This is the fourth of four award-winning presentations from the inaugural Medical School Orthopedic Society (MSOS) symposium. MSOS is a medical student-run initiative with a mission to support “research and educational opportunities for students interested in orthopedic surgery.”
This presentation was given by Derrek Edukugho, a fourth-year medical student at Boonshoft School of Medicine.
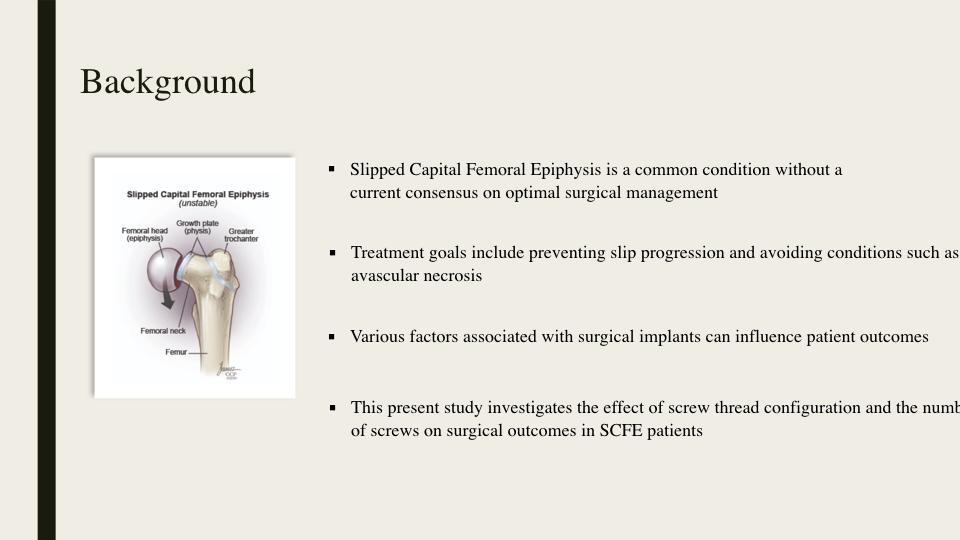
Slipped capital femoral epiphysis (SCFE) happens when the femoral head slips off the growth plate. It is a common condition without a current consensus on optimal surgical management. Treatment goals include preventing slip progression and avoiding conditions such as avascular necrosis (AVN). Various factors associated with surgical implants can influence patient outcomes. This study investigates the effect of screw thread configuration and the number of screws on surgical outcomes in SCFE patients.
In other studies, the majority of data has been obtained regarding the placement and amount of implants used in treatment. There has not been extensive data on the screw thread configuration, whether it is partially or fully threaded. In this study, we hypothesized there would be no difference in the surgical outcomes between partially or fully threaded screw constructs.

This was a retrospective study of n = 158 patients who underwent cannulated, stainless steel, in situ screw fixation of a SCFE affected hip between January 2005 and April 2018. The major variables we considered included return to the operating room (OR), AVN, hardware failure removal, and femoroacetabular impingement (FAI) recorded as binary variables (no/never, yes/ever).
We used univariate logistic analysis to test for the effects of covariates on outcomes. Multivariate logistic regression analysis was used to test for the main effects of each primary surgical detail and preoperative stability, as well as the number of screws.
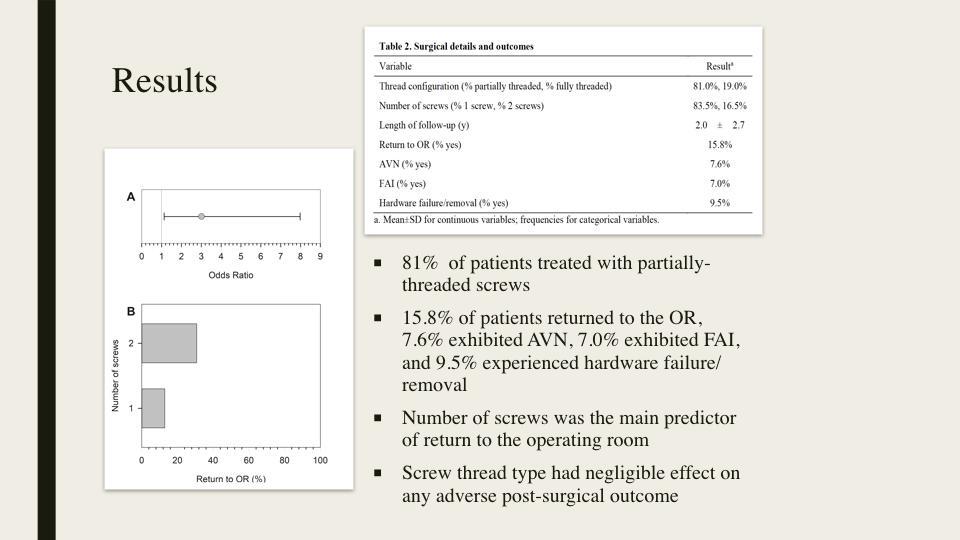
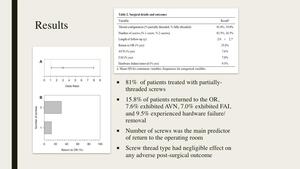
81% of patients were treated with partially-threaded screws, which could suggest a bias or preference of the surgeon. 15.8 . Other results show that 15.8% of patients returned to the OR, 7.6% of patients exhibited AVN, 7.0% of patients exhibited FAI, and 9.5% of patients experienced hardware failure and removal. Overall, the number of screws was the main predictor of return to the OR (Figure B). Screw thread type had negligible effect on adverse operative outcomes.
A common theme we observed was that the effect of thread configuration was very minimal. The most important factor was rather the number of screws to achieve fixation. Additional factors on outcomes included physeal stability, laterality of diagnosis, and, to a lesser extent, age and sex. Females had a preponderance of post-surgical complications.
The reason that the number of screws had such a large role is that the more screws used increases the intra-articular penetration and the chance of improper placement, which then increases the risk of serious complications. It should be noted that in cases with unstable slips, a surgeon might need to use more than one screw to achieve adequate fixation. The fear of complications should not prevent the utilization of an extra screw if deemed necessary.
Limitations for our retrospective single institution study is that data was not available for all patients. This led to the exclusion of some patients and introduction of potential bias.
In conclusion, the rates of hardware failure, return to the OR, AVN, and FAI did not necessarily differ between partially or fully threaded screws, but rather between the number of screws used. When compared to single-screw fixation, the use of 2 screws was associated with an increased likelihood of return to the OR, hardware failure, and AVN (when used in a stable slip). Our findings suggest that screw thread configuration has no impact on complication rates, whereas screw number is an important consideration in SCFE fixation.
Disclosures
None of the presenters or authors listed have a financial disclosure or conflicts of interest with the material in this presentation.