Introduction
Over the past 20 years, our understanding of functional mechanics related to total hip replacement component orientation has evolved from static evaluation on a supine AP coronal plane radiograph to a multiplanar assessment of the spine, pelvis, and femur in multiple positions (Gorin et al. 2004; DiGioia et al. 2006; Philippot et al. 2009; Kanawade, Dorr, and Wan 2014). Initially, Lazennec defined the coordinated movements of these segments of the postural chain in relationship to functional cup orientation (Gorin et al. 2004; Lazennec et al. 2007; Lazennec, Brusson, and Rousseau 2011). The result was an understanding of dynamic pelvic tilt, a mobile pelvis changing acetabular inclination and anteversion over a functional excursion determined individually. In simplest terms, the spinopelvic relationship means surgeons can no longer consider the hip joint in isolation as postural movement is always coordinated and not simply a mobile femur with a relatively immobile acetabulum used for volitional activities. The primary function of the hip joint is the involuntary positioning of the upper body mass that minimizes muscular efforts to balance the body in any assumed posture, a complex kinetic chain of joint interactions beginning with the head and continuing all the way to the ankle and foot (Lazennec, Brusson, and Rousseau 2011). A system driven by gravity, neurologic and muscular control, and flexibilities within the skeletal system. The clinical effects of varying pelvic spatial position during postural change on the orientation of hip joint replacement components was the focus of this research group led by the late Lawrence Dorr. Our purpose is to summarize the understanding achieved through this research, explain the classification system and how it differs from others, and how this knowledge may be applied to planning for a functionally safe total hip replacement.
Background
Surgeon selected coronal plane cup inclination and anteversion defines the paradigm hip surgeons have used for evaluation and planning for THA. However, these angles have been repeatedly shown to be unreliable for predicting safety from dislocation, a worst-case event that can be multifactorial (Abdel et al. 2016; Esposito et al. 2015). Impingement, whether bony, component, or mixed, is a better metric but has been clinically unmeasurable. Research on sagittal cup orientation has sought to determine if this plane may be more reliable in identifying outliers and component positions at risk of impingement and instability. The sagittal plane is the primary plane of motion of the body, the spatial position of the pelvis (including the acetabulum) and femur with their functional excursion can be directly measured pre and postoperatively and correlated with the coronal cup positions achieved at surgery. This data may be analyzed for safer implant positioning on an individualized basis. The approaches in the literature make use of two methods, identification of outlier mechanics in extreme positions to avoid risk (i.e., find where the cup shouldn’t go) (Pierrepont et al. 2017; Grammatopoulos et al. 2018) or measure values in essential positions testing pelvic and femoral dynamics to match the cup orientation to the patient (i.e., find where the cup should go) (Stefl et al. 2017). The classification described in this paper is based on the latter, using pre and postoperative multiplanar corroborative measurements and mathematical modeling of the effects of spatial tilt and mobility to achieve actionable findings and recommendations. Finally, this system accounts for the both sides of the hip joint by incorporating femoral version within combined anteversion guidelines as well as femoral mobility into a combined functional safe zone measure, the Combined Sagittal Index, (CSI) (Heckmann et al. 2018).
The Spinopelvic-femoral complex (Figure 1,2 Table 1)
The point of departure from established preoperative evaluation begins studying a lateral view of the spinopelvic unit and its functional anatomy using standing and seated lateral x-rays as previously described (Kanawade, Dorr, and Wan 2014). This is initially defined for any individual by measuring the pelvic incidence angle, PI, the fixed master postural parameter describing both the morphologic and functional characteristics of the pelvis (Legaye et al. 1998) (Figure 1). Morphology relates to the depth of the pelvis, the offset between hip center and load bearing center of the spine on the S1 sacral endplate. PI is also the primary postural functional descriptor as it is strongly correlated with all major positional parameters of the body. PI functional control is both structural and gravitational through the two pelvic parameters that comprise its value algebraically, PI=Sacral Slope (SS) + Pelvic Tilt (PT). Structural control is achieved through correlation with SS (r=0.73), which determines the curvature profile of the spine including the lumbar lordosis (LL), SS has an extremely strong correlation to LL (r=0.87) (Le Huec and Hasegawa 2016). The second pelvic parameter comprising PI is Pelvic Tilt, PT (r=0.64), the prime gravitational control parameter between truncal inclination above the pelvis and the lower extremity position below including the combined measure of hip joint position, the Pelvic Femoral Angle, PFA (Le Huec and Hasegawa 2016). The PT angle, driven by involuntary pelvic rotational positioning, achieves postural balance through an exquisite coordination between the suprapelvic inclination parameter, T1 Pelvic Angle, TPA (r=0.96) and the hip PFA (r=0.92). Pelvic function may be conceived mechanically as that of an intercalary gear between the spinal gear segment connected through the lumbosacral junction and the lower extremity gear connected through the femur at the hip joint (Heckmann et al. 2018). As teeth determine a gear’s function, degrees of angular change are the pelvic currency determining function in the normal state and influencing the patterns of deterioration later in life as arthritic change develops.
PI remains constant in adulthood through the integrity of the sacroiliac joints and supporting ligaments, it ranges from approximately 25-85° with a mean of 53°. As PI increases so do SS and PT, such that for every 10° increase in PI there is a SS 6-7° increase in SS and 3-4° increase in PT (Barrey et al. 2013; Vialle et al. 2005). For example, a PI of 53° may have a standing SS of 40° and PT of 13°, while a PI of 30° may have a corresponding SS and PT of 27° and 3° respectively, and a PI of 75° a corresponding SS and PT of 54° and 21° respectively, thus as PI increases the sacral endplate tilts vertically and the offset between hip and spine increases. A high PI pelvis is associated with extension of the hip (high PFA), flexibility of the spine (high LL) and a pelvis able to accommodate degenerative changes in upright posture by shifting the hip/spine positions between extension and flexion, accomplished through posterior pelvic rotation that decreases SS and reciprocally increases PT (Lazennec, Brusson, and Rousseau 2013). A low PI pelvis creates a stiffer, vertically oriented construct with the spine resting over the hips, relatively inflexible in standing, hips relatively flexed (low PFA), the lumbar spine less absolutely lordotic but actually more lordotic in relationship to the PI (more negative PI-LL), a strategy that brings the anterior pelvic plane, APP, into alignment with the body’s coronal plane (Barrey et al. 2013). The PI angle determines the environment and may be used to understand the level of decompensation a hip replacement must function within, it does not determine cup position. Functional cup position depends upon pelvic spatial position, pelvic mobility between positions, the required mating between the two components, and bony morphology of the acetabulum and trochanteric regions of the femur (Kanawade, Dorr, and Wan 2014; Stefl et al. 2017; Ike et al. 2020).
In the planning sequence, once the PI and SS spatial position are known in the standing position, the SS is measured in another position that determines the body’s response to the postural change, this change or delta defines a mobility measure that is compared to known values and may be categorized as a normal or outlier value. Changes between the supine, standing, and various sitting positions have been reported in the literature (Pierrepont et al. 2017; Grammatopoulos et al. 2018; Stefl et al. 2017; Ranawat et al. 2016; Esposito et al. 2016; Tamura et al. 2017; Berliner et al. 2018), the positions for this classification include standing where the hip is extended and the pelvis anteriorly rotated, and upright sitting where the hip is flexed and the pelvis rotated posteriorly (Figure 1). 20° or more of pelvic rotation between standing and sitting is normally measured in patients presenting for THA, 4-5X more than the normal change from supine to standing, it is the sitting position that is least addressed in contemporary coronal planning. The Dorr analysis employs intrinsic pelvic parameter (SS and PT) values shared with the spinal literature describing upright postural mechanics and utilized in Lazennec’s descriptions (Lazennec et al. 2007; Lazennec, Brusson, and Rousseau 2011) over the extrinsic APP used commonly in hip planning.
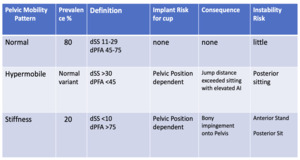
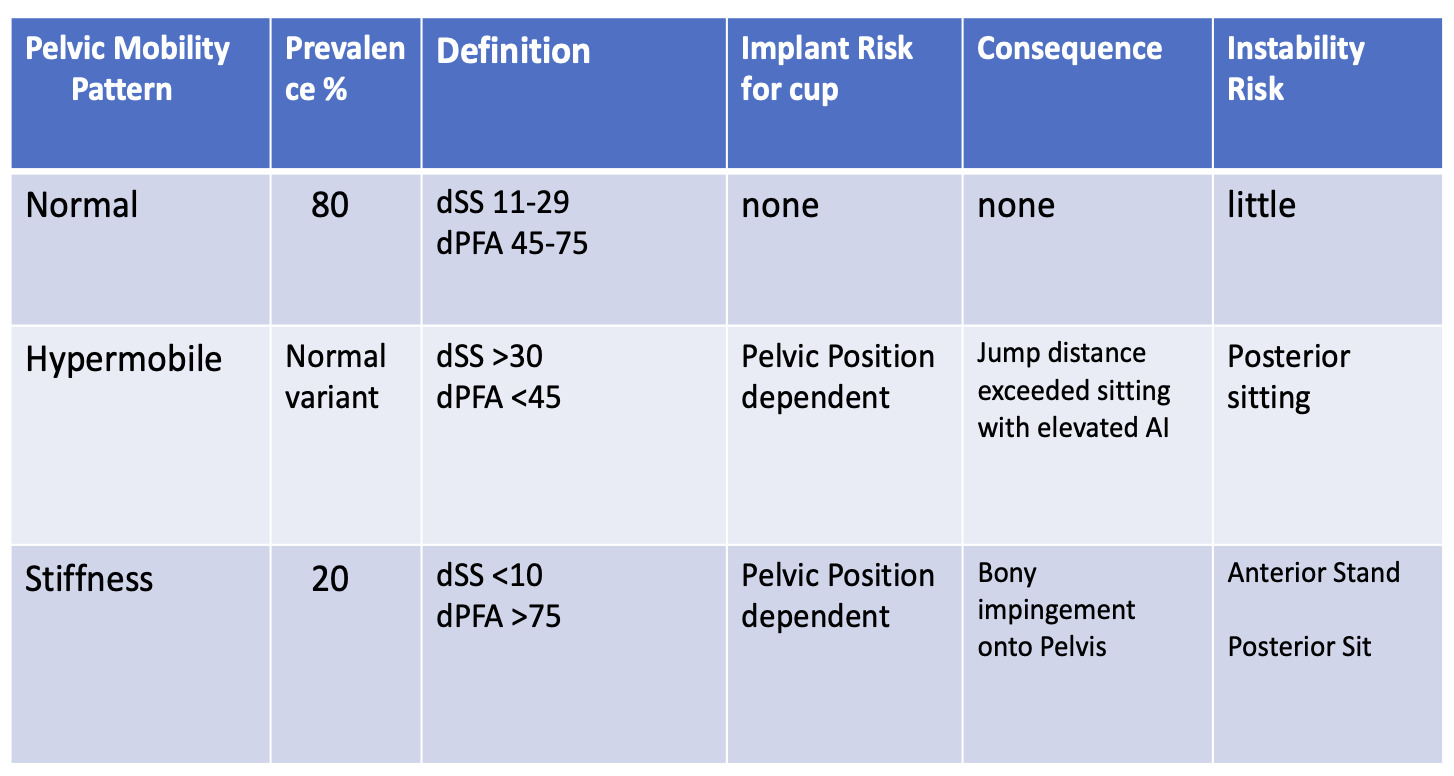
The Classification of Spinopelvic Imbalances (Tables 3,4)
The Dorr classification includes two pelvic positional imbalances with and without limited pelvic mobility (stiffness). A fifth outlier is a sitting position with a SS<10° which is called kyphotic sitting, this was felt to be pathologic if ≤5°.
Positional imbalances are determined on the basis of absolute values of the SS in the standing and sitting positions (Table 3). The clinical data revealed a normal distribution where neutral points existed at 30° with normal SS standing above and sitting below this level (Stefl et al. 2017). A pelvis that doesn’t achieve sitting SS less than 30° was called stuck standing (forward rotation), this maintains spine and hip extension through inability to rotate the pelvis posteriorly. A pelvis that doesn’t achieve standing SS greater than 30° was called stuck sitting (backward rotation), the hip and spine remain flexed even when upright extension is required. Confusion can arise by the term “stuck” implying stiffness but the stuck groups are purely positional outliers (similar to the use of PI-LL for standing positional imbalance) and may have normal mobility between the standing and sitting positions, e.g., a patient with standing/sitting SS values of 51/35 is classified as stuck standing while a patient with values of 28/13 is classified at stuck sitting, neither has stiff pelvic mobility.
Mobility between the standing and sitting position is a continuum that is clinically divided into normal between 10°-30° and stiff below 10° as here an increased risk exists, the coronal cup anteversion changes ≤7.5° between positions, half or less of the normal 15°-22° clinically measured in THA candidates (Tezuka et al. 2019) (Table 4). Hypermobility above 30° is determined to be a normal variant unless the pelvis stands with a low SS, this situation creates a grossly abnormal sitting position of extreme flexion of the lumbar spine and posterior pelvic rotation that is classified as hypermobile kyphotic, with sitting SS values often below 0°, the norm being above 10°. Kyphotic sitting with SS≤5°, no matter the mobility, was separately classified and found to be rarely reversible though the risk in this group varies significantly with the pelvic mobility. It is the stiff kyphotic, combining both significant outlier values for spatial pelvic position and mobility, that has the highest mechanical risk for safe cup placement (Ike et al. 2020; Tezuka et al. 2019), this group bears similarity to the HSS Simplified Hip-spine system’s II-B category.
Prevalence (Table 3)
In a cohort of 200 hips in 187 patients, low PI ≤41° occurred 9%, high PI ≥65° was 18%, 73% were normal. 41% had spinopelvic imbalances, 56% (23% overall) of these had both positional imbalance as either stuck standing or sitting and mobility imbalance of delta stand to sit SS (dSS) of <10°, these outliers are not mutually exclusive to each other (Ike et al. 2020). 14% were stuck sitting, 13% stuck standing, 10.5% kyphotic, and 20.5% were stiff. Low PI had a 43% chance of being stiff, 40% of being stuck sitting, 33% chance of stuck sitting and stiff, 56% of stuck sitting and kyphotic, and overall had a 44% chance of both positional and mobility imbalance. High PI had a 19% chance of stiffness, 25% of stuck standing, 14% chance stuck standing and stiff, with a 19% chance of both positional and mobility imbalances. In the full cohort of 320 hips in 291 patients, 37% had at least one spinopelvic imbalance with 18.75% chance of being stuck posterior (sitting), 8.4% stuck posterior and stiff, 9% chance stuck anterior (standing), 3.75% stuck anterior and stiff, and 11% chance of being kyphotic (Heckmann et al. 2021).
Acetabular parameters (Figures 1, 2, Table 2)
The primary parameter of sagittal planning is the position the cup, termed anteinclination (AI) (Kanawade, Dorr, and Wan 2014). As part of the pelvis, an acetabular implant moves in concert (1:1) with it into any assumed position, therefore delta AI= delta SS= delta PT. AI is measured by a line along the face of the cup to a horizontal reference in similar fashion to the way coronal inclination is measured on AP x-rays. Clinical range was documented as standing 35°+/-8, sitting 55°+/-10, providing cup positions for a mobility excursion from 2°-38°, no matter the tilt of the pelvis (Tezuka et al. 2019). The Sacroacetabular Angle, SAA (Figure 1), described by Lazennec (Gorin et al. 2004), whose vertex is formed by the intersection of the SS line along the S1 sacral endplate and the AI line extended anteriorly across the mouth of the cup, is the algebraic sum of the SS+AI. This is a constant value created on cup impaction that defines the cup’s relationship to the SS sacral slope of the pelvis. The Pelvic Acetabular Angle, PAA (Figure 1), formed by the intersection of the same AI line and the line connecting the center points of the hip and sacral plateau simultaneously describes the constant relationship between the cup and the PT pelvic tilt value (Heckmann et al. 2021). Geometrically, SAA+PAA=90+PI, integrating the cup AI position within the spinopelvic unit as determined by the individual’s PI and state of standing balance and seated mobility. SAA, PAA, and the complimentary angle to PI, (90-PI), therefore form the corner angles of a triangular structure depicting the functional relationship of the cup AI angle to both the SS/PT values as well as the dSS mobility. The cup AI angle is adjacent and below the triangle as measured to its horizontal reference line. (Figures 1 and 2).
Combined anteversion (Table 4)
Impingement occurs from mechanical collision between both sides of the hip construct; an accepted mechanism for measurable THA dislocations (Malik, Maheshwari, and Dorr 2007). Occurring between the stem neck and edge of the cup, bone against bone with trochanter to ilium or ischium, or bone against metal, the collision causes a levering moment at the impingement site that is resisted by a countering moment at the dislocating egress site (Brown et al. 2014). Component to component impingement is primarily caused by imperfect surgical combined anteversion, and bone to bone by the combination of distorted mobility between each of the two components (spinopelvic effect), often combined with a reduced offset and leg length (Heckmann et al. 2018; Malik, Maheshwari, and Dorr 2007; Palit et al. 2020). A proper combined anteversion accommodates the functionally changing pelvic tilt and femoral motions through different postures alleviating the dislocating moments, the femoral head remains centered with in the cup. With non-cemented femoral stems, adjustments for combined anteversion are made on the acetabular side, and this classification system recommends combined anteversion positions using the supine coronal plane radiographic ellipse for the cup anteversion with the femoral version estimated from the transepicondylar knee axis at the time of surgery (Stefl et al. 2017). Multiple studies, both clinical and laboratory, have defined the range of combined anteversion between 25-50° with men typically 5-10° lower than women (Ranawat et al. 2016; Dorr et al. 2009; Ranawac and Maynard 1991; Widmer and Zurfluh 2004; Yoshimine 2006; Hisatome and Doi 2011).
Functional Safe Zone, CSI (Table 4)
The Combined Sagittal Index, introduced by Heckmann et al (Heckmann et al. 2018) as the sum of (AI+PFA), is simply is a measure of the combined sagittal mobilities of the cup and femoral components between the standing and seated positions. Just as combined anteversion measures spatial orientation on both sides of the joint, CSI measures the combined excursion, together accounting for the mechanical behavior of the construct. CSI was found to be predictive of late dislocations, too low sitting for posterior and too high standing for anterior. A key finding was the compensatory increase in hip motion correlated to the loss of spinopelvic mobility, the femur making up in a nearly 1:1 fashion for the age-related degenerative pelvic stiffness. Recently, CSI was also validated as predictive in acute dislocations, making it the single best parameter to date for THA safe zone planning (Grammatopoulos et al. 2021).
PFA femoral hypermobility, in either position, was found to be the best preoperative predictor for cups implanted within the Lewinnek zone falling outside the CSI (Tezuka et al. 2019). PFA, a non-modifiable parameter and not the surgical cup AI becomes primarily implicated for functional outliers, a supportive reason for the failure of the Lewinnek zone principle. PFA is directly affected by the PT value which natively reflects the PI, higher PI associated with higher PT values, therefore CSI was stratified by PI into 10° stepped ranges for both standing and sitting positions (Ike et al. 2020). Low PI ≤ 41° was associated with a 28% chance of sitting CSI outlier status versus 6% with normal PI and 5% with high PI ≥ 65° (Ike et al. 2020), these hips sit in a hyperflexed position (PI derived spinopelvic imbalance) which increases anterior impingement risk, bony with pelvic stiffness and mixed with component impingement when the cup is placed with inadequate anteversion. In this series, low PI was associated with a 39% chance of CSI outlier status versus 9% for normal PI and 11% for high PI. Once again, It is rotational stiffness of the pelvis associated with a reciprocal compensatory femoral hypermobility that is the major cause of spinopelvic derived impingements, not the coronal cup positions. 76% of CSI outliers demonstrate this combined mobility defect, a major contribution to the understanding of THA biomechanics.
Recommendations (Figures 3,4)
Unique among classification systems, recommendations include both femoral and acetabular positions within combined anteversion and acetabular coronal orientations. Acetabular position is stratified according to pelvic mobility, with the normal dSS 11-29° between positions, the cup is placed within a 10x10° area, 35-45° inclination, 15-25° anteversion, combined anteversion within the full 25-45° range. Stiff hips with ≤10° dSS mobility, no matter the pelvic tilt, require cup positions within a 5x5° area of 45-50° inclination, 20-25° anteversion with combined anteversion 35-45°. Low PI, with a lower PFA<120° sitting, also requires this higher cup position. The hypermobile kyphotic sitter has risk of a high sitting AI therefore requires lower cup positions within another 5x5° area, 35-40° inclination, 15-20° anteversion, and lower combined anteversion 25-35°, though most patients correct significantly when postoperative hip flexion is restored. The neurological hypermobile hip or extreme athlete without a positional outlier (a hypermobile yoga practitioner with full hip ROM) requires cup values that may have the lowest radiographic anteversion directly correlated with mobility, 35-40° inclination, anteversion 10-20°, combined anteversion 25-35°. These cup positions may be adjusted based on broached femoral version, femurs <10° should have the cup version raised, while version >20° should have the version lowered, always respecting the version confines of the native acetabulum. In the sagittal plane (Figure 4), the linear relationships of tilt and mobility to AI cup position and the Dorr groups are seen. Tilt change causes a cup to increase its AI 2.5 degrees for every 10° decrease in standing SS while each 10° decrease in dSS will increase standing AI 5° and decrease the sitting AI 5°. Every Dorr grouping is associated with distinct standing and sitting AI positions.
Discussion
The Dorr classification recommendations were devised to be consistent with the available accuracy and precision range of most hip surgeons, no target requires under a 5° accuracy (Stefl et al. 2017). Preoperative planning requires the customary coronal mechanical reconstructive parameters; center of rotation, offset, leg length, and cup coverage with the addition of lateral standing and sitting spinopelvic radiographs as previously described (Ranawat et al. 2016; Esposito et al. 2016; Tamura et al. 2017; Berliner et al. 2018). PI and SS are measured in the standing and sitting postures alerting of three risk factors; (1) low PI inferior mechanics, (2) abnormal pelvic spatial position both in sitting (stuck standing and kyphotic sitting) and standing (stuck sitting), and (3) pelvic mobility, the prime determinant for sagittal AI cup position (Tezuka et al. 2019). Coronal cup recommendations (Figure 2) can be planned with or without the adjustment for femoral version if known or determined surgically. The addition of PFA standing and sitting confirms additional risk inherent to spinopelvic influences on the femur, standing values >190° (typically associated with PT>20°), sitting values <120°, and dPFA >75° are associated with hip hyperextension standing, hyperflexion sitting, and functional hypermobility respectively. Indications for dual mobility cups were spinopelvic stiffness, femoral hypermobility particularly with low PI and the stuck sitting kyphotic (the extreme imbalanced, stiff groups in Phan [Phan, Bederman, and Schwarzkopf 2015] and Vigdorchik [(Vigdorchik et al. 2021)]) being the absolute highest risk for bony impingement and dislocation. Similarly, patients over 75 years with pelvic stiffness, particularly smaller females with high standing and low sitting PFA, abductor weakness from trauma or neuromuscular disease, and poor tissue integrity at the egress site, as is often encountered in revision surgery are considered candidates along with the protection against bony impingement afforded by increased hip offset (Heckmann et al. 2018; Ike et al. 2020). Finally, a mismatch between native or accessible acetabular version and component orientation demands such as a retroverted acetabulum in a stiff patient that cannot support a cup version >15° is a valid indication. The simple presence of short segment hardware in the lumbar spine should not be considered an indication.
The limitation of this system includes the direct correlation of standing sagittal data to coronal supine positions as the supine to stand change varies significantly on an individual basis. The CSI value was only measured postoperatively and planning was never performed targeting a specific AI or making adjustments for abnormal PFA values, it only followed the supine coronal guidelines. Cup adjustments for native acetabular or broached femoral version outliers were not quantified, only the range of combined version was stated. These changes were made intraoperatively and could affect the recommendations. The algorithm is geared to match the cup optimally to the preop data in standing and sitting, it does not take into consideration changes that occur over time when hip function is restored. Approximately 10% of cases were felt to change groupings at one year follow up with the trend in most groups to decrease pelvic motion as femur excursion was restored. Nor does it measure hip position in extreme postures such as the flexed seated position, a proxy for posterior instability, thus it is not as sensitive a testing for lumbar flexion stiffness and pelvic excursion in the anterior direction.
The beauty lies in its intended user, the orthopedic practitioner not married to specific technologic products; it requires no advanced imaging, does not need the hip surgeon to measure any spinal values, provides guidance for both sides of the joint, providing guidelines to validated safe functional positions. His genius opened the “Dorrway” through which all quantitative biplanar planning algorithms will follow.




_and_sitting_(right)_schematic_diagrams_of_the_spinopelvic-femoral_complex_.png)
_and_sitting_(right)_lateral_spinopelvic_postoperative_x-rays_demonstrate_t.jpg)
_determined_by_absolute_ss_val.png)

_to_mobility_(dss)_to.png)




_and_sitting_(right)_schematic_diagrams_of_the_spinopelvic-femoral_complex_.png)
_and_sitting_(right)_lateral_spinopelvic_postoperative_x-rays_demonstrate_t.jpg)
_determined_by_absolute_ss_val.png)

_to_mobility_(dss)_to.png)
