Background
Osteoarthritis (OA) is a major cause of pain and disability, with 18.8 million people being affected across the UK. In England, one in five people over the age of 45 has knee OA (Versus Arthritis, n.d.) and the rates are constantly increasing due to an aging population and a rise in obesity. Knee OA leads to major social, psychological, and economical burdens with a substantial financial burden to the individual and society. Overall annual costs of OA to the healthcare system are estimated to be £10.2 billion (Woolf 2018).
Total knee replacement (TKR) is considered the most common and effective treatment for end-stage knee OA. Yet, as with any surgical intervention, TKR poses some risks including post-operative complications, persistent pain, and the need for revision surgery (Weinstein et al. 2013; Wylde et al. 2011, 2018). Furthermore, TKR carries a high cost, which is expected to rise as the demand for TKR grows, adding yet a greater burden to the healthcare system.
Interestingly, since the COVID-19 pandemic and the need to postpone a huge number of surgeries, the waiting lists for TKR have grown exponentially, with the number of inpatient procedures rising by 73% compared to the previous year (Hampton et al. 2021). Healthcare systems are trying to address the backlogs, but with limited capacities for elective surgery, patients are left untreated, and the recovery from the backlog is much slower than required. Therefore, it is paramount that health systems look for effective alternatives for treating these cohorts with interventions that are able to significantly delay and potentially avoid the need for joint replacement surgery altogether where possible.
The National Institute of Clinical Excellence (NICE) guidelines outline core treatments such as education and exercise as first line care, progressing to more advanced biomechanical modalities such as valgus knee braces and orthotics along with pharmacological interventions and knee injections (Conaghan et al. 2008). With approximately 6-19% of all knee OA cases being considered severe and quality of life reported “worse than death” (Versus Arthritis, n.d.), effective treatments to delay surgery or alleviate symptoms while waiting for surgery are essential. One such intervention includes a non-invasive biomechanical device (AposHealth®) that manipulates the center of pressure (COP) to shift loads and train neuromuscular control. This intervention has been reported in randomized controlled trials and via real world evidence to significantly reduce pain, improve function and biomechanical indicators for disease severity that correlate with the likelihood of TKR (Reichenbach et al. 2020; Haim et al. 2012; Bar-Ziv et al. 2013; Elbaz et al. 2014).
Between 2017 and 2019, the biomechanical treatment (AposHealth®) was commissioned by an NHS Clinical Commissioning Group (CCG) as a non-invasive solution for patients that met the criteria for orthopaedic referral for TKR. The objective of the service was to improve the care of knee OA patients and manage their condition conservatively. This approach could also produce economic advantages from avoided costs associated with surgery, along with a system-wide solution to support and manage the elective backlogs. With over 2 years of data, the purpose of the current study was to examine the surgery avoidance rate amongst TKR candidates that received this intervention and assess its clinical effect over time.
Methods
The study was a retrospective analysis of 365 patients with end-stage knee OA that began treatment between November 2017 and November 2019 and were in treatment for at least 2 years. All patients had met the criteria for orthopaedics referral as set out in the CCG’s Value-Based Commissioning Policy and been screened by the CCG’s clinical triage team to ensure appropriate candidate selection (Table 1). Once referred into the service, patients were assessed by specially trained physiotherapists and suitable candidates were enrolled in the programme. The protocol was not approved by an ethics committee, however the local NHS Trust’s Clinical Audit Team reviewed and approved this research work as an audit on commercial activity. In addition, all patients that started treatment signed a consent that acknowledges that their data might be used for research purposes while maintaining their privacy.
Outcomes
The primary outcome measure was surgery avoidance rates at 2 years. All patients were contacted between June and November 2021, at least 2 years from commencing treatment to assess their surgical status. Patients that were lost to follow-up were either contacted by telephone or the data provided from the hospital databases regarding their surgical outcome. Secondary outcomes included changes in clinical outcomes evaluated at baseline, 3, 6, 12 and 24 months into the treatment. The WOMAC questionnaire and Oxford Knee Score (OKS) were used to assess changes in patients’ perception of pain and function (Hmamouchi et al. 2012; Lundgren-Nilsson et al. 2018; Harris et al. 2013). The OKS was developed and validated for use with individuals undergoing knee arthroplasty and measure outcomes following rehabilitation of patients with knee OA. OKS was completed by patients at 6-month intervals since commencing the biomechanical treatment.
The OptoGait system (Version 1.11) was used by trained physiotherapists to measure spatial-temporal gait parameters at each data collection point (Lee et al. 2014). Patients walked barefoot at a self-selected speed over a 4-m measurement area, with 2-m before and after to allow for constant velocity walking speed during data capture. Each gait test consisted of 4 lengths in which the mean values were calculated for each parameter. The parameters recorded include velocity (cm/s), step length (cm) and single-limb support (SLS) phase (% gait cycle). Step length and SLS were calculated for the less and more symptomatic limbs, respectively. For patients with bilateral OA, the more symptomatic limb was determined by the lower SLS at baseline. For patients with unilateral OA, the more symptomatic limb was the limb that was reported with OA.
Intervention
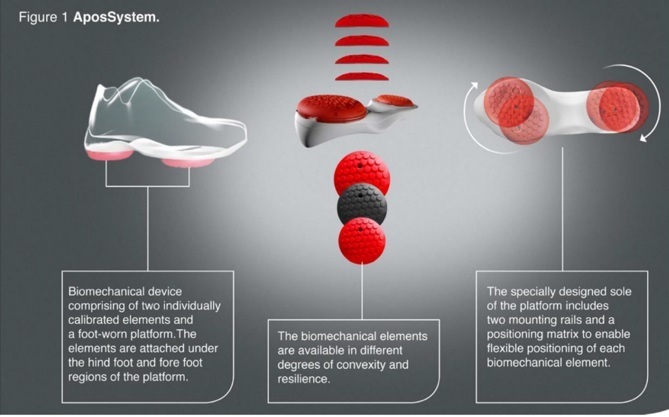
All patients received a personalized, non-invasive, home-based, biomechanical treatment that aims to alleviate knee pain and improve function (AposHealth®). The treatment is delivered via unique footwear (Apos device- see Figure 1; Apos in action - see video 1) that provides the platform to fit two convex pods to the plantar surface of the sole using screws. The pods cannot be attached to personal shoes and require a trained clinician to calibrate the device and locate the pods in the correct position based on treatment methodology. The clinician calibrates the devices to reduce pain in the knee whilst walking. By adjusting the location of the pods, it changes the ground reaction force (GRF) vector and reduces pressure on the area immediately (Haim, Rozen, and Wolf 2010; Haim et al. 2011). The convex nature of the elements induces a level of controlled perturbation and proprioceptive training causing muscles in the lower limb to work differently (Debbi, Wolf, and Haim 2012; Goryachev et al. 2011). The combination of altered forces and moments acting on the affected joint as a result of the device set-up, combined with controlled perturbation allowing a neuromuscular training response and carry-over effect to usual walking without the device to occur (Haim et al. 2012; Debbi et al. 2015).
The treatment combines three main elements: First, manipulating the center of pressure (COP) to reduce loads from the affected area in the joint. Second, neuromuscular training (via controlled perturbation provided by the shape of the biomechanical elements). Third, home-based training with the device in task-specific actions (i.e., the patient is instructed to wear the device and go on about their daily living). In addition, patients are also educated about the condition and ways to manage their symptoms. Following the initial consultation and calibration of the Apos device in the clinic, the patient received a home-based treatment plan from the physiotherapist. This includes wearing the device for approximately 20 minutes per day initially and the patient is instructed to wear the Apos device and go about his/her daily routine. A gradual increase in usage time is prescribed, often reaching up to 2-3 hours per day indoors. Patients were requested to return to follow-up appointments in which re-assessment of clinical outcomes and gait patterns were performed and the calibration of the Apos device is adjusted as indicated. Treatment plans were adjusted at each appointment, and patients were encouraged to continue to wear the device regularly at home as prescribed.
Statistical Analysis
Means and standard deviations were calculated for all dependent variables. To address our primary goal, the rate (and 95% confidence interval) of patients who had TKR, out of the total cohort was calculated at two time points: within 12-months and within 24-months (i.e., two years) since initial consultation. The independent-sample t-test were used to compare the baseline characteristics between patients who avoided surgery (i.e., non-TKR group) and those who progress to TKR within two years (i.e., TKR group). Change in clinical outcomes over time was assessed using the generalised linear mixed-models. Pain, function, gait velocity, step length and single limb support phase were compared across five time points including baseline, 3-month, 6-month, 12-month and 24-month follow-ups. The generalised linear mixed models were chosen as a preferred method to handle repeated measures with unbalanced sample size, resulting from patient progression to TKR, missed follow-ups during COVID-19 quarantine and attrition due to other medical and personal reasons. In addition, we calculated the Outcome Measures in Rheumatology Clinical Trials (OMERACT)-Osteoarthritis Research Society International (OARSI) responder criteria for clinically significant improvement for each of the patients (Pham et al. 2004). These stipulate either an improvement in total, pain or in function WOMAC sub-scales of at least 50% with a decrease of 2 cm on the visual analogue-scale for pain or function, or an improvement in both pain and function of at least 20% with a decrease of 1 cm on the VAS (Pham et al. 2004; Angst, Aeschlimann, and Stucki 2001). All statistical analyses were conducted by an independent biostatistician using SPSS software version 27.0 with significance levels set at p<0.05 (two-sided).
Results
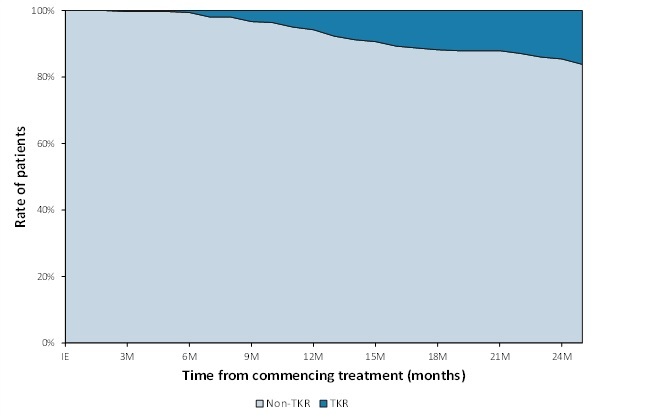
Three hundred and sixty-five (365) patients, 193 females (53%) and 172 males (47%) males with symptomatic knee OA participated in the study. Two years from commencing the treatment, 305 of the patients (84%) avoided TKR surgery. The rate of TKR within the cohort was 16% (95% CI 12% to 20%) at the 2-year time point, with 23 patients (6%) progressing to TKR within the first year, and a further 36 patients (10%) within the second year of follow-up (see Figure 2). Nine (9) patients (2%) deceased during the two-year follow-up. A comparison of baseline characteristics between those who underwent TKR surgery and those who avoided surgery at 2 years is detailed in Table 2. Significant differences existed between cohorts at baseline with the TKR group reporting lower OKS (19.8 vs 21.8 respectively; p=0.045) and SLS of the involved limb (33.9% vs 35.0%; p= 0.018, respectively) signifying higher pain and functional disability. No other significant differences existed between cohorts.
With regards to the clinical outcomes, of those that did not progress to TKR or decease, 91% had data at 3 months, 70% at 6 months, 69% at 12 months and 63% at 24 months. Table 3 summarises the changes in clinical measures (WOMAC, OKS and gait parameters) over the time periods. It shows significant improvements in WOMAC pain and function subscales of 34% and 31% respectively at 3 months, increasing to 42% and 39% at 6 months. These continued to improve to 49% and 54% respectively over the 2 years. 67% of patients met the OMERACT-OARSI criteria for clinically significant improvement (Pham et al. 2004). OKS improved by 7.6 points in the first 6 months of treatment, and further to 10.6 points at 2 years, meeting the minimally important change of 7 points (Harris et al. 2013). Table 3 also displays the trend of improvement in all spatial-temporal gait measures over time (p<0.001).
DISCUSSION
The purpose of this audit was to look at surgery avoidance at 2 years following a non-invasive biomechanical intervention for patients eligible for TKR as an alternative to surgery. The aim of the study was to investigate whether the provision of this treatment intervention could help to address the challenges of long waiting lists, the ongoing decrease in average surgical age and its future implications, along with the financial burdens felt within the health system. The results of the current study suggest that 94% of patients with severe knee OA, otherwise eligible for TKR, avoided surgery at 1 year post commencement of treatment and 84% of patients avoided surgery at 2 years. These results are relevant considering the rising prevalence of knee OA and the alarming demand for TKR globally, with an estimated 130 million people suffering worldwide by 2050 (Wittenauer, Smith, and Aden 2013).
Within the UK alone, it is conservatively projected that by 2035 there will be 120,000 TKR’s annually, contributing significantly to the financial burden on the healthcare system (Culliford et al. 2015). Alternative models have suggested figures to be as high as 1.2 million, but either way, there is an acknowledgement of the lack of system capacity to be able to manage such rises (Culliford et al. 2015). There is a growing need for effective non-surgical interventions for knee OA, delaying the need for TKR or avoiding it altogether. A paradigm shift is needed to focus efforts on treating patients at high-risk earlier in the disease progression (Hunter 2011), or utilising more specialist modalities that can help minimise flow to surgery where advantageous and appropriate. The results of this study suggest a significant reduction in rates of TKR over 2-yrs. Future studies should examine the cost-effectiveness of this intervention in the short and long-term.
Alongside surgery avoidance, patients displayed significant improvements in clinical outcomes, including a reduction of 34% and improvement of 31% in pain and function respectively within 3 months. These improvements exceed the recommended Minimal Clinically Important Difference (MCID) of a 17%-22% reduction (Bennell, Hunter, and Hinman 2012) and improved further across the 2 years (see Table 3). In addition, 67% met the OMERACT-OARSI guidelines for clinical response, signifying true positive impacts felt by patients (Bennell, Hunter, and Hinman 2012). The changes in the OKS also reflect these positive changes in pain and function, with improvements meeting the MCID for clinically meaningful improvement at all time points (Harris et al. 2013). These results suggest that treatment with the biomechanical device significantly improved patient symptomology and may have consequently enabled the majority to re-consider and delay the need for TKR surgery for at least 2 years.
Patients also displayed improvements in various key gait metrics associated with knee OA (Elbaz et al. 2014, 2012), suggesting improved function with treatment. The changes in gait velocity over time could have substantial implications for patients. Studenski et al (2011) reported a correlation between walking speed and survival, suggesting that survival increases across the full range of gait speeds, with significant increments per 10cm/s (Studenski 2011). The average change in gait velocity in the current study was 18 cm/s. Interestingly, the recommended walking speeds for pedestrian crossings are typically between 91 to 107 cm/s. Patients in the current study started with an average gait velocity that was lower than this suggested threshold but have reached the clinical milestone after three months (recall Table 3) and further increased their velocity over the two years. The practical implications of these outcomes suggest that patients can now cross the street safely and independently.
The improvement in SLS symmetry and SLS of the symptomatic leg over the course of the treatment is also of interest. Previous studies have suggested SLS% to be a good indicator of knee OA severity, pain, function and risk of TKR (Elbaz et al. 2014, 2012). Positive changes in this measure over the treatment programme suggest that patients become less “at risk” of requiring a TKR to manage their condition (Elbaz et al. 2014; Herman et al. 2018). This is particularly relevant considering that patients who opted for TKR surgery during the study period demonstrated significantly lower SLS of the symptomatic leg at baseline (Table 2). These results further support gait metrics being an objective marker for identifying those patients most likely to require TKR versus those that may respond to more conservative measures such as the biomechanical treatment. Alongside current guidelines for assessing patients’ suitability to surgery such as imagery, PROM’s, and patient symptomology, gait metrics such as velocity and SLS may be an additional assessment tool and objective way of tracking clinical success.
The limitations of this study should be acknowledged. Firstly, this was a retrospective study with no control group to compare the outcomes. The NHS in England established a maximum waiting time target of 18 weeks to ensure that hospitals make it a priority to deliver treatment in a timely manner. This is the time from receiving the referral to receiving treatment. The average wait time in the locality for this project is 26 weeks. This timeframe is well within the follow-up duration of this trial of 2-yrs), hence it can be assumed that most patients should have had a knee replacement within two years. That said, a study by McHugh et al. suggests that in the UK, 33% of the patients that are referred to secondary consultation by a general practitioner will undergo surgery within 12 months (McHugh, Campbell, and Luker 2011). Even with this conservative number, a 33% decay rate at 12 months is over 5-times more than the 6% seen in the present study. To better assess the differences in decay rate between TKR candidates that were treated with this intervention relative to controls, a future randomised control trial is recommended. Secondly, this was a retrospective analysis, and some clinical data is missing. Although clinical outcomes were secondary outcomes of this study, only 63% of the patients had clinical measures at two years. The COVID-19 pandemic meant patients that would have normally been seen in clinic were not able to be seen for extended periods, meaning a lack of clinical support and progression, and therefore contributed to dropout and opting for surgery. We used ITT statistical procedure and found significant improvement over time that suggests a long-term effect, however additional studies should further investigate the long-term effect of this treatment. Furthermore, it can be argued that with COVID-19 halting elective surgeries, including TKR, the decay rate might be underestimated. A sub-group analysis of patients that were enrolled until April 2018 and would have completed 2-yrs of treatment pre-COVID, showed a decay rate of 20% at two years (compared to the reported 16%). This sub-group analysis suggests that COVID had minimal effect on the decay rate reported in this study.
In conclusion, the administered biomechanical treatment led to 84% surgery avoidance for at least 2 years among patients that would have otherwise opted for TKR surgery. With the additional pressures that the COVID-19 pandemic has placed on elective care pathways, offering a non-surgical alternative to those already on waiting lists may assist in managing the large backlogs, allowing healthcare systems to prioritize those most in need. The long-term clinical outcomes suggest lasting pain reduction, and an improvement in disability and gait patterns. Whilst further studies are required to fully understand the long-term clinical effect of this treatment, this study suggests that it may provide positive clinical implications for patients, with the potential to provide an effective alternative to surgery for healthcare systems to manage knee OA patients in community settings.
Abbreviations
OA: Osteoarthritis; NICE: National Institute of Clinical Excellence (NICE); TKR: Total knee replacement (TKR); PROM’s: Patient reported outcome measures (PROM’s); LED: Light emitting diode (LED); SLS: Single-limb support (SLS); VAS: Visual analogue scale (VAS); COP: Center of pressure (COP); OMERACT-OARSI: Outcome Measures in Rheumatology Clinical Trials (OMERACT)-Osteoarthritis Research Society International (OARSI); OKS: Oxford Knee Score (OKS); CCG: Clinical Commissioning Group (CCG); GRF: Ground Rection Force (GRF)