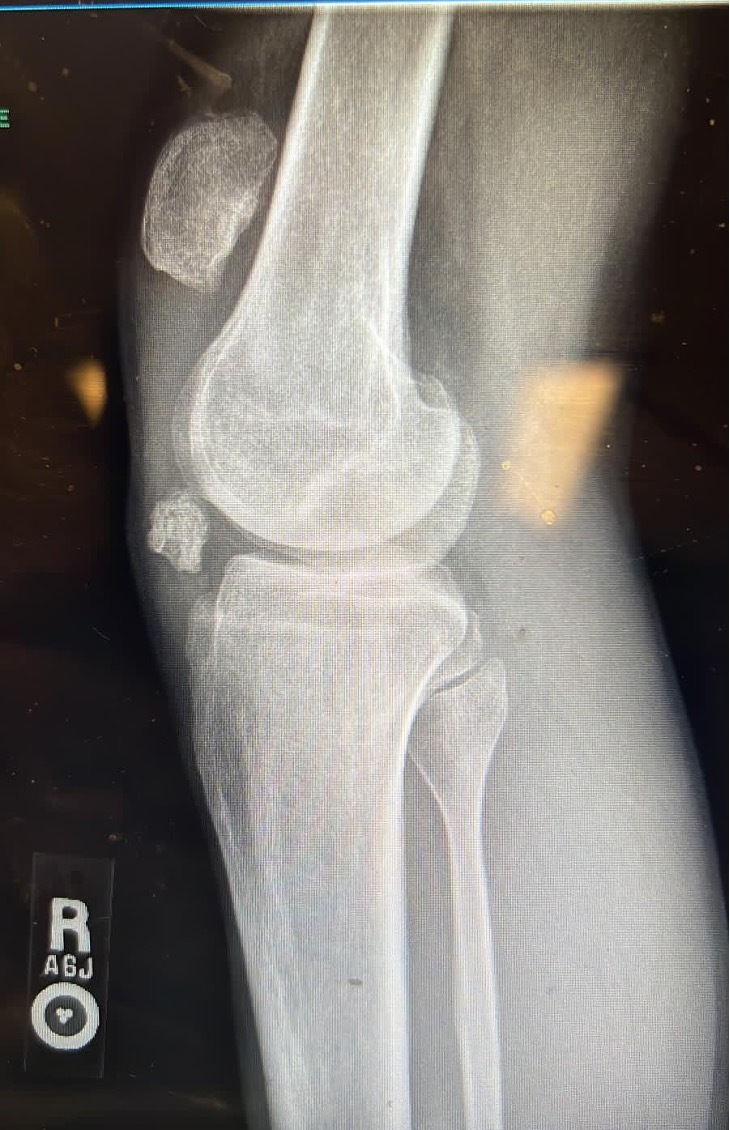
The above findings on physical exam were confirmed using X-ray and MRI scan (Figure 2) which showed a recurrent patellar tendon rupture with patella Alta and a distal pole patella fracture remnant. Risks of the surgery and anesthesia were explained to the patient who agreed with the plan and had all his questions answered.
Surgical technique
The patient was identified in the preop holding area. The right lower extremity was marked. He was then wheeled to the operating room whereby general endotracheal anesthesia was given in the supine position. All bony prominences were padded. A tourniquet was applied to the right lower extremity. Preoperative antibiotics were given. Time-out was done by staff. The tourniquet was inflated to 275 mmHg. The previous incision over the anterior knee was re-explored and extended mainly proximally. Both medial and lateral flaps were elevated. The previous distal patella sutures were removed. There was a small patellar tendon remnant distally, close to the tibial tuberosity. The avulsed distal patellar fragment was small and was excised. There was no possibility of primary repair without the use of an allograft due to the significant proximal migration of the patella. A quadriceps plasty was necessary. A V en Y quadriceps-plasty was performed and repaired using non absorbable sutures providing around 4 cm of distal migration of the patella. A tibialis anterior allograft was prepared and was whipstitched on both ends using non absorbable sutures. A 7 mm drill hole was made in the tibia slightly distal to the tibial tuberosity, the allograft tendon was passed in the hole and both ends were repaired to the patellar tendon remnant. Two 7mm interference screws were secured on each side of the tibia transverse tunnel to provide additional fixation of the tendon in the bone and to prevent any cutout. Krackow sutures were performed over the tibialis anterior tendon including the patellar tendon remnant and then both ends of the allograft converted to the distal patellar pole with a side to side repair done to centralize the repair ending in robust suture anchors fixation at the distal patellar pole and were secured using 4.75 SwiveLock (Arthrex, Naples, FL) anchors forming a delta or triangular configuration. An Arthroflex (Arthrex, Naples, FL) graft was draped and sutured on top of the tendon to provide more biological healing. Subsequently on each side of the patella a 4.5mm FT suture anchor (Arthrex, Naples, FL) was secured to reapproximate the medial and the lateral retinacula. An additional drill hole was made in the proximal patella in a transverse fashion and a fiber tape was passed and was secured in a Box and X configuration along with the sutures from the corkscrew anchors to the tibial tuberosity using 2 x 4.75 mm SwiveLock (Arthrex, Naples, FL) anchors in 30° of flexion as an added security construct to protect the Delta repair. Intra-op X-rays are shown in Figure 3. At this time extensive irrigation was done followed by release of the tourniquet and hemostasis. Closure was done using 1.0 Vicryl for the quadriceps followed by 2.0 Vicryl for the deep dermis and 3.0 nylon for the skin. Sterile dressing was applied followed by a knee immobilizer. The patient tolerated the procedure well. He was extubated successfully and wheeled to the recovery room in good condition.
Post op and rehabilitation
Patient had a non-eventful recovery after surgery. The knee was kept in an immobilizer and the patient was kept inhouse for pain control and was discharged the next day.
At 1 week post op, his incision was dry and clean however he had significant swelling and ecchymosis. The sutures were removed at 2 weeks post op and the swelling had subsided by then. Since the patient had 2 previously failed repairs, had patella alta and the combination of allograft tunnel and the V en Y quadriceps plasty caused reasonable tension on the repaired tendon, we opted to put the knee in a well-padded cast in extension for additional 2 weeks to protect it.
Decision was made to proceed with range of motion of the knee 0-30 degrees and progress 15° every 2 weeks. A range-of-motion brace was applied. The patient was asked to do quadriceps isometric exercises and to weight bear partially using crutches. At 10 weeks post op, knee ROM was 0-45° and repeat Xray showed stable patellar repair (Figure 4). Patient was fully weight bearing independently. He continued physical therapy for a total of 5 months. At 24 weeks, pain was rated as a 1/10 only and the patient was given clearance to resume work. Last follow up was at 32 weeks post op. The patient had completed physical therapy and was back to work. His pain improved and was rated as a 1-2/10 depending on the workload subjected to his knee. ROM was 0-75 of flexion.
Discussion
The treatment of chronic patellar tendon tear is still a challenge in the literature. The main surgical rationale is to debride the scarred and devitalized tissues and perform a graft reconstruction with or without quadriceps lengthening. Any delay in treatment leads to disability, patella alta, and further quadriceps shortening and knee stiffness (Greis, Lahaw, and Holmstrom 2005). As such, many techniques have been described in the literature and each carries its pros and cons. One study described the use of a gracilis and semitendinosus grafts to reconstruct a previously repaired tendon that has failed, with a good result following bracing and physiotherapy (Wagih 2014). Another study described a double row suture anchor fixation with Achilles allograft augmentation (Cregar et al. 2022). Another case series studies showed good to excellent outcomes after operative repair of chronic patellar tears using a direct repair approach with autogenous or allogenous graft augmentation and cerclage wire reinforcement (Jabalameli et al. 2018). In our case, the patient previously had bilateral patellar tendon repair, then the right tendon failed, was repaired again then failed for a third time before presenting to our clinic. Due to that, conventional autografts were already used, and we had to look for another source, adding to the complexity of the treatment algorithm. In the literature, tibialis anterior graft was rarely described. It is not as widely described as the gracilis or contralateral bone-patellar tendon-bone among others. We supplemented the allograft with another dermal cadaveric scaffold to strengthen the construct and optimize the healing. Another important aspect is the lengthening of the quadriceps we had to do. In effect, after a chronic tear, and due to the pull from the quadriceps tendon, the patella usually migrates proximally. Quadricepts-plasty is described in the literature and is mainly done to lengthen the quadriceps tendon to re approximate the patella to its anatomical position (Watson, Kingham, and Patel 2022). This is shown in the follow up imaging we did for our patient. Another described procedure to lengthen the quadriceps tendon is with the use of an external fixator (Kumar et al. 2020).
In this article, we described a new technique where the patient had a chronic tear as well as failed repair twice. We performed quadriceps-plasty in addition to the use of a tibialis anterior allograft in a triangular fashion through transverse tunnel in the tibia, the so-called Delta repair. We supplemented this repair with a dermal allograft as well to enhance the mechanical and biological properties of the construct. The patient had relatively a favorable outcome. He presented initially on crutches and was not able to independently walk. After the procedure, he was able to ambulate again, and he even resumed his previous occupation.