Introduction
A scaphoid fracture commonly encountered in Orthopaedic general practice. It poses the problems of delayed diagnosis, treatment and complications like non-union, AVN and wrist degenerative arthritis (Cooney, Dobyns, and Linscheid 1980). A non-displaced scaphoid fracture treated conservatively needs prolong plaster cast immobilization, which it is not preferred by most the patients (Russe 1960).
There have been different methods of surgical treatment options since 1970’s from open reduction internal fixation to percutaneous fixation (Kamineni and Lavy 1999). K-wires and different rigid implants like a Herbert screw, headless screw and compression screws, are used along with bone grafting and vascularized bone grafting. In spite of advancement in techniques and implants the complications for this fracture remains as high as 10%.
Internal fixation of scaphoid fractures is currently recommended, which facilitates fracture healing and lower rates of long-term complications compared to the non-operastive management (Russe 1960). Commonly used internal fixation devises includes Kirschner (K) wires and compression screws (Tomaino, King, and Pizillo 2000; Trumble and Nyland 2001).
The percutaneous technique (Haddad and Goddard 1998) has advantages over open surgical fixation, where the vascularity of the fragment is of utmost importance in fracture healing. Botte et al (Botte et al. 1988) described the vascular effects of volar and dorsal operative scaphoid exposures.
A dorsal approach with percutaneous fixation address all types of scaphoid fractures. The current trend of fixation of scaphoid fracture is by dorsal approach with rigid compression screws and headless screws (Herbert and Fisher 1984; InoGe and Tamura 1991). Rigid fixation with the screw, after drilling the scaphoid delays fracture healing due to the disruption to the soft tissue, bony architecture and the vascular supply to the scaphoid fracture fragments.
The objective of an ideal recommendation for scaphoid fracture fixation implant would be one that causes the least damage to the soft tissue, hold the fracture fragments in axial alignment and in compression with relative stability. Hence the straight K-wire is not ideal.
The implant, when placed along the central axis of the scaphoid gives the best chances for secure fixation and fracture union (Adams et al. 1988).
When several different scaphoid fixation screws were studied for the time to failure by cyclically loading, resistance to failure was related to the radius of the screw to the fourth power (Toby et al. 1997).
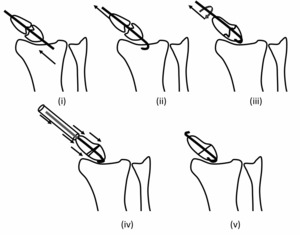
A K-wire which is placed axially along the anatomical long axis of the scaphoid, which is hooked proximally and pulled to compress on the distal fragment can achieve double compression to the fracture site. The distal fragment is an anvil on the proximal fragment to achieve double compression to the fracture site to achieve union.
The bending of the K-wire hooks the proximal fragment and also resists it from migration. The disadvantage of the K-wire of not achieving compression is overcome by bending and axial loading.
We propose a simple concept of placing a K-wire along the anatomical axis across the fracture site, bending it at one end so as to hook the proximal fragment and pulling the K-wire at the other end to compress the fracture site. This gave us the innovative idea of Axial Loading and Compression Fixation with a K-wire (ALCF technique).
Background story of ALCF Technique
This technique happened accidentally in our hands, while we were doing percutaneous cannulated Herbert screw fixation in our institution. The instrument set was used by many surgeons at many hospitals in the state. The set guide wire was worn out & bent, which had high chances of breakage. We realised this after two consecutive incidents.
Twice the guidewire got bent and broke at the dorsal proximal entry point and while cannulated drilling, we had to abandon the procedure. With the broken bent K-wire tip at the proximal end, we attempted to pull out the K-wire from the volar end, to our surprise the fracture margins got aligned and approximated. This led us to conclude to retain the broken guidewire (1.5 mm thickness) in the scaphoid. The other end of the guide wire was cut short on the volar side in the thenar muscles and buried it under the skin. We consider the retained broken bent guide wire as an implant. These 2 cases of fracture scaphoid waist and proximal pole went onto healing in 10 and 12 weeks.
Materials and Methods
All patients had surgery between January-2017 to January-2020 in our institution Jubilee Mission Medical College, Thrissur, Kerala and were retrospectively reviewed. Patients with concomitant injuries such as distal radius fractures, dislocations and compound fractures were excluded from the study. Patient age range was from 18 to 69 years, with an average age of 26.2 years. The right hand was involved in 11 patients and the left in 5 patients. 13 fractures involved the dominant hand. 12 patients were males and 4 were females. The fracture was acute in 10 patients of which 7 were trans-scaphoid displaced fractures sustained in motor vehicle accidents, three were lower pole displaced fractures sustained after a fall. 6 patients were scaphoid non-unions. All acute scaphoid fractures, patients were immobilized with a short below arm splint until surgery. All data extracted from patient charts were recorded on a standardised form. Patient’s demographic data, radiographs and clinical data were obtained.
Technique
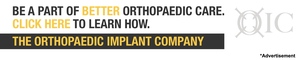
We place the wrist on the operating table after prepping up to the elbow in such a way that the surgeon can freely do supination and pronation at the wrist with free movement of elbow. C-arm was used to take images of the wrist in flexion, extension and neutral position with full pronation and supination of the forearm and ulnar deviation of the hand so as to visualize the scaphoid. Then the K-wire (1.2,1.5,1.8, 2 mm) is driven from the dorsal to volar wards into the scaphoid with wrist pronated and flexed in the centre-centre of the circle, "the ring sign". The K-wire is directed volar towards to the base of the thumb. The axial K-wire is placed along the long axis of scaphoid and confirmed on the C-arm image. Holding the fracture fragments of scaphoid in alignment is mandatory.
If the alignment of the fracture fragments of scaphoid are not well aligned, a second parallel K-wire of different thickness maybe used as a joystick to attain better alignment. Once the K-wire position and fracture fragment alignment are confirmed as satisfactory, the K-wire is advanced to pierce the skin at thenar eminence. Then the dorsal tip of K-wire is gently bent and cut at the skin level so as the bent tip can be buried dorsally into the skin keeping 3-4 mm, care to be taken not to hinge on the distal radial articular surface.
The volar tip of the K-wire is then pulled by manual loading gently such that it hooks at the proximal pole of the scaphoid confirmed on the C-arm image. The gentle pulling load with rotation of the K-wire help in compression of the proximal fragment to distal fragment and fracture alignment.
A stab skin incision is put at the volar exiting K-wire on the thenar eminence. A straight K-wire bender tube is mounted on the K-wire and hammered gently to anvil on the distal fragment of the scaphoid, thus will further compress the fracture fragments. Now the volar tip of the K-wire is bent and cut short so as to bury into the thenar muscle such that it is palpable on deep pressure 8-10 mm from distal pole of scaphoid.
Occasionally when the reduction is not satisfactory with the first K-wire, then the second K-wire is passed in the similar way so as to use it as joystick in the proximal fragment or the distal fragment and then similar axial loading compression applied as previously to achieve stable fixation. The position of the K-wire, single or double, is reassessed in the C-arm image before skin closure.
Post-operative
Wrist splint immobilization was used for a period of 2 weeks followed by a thumb splint for a period of 6 weeks. Radiological assessment of the wrist was at end of 6 and 12 weeks.
Assessments
Outcome was assessed for each patient at 6 weeks and 12 weeks after surgery. We used objective assessment of range of motion. Wrist range of motion was measured using a goniometer. Radiologic evaluation was used to assess fracture union. Fracture union was identified based on the presence of trabecular bridging across fracture site in at least 2 scaphoid views with no gaps seen in any of the radiographic views. Subjective assessments were performed by a 10-point Visual Analogue Scale (VAS) (1 indicated no pain and complete satisfaction, while 10 Indicated the worst pain and complete dissatisfaction). The patients were also evaluated by the Mayo wrist score. The Mayo wrist score was evaluated for overall functional recovery, interpreted as Excellent (90-100), good (80-90), satisfactory (60-80), and poor if below 60.
Results
The results of 16 patients treated for scaphoid fracture using ALCF technique were available for analysis. The average total flexion was 51.8 and the average was extension-63.4 at 3 months. This was comparable to contralateral normal, contralateral wrist.
Radiographs was evaluated for fracture union. Union was considered present if bony trabeculae crossed fracture site in AP and scaphoid view. At 3 months there was 100% union in our study.
Patient satisfaction was assessed with VAS score and MAYO wrist score. Our VAS score at 6 weeks was 5.5 and at 3 months it was 1.43. MAYO wrist score for functional recovery were interpreted as 81.31 (Good) and at the 3 months 95.18 (Excellent). Average time of removal of implant after radiological union was 8-10 months
Conclusion
ALCF percutaneous technique of K-wire fixation for any kind of scaphoid fracture is a safe and simple technique. The implant used, a K-wire, is cost effective treatment. It does not need any extra instrumentation. As the technique is percutaneous, there is low risk of infection, soft tissue damage, and injury to the vascularity of the scaphoid. The placement of the axial K-wire guide wire along the long axis of the scaphoid is a simple technique does not need a steep learning curve. The axial traction loading of the K-wire is a gentle manual procedure which can be observed under image intensifier to show us the impaction of the proximal fragment to distal fragment. Moreover, this axial compression of proximal fragment with the K-wire can assist in mild rotational alignment of the fracture fragment. Thus the entire procedure is gentle and with the smooth K-wire the bony architecture pattern of the scaphoid is not much disturbed unlike in screw fixation where drilling, compression with a threaded screw damages the bony architecture of scaphoid bone thus delaying fracture healing. The volar tip of the K-wire is cut short under the skin in thenar eminence for ease of removal from the healed fracture scaphoid.
Regarding the 2nd K-wire insertion, this helps in giving axial and rotational stability especially in displaced fractures with difficult reductions.
With this ALCF technique, all the fractures healed with no complications and good clinical and functional outcomes. The ALCF technique using K-wires gives relative stability to the fractured scaphoid and allows for early mobility with minimal morbidity. This technique is a day care procedure, under regional anastasia, economical, no special instruments needed and low morbidity hence patient’s friendly procedure.
Acknowledgments
We thank all our patients and members of the Department of Orthopaedics at Jubilee Mission Medical College and Research Institute, Thrissur, Kerala for their endless encouragement and contribution to this study.





_and_post_(ii)_plain_radiograph.png)
_and_post(ii)_implant_removal(iii)_plain_radiograph.png)






_and_post_(ii)_plain_radiograph.png)
_and_post(ii)_implant_removal(iii)_plain_radiograph.png)
