Introduction
Arthrogryposis Multiplex Congenita (AMC), also known as multiplex congenita contractures (MCC), is a rare, nonhereditary disease characterized by multiple joint contractures (Bamshad, Van Heest, and Pleasure 2009). The descriptive diagnosis denotes more than 300 individual diseases with varying etiologies, but share the common feature of congenital, non-progressive joint contractures involving at least two different areas of the body (Kowalczyk and Feluś 2016). Affecting 1 in 30,000 live births (Thompson and Bilenker 1985), it commonly presents with upper limb and knee deformities, scoliosis, muscle wasting, hip conditions including contractures, dislocations and subluxations (Yau et al. 2002).
There are only 7 case reports on total hip arthroplasty (THA) in patients with AMC, all of which report primary procedures (Dalton, Magill, and Mulhall 2015; Fisher and Fisher 2014; Cameron 1998; Leonard and Nicholson 2010). A recent case report described an emergency use of a distal femoral replacement for an acute periprosthetic fracture for a patient with AMC with multiple failed revision total knee arthroplasties (Emara et al. 2021). Technical difficulties in performing the operations were described due to the soft tissue obstacles and remarkable stiffness. Limited literature exists to guide surgeons on the treatment of patients with AMC. Thus, we present our results to adjoin among the body of existing publications, describing a revision THA (rTHA) using a direct anterior approach (DAA) for the management of a patient with AMC presenting with chronic right hip pain from a revised THA.
The patient was informed that data concerning the case would be submitted for publication, and he provided consent.
Case Report
Preoperative Course
A 48-year-old man with AMC presented with 1 year of chronic right groin pain and worsening functional disability. His past surgical history was significant for right posterior THA in 1988 at the age of 15, left posterior THA in 1989, right total knee arthroplasty (TKA) in 1991, left TKA in 1992, right revision TKA in 2013, lumbar laminectomy in 2014, and repair of a herniated nucleus pulposus in 2015. In addition, the patient underwent a right posterior rTHA in 2013 for advanced polyethylene wear. The 46-millimeter (mm) acetabular cup and femoral stem were both found to be well fixed and well positioned. The polyethylene liner and 28 mm +0 mm head were successfully exchanged. However, exposure was challenging via the posterior approach due to the patient’s contractures. The patient had no excessive intraoperative bleeding and suffered no complications in the immediate postoperative period after each of his surgeries. His past medical history was significant for rheumatoid arthritis, treated with enteracept, which was discontinued 4 weeks prior to surgery.
On examination, the patient had a body mass index of 18.55 kilograms/meter (Kowalczyk and Feluś 2016). The patient presented with severe right hip pain. The patient had 0 degrees (°) of internal rotation, 10° of external rotation, 10° of hip flexion, and 0° of hip extension. The patient had severe ankylosis and contractures of hips ankles, knees, hips, spine, shoulder, elbows, and wrists. The patient walked with a valgus thrust in the right knee, and an antalgic gait on the right side. The patient had generalized muscle weakness and was neurovascularly intact throughout.
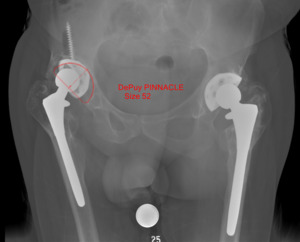
Radiographs revealed the presence of bilateral THA components, with catastrophic failure of his right acetabulum component with osteolysis and debonding of the bone implant interface (Fig. 1). Additionally, lucency of the proximal femur was noted, most likely secondary to osteolysis, and no evidence of subsidence of his femoral component was seen. Extensive heterotopic ossification (HO) of the capsule was evident on radiographs. The patient’s preoperative infection work-up was a Musculoskeletal Infection Society score of 0, including c-reactive protein and erythrocyte sedimentation rate within normal limits and negative gram stain (Parvizi et al. 2018).
After a long discussion of the risks, benefits, and expectations of the procedure, a rTHA with a DAA of his right hip was recommended and agreed upon in a shared decision between the patient and surgeon. Due to the significant difficulties with exposure during the patient’s previous rTHA in 2013 via a posterior approach and progression of the patient’s ankylosis, a DAA was determined to be the best approach. Since the patient’s severe ankylosis prevented inhibited the patient from passively internally rotating his right hip or bending his right knee, it was believed that a posterior approach would not provide sufficient exposure to revise the acetabular cup and retain the femoral stem.
Operative Course
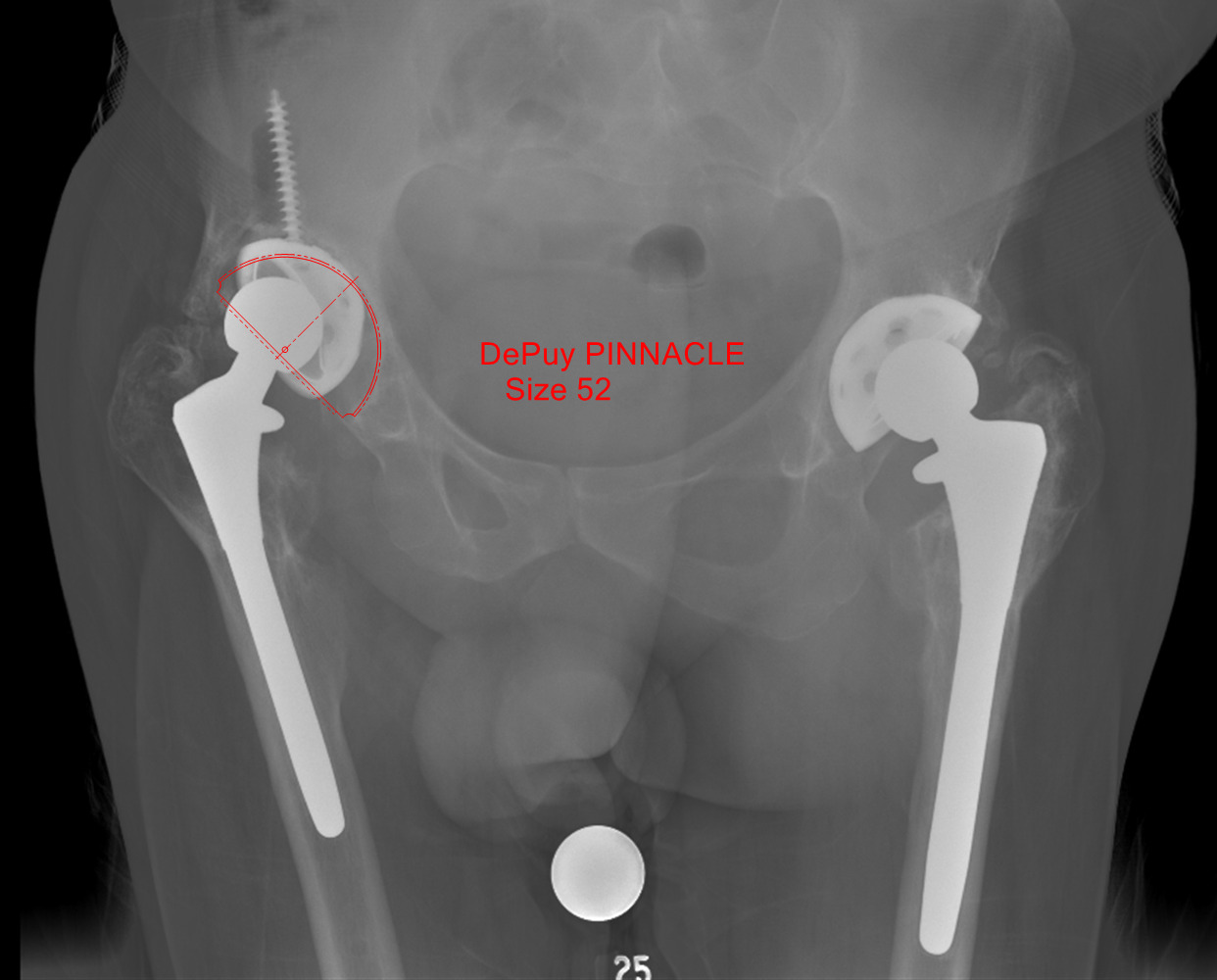
The preoperative radiograph was templated using a 52 mm Pinnacle cup (Depuy Synthes, Warsaw, IN) (Fig. 2). The patient was placed supine on the Hana table (Mizuho Osi, Union City, CA). Incision was performed from the anterior half of the iliac crest to the anterior superior iliac spine, and then extended an additional 10 centimeters towards the lateral patella. Dissection was performed down to the tensor fascia lata (TFL). The TFL was released from the anterior iliac crest, and superficial dissection continued using the TFL-sartorius interval. Rectus femoris was released from the anterior inferior iliac spine, and deep dissection was performed through the rectus femoris-gluteus medius interval. No purulence was encountered. Locating the femoral neck was difficult due to the extensive HO present. The leg was placed into extension and maximum external rotation. Capsulectomy and excision of the HO was performed down to the level of the femoral neck. The prosthesis was completely encased within heterotopic bone. The hip could not be distracted or dislocated, so additional debridement was performed around the joint to remove the HO.
Using traction from the Hana table, the hip was maximally externally rotated and subluxated laterally with a bone hook to remove the femoral head from the trunnion. The trunnion and stem were visually and manually inspected and found to be well-fixed without evidence of metalosis. Dissociation of the polyethylene from the acetabular shell was unsuccessfully attempted to gain access to one of the cancellous dome screws, which appeared to be well-fixed. However, the acetabular component was found to be loose, and the cancellous dome screw was broken. A rongeur was successfully used to remove the loose acetabular component. Dissection on the femur was carried down to the level of the septal perforators on the vastus lateralis. A retractor placed at the posterior aspect of the transverse acetabular ligament successfully retracted the femoral component posteriorly, allowing better access to the lose acetabular component.
The second broken cancellous dome screw was identified. The broken screw removal set could not be utilized due to the angle of the screw. Instead, an osteotome and vice grips were used to successfully remove the cancellous screw without significant bone loss. Gentle reaming proceeded up to the size 51 mm reamer. Autograft was utilized to reverse ream into the segmental and contained defect within the acetabulum. A 52 mm Pinnacle multi-hole with Gription acetabular cup (Depuy Synthes, Warsaw, IN) was impacted into 20 degrees of forward flexion and 40 degrees of abduction (Fig. 3). The acetabular cup had a primary impaction bite and was quite stable. The position of the acetabular cup was confirmed using intraoperative fluoroscopy and software that digitizes radiographs to determine positioning of the acetabular component. The acetabular cup was further secured with five 6.5mm cancellous dome screws. A 32mm head was chosen secondary to the constraints on the 10/12 femoral stem taper. A 32mm neutral AltrX polyethylene liner (Depuy Synthes, Warsaw, IN) was impacted into place. A 32mm +5mm offset PFC femoral head (Depuy Synthes, Warsaw, IN) was impacted onto the trunnion.
The hip was reduced with internal rotation. Bleeding was controlled using electrocautery, and Betadine irrigation was performed. The incision closed in layers with #1 polydioxanone suture (PDS), 0 PDS, and 2-0 PDS. The TFL was repaired in a figure-of-eight fashion with #1 PDS. The skin was closed using nylon sutures, and a negative suction pressure dressing was applied. The patient was successfully extubated and transferred to the PACU in stable condition.
Postoperative Course
Immediate postoperative radiographs demonstrated proper alignment and adequate fixation of the acetabular and femoral components. Pathology showed no acute inflammation or evidence of infection. The patient was allowed to weight-bear as tolerated. The patient worked extensively with physical therapy and occupational therapy to improve mobility. The patient progressed to ambulating with platform crutches, which he required since he was unable to grip traditional crutches due to hand deformities. The patient was discharge to an acute rehabilitation center on postoperative day 7.
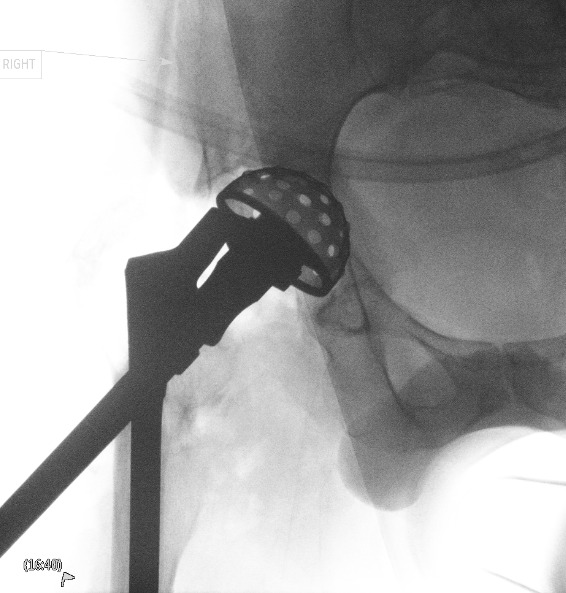
The patient was followed outpatient at 3 weeks, 3 months, 6 months, and one year after right rTHA. The patient had a successful recovery without complications. Radiographs performed 3 weeks postoperatively demonstrated a well-fixed, well-positioned revision acetabular component (Fig. 4). At one year postoperatively, the patient’s incision was well-healed, demonstrating a hypertrophic scar without erythema, effusion, or tenderness (Fig. 5). The patient reported that he no longer had pain in his right hip and had improved mobility due to the lack of pain. The patient ambulated with one crutch on his left side due to progression of his AMC and rheumatoid arthritis (Fig. 6). Radiographs performed one year postoperatively continued to demonstrate a well-fixed, well-positioned revision acetabular component without deformity or loosening (Fig. 7).
Discussion
The hips of patients with AMC are affected in 30-80 percent of cases (Dalton, Magill, and Mulhall 2015). Because of this high incidence, it is likely that patients with AMC will demand a higher burden of primary and revision arthroplasties to treat the affected joints.
We identified 7 case reports regarding THA in patients with AMC. Fisher and Fisher reported a successful primary right THA and left acetabular cup revision due to aseptic loosening in a patient with AMC (Fisher and Fisher 2014). Although similar to our patient, there is no known etiology that predisposes patients with AMC to aseptic loosening. Dalton, Magill, and Mulhall reported successful primary staged bilateral THAs via a posterior approach (Dalton, Magill, and Mulhall 2015). Leonard and Nicholson reported a successful primary THA using an antero-lateral approach in a patient with AMC and ipsilateral above the knee amputation (Leonard and Nicholson 2010). Cameron reported bilateral THAs via an anterolateral approach which was initially successful, but then patient developed progressive loss of range of motion in his hips (Cameron 1998). Theil et al. reported a series of 2 patients who underwent unilateral and 1 patient who underwent staged bilateral primary THA via a lateral approach (Theil et al. 2020).
Multiple studies have reported that DAA for can be successfully used for rTHA. A systematic review by Singh et al. reported on 319 rTHAs performed via the DAA across 9 studies, with 158 hips undergoing rTHA for aseptic loosening of the acetabular cup (Singh, Khurana, and Gupta 2021). They found that across the studies, most patients had a good or excellent outcome after rTHA and the overall complication rate was 1.6% (Singh, Khurana, and Gupta 2021). Kurkis et al. reported on 99 successful DAA rTHAs and showed that the DAA rTHA was associated with a lower risk of dislocations, but a higher risk of superficial wound complications (Kurkis et al. 2021).
We report the first instance of a successful case of THA and rTHA to be performed using a DAA in patient with AMC. It is important for surgeons to know that this may be an appropriate approach for patients with severe ankylosis and contractures that limit the ability to internally rotate the hip and flex the knee, since this is necessary for sufficient exposure during a posterior approach. Previously published studies have shown that an extensile DAA can be used for visualization of both the anterior and posterior columns of the acetabulum (Mast and Laude 2011; Manrique et al. 2014). Therefore, we believed that this surgery could be performed successfully from the DAA even if the patient would have required augmentation and/or buttressing of the acetabular component. Additionally, native hip dislocations occur in approximately 30 precent of patients with AMC and it is important to minimize this risk in patients with AMC who undergo THA (Bradish 2015).
DAA is an appropriate approach for patients with AMC undergoing THA or rTHA and may be especially helpful for exposure in patient with limited internal rotation and knee flexion.


_and_unilateral_lateral_(fig._1b)_radiographs_showing_fa.png)

_and_unilateral_lateral_(fig._4b)_.png)


__lateral_(fig._7b)__and_mechanical_axis_ful.png)

_and_unilateral_lateral_(fig._1b)_radiographs_showing_fa.png)
_and_unilateral_lateral_(fig._4b)_.png)


__lateral_(fig._7b)__and_mechanical_axis_ful.png)
