Introduction
The cost of healthcare continues to rise, yet the value of healthcare services does not appear to be improving (Kaplan and Porter 2011; Shrank, Rogstad, and Parekh 2019). Value-based care looks to improve efficiencies and reduce waste and minimize costs while maintaining quality (Chatfield et al. 2019). The four main challenges facing value-based care in the OR include: staff retention, risk reduction, process inefficiencies, and the hidden costs of bundling. Technological advancements in OR equipment holds the greatest promise for improvements in value-based care.
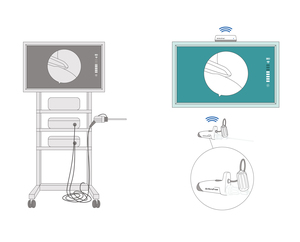
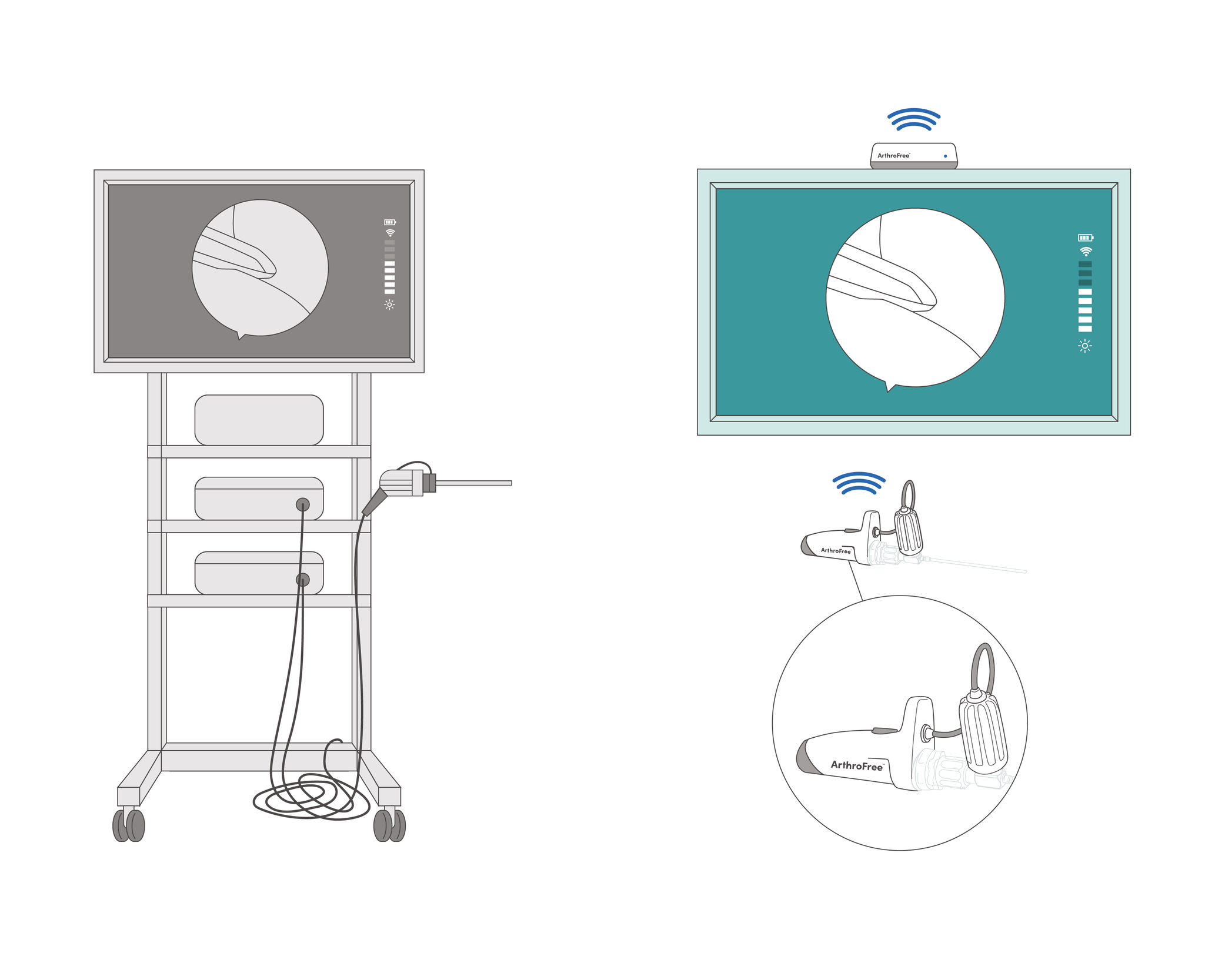
Arthroscopic cameras have undergone incremental advancements over the last 50 years. From the incandescent era to the fiber optic era med-tech companies have repeatedly refined the image quality, monitor size, latency, and data capture. However, these cameras continue to be tethered by light and power cords (Williams and Gupta 2022). The FDA-cleared ArthroFree wireless camera system (Lazurite LLC, Cleveland, Ohio) eliminates the need for power and light cables (Figure 1). We expect ArthroFree to improve the efficiency of arthroscopic equipment set-up and take-down, decrease the workload of OR nurses/scrub technicians, improve ease of surgeons movements, and reduce overall OR case cost.
This comparative simulation study of ArthroFree and a conventional camera system included analyses of: set-up and take-down times, cost per case, and other efficiencies. This study also surveyed OR nurses and scrub technicians on user experience metrics.
Materials and Methods
To analyze the set-up and take-down times of the two different arthroscopic cameras under simulated OR conditions, thirteen experienced OR nurses and scrub technicians were recruited to participate in the study. A brief tutorial on the components and proper use of the camera was given (Figure 2). Set-up time was recorded in seconds from the time the instrument was first touched to the time it was white balanced and ready for use. Take-down time was recorded in seconds from the time the instrument was picked up for disassembly to the time it was placed in the sterilization tray.
Each OR nurse or scrub technician was provided a set-up and take-down trial run. Each participant also had the opportunity to serve as the scrub nurse with the other serving as the circulating nurse. Both set-up and take-down were completed by each OR nurse/scrub technician pairing. Three sequential trials using the wired camera system were followed by three sequential trials of the wireless camera system.
From the data collected, OR set-up, take-down and total time efficiency were determined (% increase in efficiency = time difference between the wireless camera and the wired camera divided by the wired camera time times 100). OR cost savings estimates per case were calculated based on time savings and cost per minute for OR time.
Statistical analysis was completed using Stata (Stata Corp, College Station, TX). Means, standard deviations, and 95% confidence intervals were calculated. P values were determined using an ANOVA analysis.
To determine the potential benefits of a wireless surgical camera, five additional circulating OR nurses—along with the thirteen OR scrub nurses and scrub technicians (total of eighteen)—were administered a 5-point Likert scale questionnaire (Table 2).
Results
Set-up Times
The wired surgical camera mean set-up time in seconds +/- SD (standard deviation) was: 56.1 secs +/- 17.39. The wireless surgical camera mean set-up time was: 31.5 secs +/-8.52. The wired-wireless mean difference was 24.5 secs +/-16.03, with (p = 0.0001) (Figure 3).
Take-down Times
The wired surgical camera mean take-down time was: 21.0 secs +/-6.99. The wireless surgical camera mean break-down time was 16.1 secs +/-6.39. The wired-wireless mean difference was 4.9 secs +/-7.97 (p = 0.0458) (Figure 4).
Total Time
The total time for the wired surgical camera mean was 77.0 secs +/-16.94. The total time for the wireless surgical camera mean was 47.6 secs +/-12.62. The wired-wireless mean difference was 29.4 secs +/- 16.18, (p < 0.0001) (Figure 5 and Table 1).
Set-up, Take-down, and Total Time Efficiency
The wireless system was more efficient overall by 38.1%. Set-up time was decreased by 43.7% and take-down by 23.3%.
Cost Savings
Cost per minute of OR time was taken from three different published studies (Shippert 2005; Childers and Maggard-Gibbons 2018; Chang et al. 2019) to calculate cost savings. In this setting, the wireless arthroscopic camera saved 29.4 seconds or 0.49 minutes. The cost savings per case would therefore be $9.80 (Shippert), $18.00 (Childer) and $117.35, $92.64, and $80.41 for 30-, 60-, and 120-minute operative procedures (Chang).
Questionnaire Responses
On a 5-point Likert scale, the OR nurses and scrub technicians gave ArthroFree for all eleven questions a mean score of 4.69 (std: 0.52) (Table 2). ArthroFree scored highest (4.82) on the statement: “Having no light and power/data cables will have a positive impact on overall efficiency.” It scored the lowest on the statement: “Preparing the ArthroFree System for transport to SPD increased my efficiency.”
Discussion
This study demonstrates that a wirelss arthroscopic camera saves time, is more efficient and reduces cost per case vs a wired arthroscopic camera in terms of set-up, take-down, and total time in a simulated OR setting utilizing operating room nurses and scrub technicians with arthroscopic OR experience. Surveys of the participating OR nurses and scrub technicians demonstrated high scores for the wireless camera in terms of ease of setup and takedown, and the prospects of improving patient safety, simplifying duties, reducing job stress, and improving OR efficiency. In Shippert (2005), cost estimates for one minute of operating room time vary from $20 to over $100 per minute. Childer’s study (2018) based on data collected from 2005 to 2014 reported a mean cost of $36-$37 per minute. A more recent study (2019) by Chang taking data from 103 Ohio hospitals noted that after considering OR set-up costs, the per minute charges for 30-, 60- and 120- minute operative procedures were $239.50, $189.07, and $164.12, respectively. The total average cumulative time savings for set up and take down was 0.49 minutes representing a 38 % improvement and a prospective cost savings of $9.80 to $117.35 per case with use of a wireless surgical camera.
The US healthcare system is a $3.6 trillion industry (2018). It is estimated that 30% is wasted (unplanned cost). In a multicenter study by Dreyfus, Nair, and Roasals (2020) observing surgical cases, the researchers found an extra 5 to 10 minutes in delays resulted in $1,800 of unplanned cost per case. Hospitals generate 50% of their income from the OR while the OR accounts for only 25% of the expenses (Etges et al. 2022). Fifty percent of these costs are fixed costs primarily in the form of staffing costs. The surgeon represents 35% of the overall cost of surgery and 66% of the in-OR cost. Therefore, increases in case times results in increased staffing costs. Additionally, longer anesthetic times means increases in postoperative complications such as nausea, vomiting, and grogginess—all of which can delay patient discharge. Cheng et al. (2018) found that for every minute a patient spends under anesthesia their risk of a complication increases by 1%. Healy, Muller, and Campbell (2016) found the average cost of a surgical complication is $19,626. While the savings in this study seem modest for any given case, a study by Brodsky (1998) noted that saving two seconds per case could result in annual savings as high as $17,000.
Less equipment to perform a given surgery means less potential equipment failures and OR delays. Both systems rely on a surgical tower (or equivalent), with a data information box and a surgical monitor, as well as scopes and couplers, as needed. The conventional camera system includes the camera with power cord, a light cable, the power/video box, and the light box. The ArthroFree System includes the wireless camera, receiver, rechargeable batteries, and a battery charger. The ArthroFree System requires fewer box (or tower) components, and it’s designed to be compatible with existing arthroscopic lens/couplers, monitors, and patient data information boxes. It was also designed so surgeons, ASCs, and hospitals would not have to purchase a whole new system thereby reducing capital outlays. The components of the wired camera systems that the ArthroFree System displaces (the camera heads, light cables, light box, and video/power box) an average list price of $158,000. The ArthroFree wireless camera system is priced at the average, but the projected cost of ownership is strikingly lower due to lower associated consumable and reprocessing costs. Projections of cost per case for the wireless system are 20.4% lower than the average conventional camera system (LLC 22AD).
Fewer components means less equipment to maintain, refurbish, and replace. For the surgical processing department this means less to clean and less to reprocess and sterilize. At University Hospitals (Cleveland, Ohio) it costs $19 to clean a light cable. They perform an average of 162 arthroscopic cases per month and estimate that eliminating the light cable alone would save $37,000 per year.
The ArthroFree System was designed to free surgeons from the tethers of the surgical tower. It will allow surgeons more ergonomic and efficient surgical movements, which is expected to lead to shorter procedures. Likewise, the prospect of fewer items in the sterile field offers numerous advantages. Removal of the two cables crossing the sterile field is likely to reduce the chance of sterile field contamination. The circulating nurse is no longer involved in camera set up and take down. While there are no direct cost savings in this, it enables the circulating nurse to focus on helping anesthesia and with patient safety—both of which can improve OR efficiency and help prevent costly complications. A wireless camera is also expected to make the OR a safer place for patients and staff. Elimination of light and power cables means reduced risk for trips and falls by the OR staff and eliminates light cable related OR fires and patient burns. The camera is designed to be balanced once in a joint—unlike wired cameras, which are tail heavy due to the drag and weight of the cords. In a pilot human factors study, surgeons’ feedback on the camera has been positive in terms of weight/balance, no discernible latency, and maneuverability (Williams and Gupta 2022). Over 90% felt they could perform surgery as easily as they do with their current wired systems. These results suggest strong surgical adoption of a wireless camera system.
A drop-in compatible wireless arthroscopic camera system gives hospitals and ASCs the opportunity to move away from bundled contracts (e.g., video systems plus disposables and implants). Value-based care will continue to look for ways to reduce costs and improving inefficiencies. Hospitals and ASCs engaged in bundled contracts are shielded from knowing the true costs of the implants and disposables they purchase. The arthroscopic equipment companies have to markup disposables and implants significantly to make the tower/wired arthroscopic system appear “free”. In addition, the buyer must use a predetermined number of disposables/implants per year. If they fail to meet that number, they must pay a hefty surcharge. For hospitals and ASCs there are tremendous savings to be had by unbundling the disposables and implants.
Staff shortages and turnover are major problems for hospital and ASC operating rooms. OR nurses and scrub techs are under increasing stress and risk of burnout. The average cost to replace a bedside RN is $46,100, and it takes an average of 87 days (additional lost productivity cost) to find a replacement. The turnover rate of operating room RNs in 2021 was 18.8%. It took an average of 97 days to find an experienced replacement (NSI Nursing Solutions Inc. 2022).
The fear of an OR fire and patient burn due to the high-heat light source of current wired camera systems can be a big stressor for OR nurses and scrub techs. Medical equipment and documentation programs that enable the OR to function in an easier and more efficient manner have the potential to alleviate OR staff stress and turnover. The OR nurses and scrub techs gave the ArthroFree wireless camera system high marks (Likert scale 1-5) for improving safety (4.8), making their jobs easier (4.7), reducing their overall level of stress (4.5), improving OR efficiency (4.8), and ease of use (4.7). Medtech designed with nurses in mind should help OR administrators with staff retention and recruitment.
This study draws upon recent work (Williams and Gupta 2022) on the OR set-up, take-down, and total time of a wireless camera system vs a wired camera system. One limitation of the study was that it did not include the typical distractions common in operating rooms. The OR nurses and scrub technicians had varying degrees of experience with arthroscopic equipment—which is reflective of typical OR staffs. The lack of the normal OR distractions led to very efficient set-up, take-down, and total times. In a live OR setting, set-up, take-down, and total times will undoubtedly take longer due to all the other OR tasks occurring simultaneously. RNs with less experience with arthroscopic equipment will take longer to set-up and take-down the equipment. Future wired vs wireless camera system studies in a live OR setting will help to determine more accurate time savings, efficiencies, and cost savings. After using the ArthroFree System in this study, the OR nurses and scrub technicians felt strongly that it will improve patient safety, make their jobs easier, reduce their overall level of job stress, improve OR efficiency, and was easier to set-up, use, and take-down.
The struggle to deliver affordable healthcare is real. A wireless arthroscopic camera system appears likely to support value-based care in terms of staff retention, reducing complications, improving OR process efficiencies, and breaking down the hidden costs of bundling.
Summary
The ArthroFree wireless surgical camera was 44%, 23%, and 38% more efficient than a wired surgical camera in set-up, take-down, and total time in this OR simulation study. The projected cost savings per case vary from $9.80 to $117.35 per case and will depend on each individual institution’s cost per minute of OR time. The OR nurses and scrub technicians who participated in this study gave high scores (mean 4.67 out of 5) for ArthroFree’s ease of set-up and take-down along with improved patient safety, making their jobs easier, reducing their overall level of job stress, and improving OR efficiency.
Acknowledgments
The authors would like to thank Randal Doane, Ph.D., for his help editing this manuscript.




_times_by_nurse.png)
_times_by_nurse.png)
_times_by_nurse.png)




_times_by_nurse.png)
_times_by_nurse.png)
_times_by_nurse.png)