INTRODUCTION
Total shoulder arthroplasty (TSA) has revolutionized the treatment of glenohumeral osteoarthritis and other shoulder degenerative joint disease, reducing pain and restoring functional mobility (Jensen et al. 2021; Mattei et al. 2015). The primary goal of anatomic TSA is to restore the normal functional anatomy of the glenohumeral joint by replacing the humeral head and glenoid surfaces. Much of the modern shoulder arthroplasty designs originated from the ideas of Dr. Charles Neer, who first started using stemmed humeral components in the 1950s and then introduced the glenoid component in the 1970s (Boileau et al. 2006). Over the years, much research and time has been invested into refining these designs and making modifications to improve the biomechanics, durability, and stability of shoulder arthroplasty components. One area that has been continually investigated is the length of stem of the humeral component.
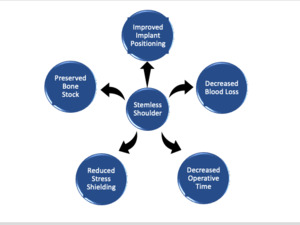
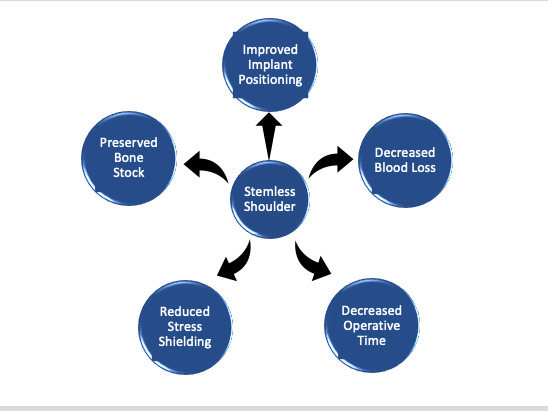
Early humeral component designs involved using a long humeral stem. These longer humeral stems have several advantages, including stronger distal fixation and thus a lower risk of loosening (Owens, Sperling, and Cofield 2014). However, they have disadvantages as well, including a greater risk for stem-related complications such as stress shielding, intraoperative humeral fractures, and periprosthetic fractures, which can lead to increased operative times and greater blood loss (Cisneros et al. 2016; Oh and Lim 2018). Additionally, significantly more bone is removed during implantation. Implant design and research have therefore moved towards intermediate length, short length, and now even completely stemless humeral implants. The first stemless shoulder arthroplasty system to be used was the Biomet Total Evolutive Shoulder System (TESS, Biomet, Warsaw, IN, USA) in 2004 in Europe. Clinical outcomes and other data using stemless implants, including those of the TESS System, have been promising (Berth and Pap 2013a; Uschok et al. 2017; Spranz et al. 2017; Beck et al. 2018; Maier et al. 2015; Churchill et al. 2016; Hawi et al. 2017; McMillan et al. 2021). With much recent discussion around these implants, there is a need to review the essentials of these implants to increase awareness for shoulder surgeons and promote further research. This article will provide a concise review on stemless humeral implants, including an in-depth exploration of their advantages, disadvantages, and future in anatomic TSA as shown in Figure 1. A postoperative x-ray is shown in Figure 2.
ADVANTAGES
Decreased Operative Time
Surgical operative time is an important variable to target for improving patient outcomes and patient safety. It is well established that surgeries of longer length have disadvantages, including a greater risk for infection and higher healthcare costs. For example, in a study of 10,082 patients undergoing total shoulder arthroplasty (TSA), an increase in operative time significantly increased the risk for any complication, and specifically the risks of anemia requiring transfusions, peripheral nerve injury, and urinary tract infections (Wilson et al. 2021). Thus, the benefit of a shorter operative time using stemless implants is important to highlight (Heuberer et al. 2018; Berth and Pap 2013b). In a study of 82 patients with primary shoulder osteoarthritis, patients who underwent surgery using a stemless shoulder prosthesis had an average operative time of 91.5 minutes whereas surgeries using a conventional stemmed shoulder prosthesis had an average operative time of 106.2 minutes (Berth and Pap 2013b). Another study by Heuberer et al also showed similar findings. Among patients undergoing TSA, the average operating time using stemless humeral implants (95.7 minutes) was significantly lower than those surgeries using stemmed humeral implants (120.7 minutes) (Heuberer et al. 2018).
Decreased Blood Loss
Patients with greater estimated blood loss are more likely to require blood transfusion after TSA (Burns et al. 2019). These patients receiving blood transfusions after TSA are at a greater risk for a longer hospital length of stay as well as higher total charges than those without a transfusion (Kandil et al. 2016). The advantage of decreased blood loss with stemless humeral implants is important for patients and surgeons. Prior research has shown this benefit17. In a study of patients with primary osteoarthritis undergoing TSA, those who received a stemless shoulder prosthesis had an average estimated blood loss of 496.3 mL whereas those who received a conventional stemmed shoulder prosthesis had an average estimated blood loss of 593.4 mL (Berth and Pap 2013b).
Reduced Stress Shielding
The use of stemmed implants directly and indirectly influences bone strength and bone quality. Stem length and design significantly influence stress shielding (Denard et al. 2018; Nagels, Stokdijk, and Rozing 2003). Stress shielding (stress protection) occurs when an implant reduces bone stress and changes load transfer patterns, leading to bone remodeling and loss of bone density (osteopenia) (Huiskes, Weinans, and van Rietbergen 1992; Shishani and Gobezie 2017). This in turn reduces the support of the implant and increases risk for aseptic loosening and periprosthetic fractures (Nagels, Stokdijk, and Rozing 2003; Fram, Elder, and Namdari 2019; Tigges, Stiles, and Roberson 1994). Longer humeral stems have been shown to be associated with high rates of stress shielding and other radiographic changes (Denard et al. 2018; Verborgt, El-Abiad, and Gazielly 2007; Raiss et al. 2014; Razfar et al. 2016). Razfar et al conducted a study using finite element methods and found significant changes in average cortical bone stress for standard length humeral stems compared to stemless implants (Razfar et al. 2016). The authors concluded that reductions in stem length resulted in cortical stresses that better mimicked the intact humerus state, and that using shorter stems may at least partly reduce stress shielding (Razfar et al. 2016). Reductions in stress shielding are one driving force in the push for using stemless implants (Denard et al. 2018; Razfar et al. 2016; Arno et al. 2012; Bieger et al. 2012).
Preserving Bone Stock
In contrary to stemmed implants, stemless humeral implants rely on cementless metaphyseal fixation (Willems et al. 2021a). There is no reaming or violation of the humeral canal, preserving significantly more native bone relative to short-stemmed and long-stemmed implants (Hawi et al. 2016). Critical bone stock is preserved that can help facilitate potential future revision arthroplasty surgeries (Geurts et al. 2010; Schoch et al. 2021).
Improved Implant Positioning
Improper placement of the humeral stem can influence the humeral head position and thus the glenohumeral articulation(Iannotti, Lippitt, and Williams 2007; Terrier et al. 2010; Nyffeler et al. 2004). Thus, eliminating the humeral stem may reduce the risk of malpositioning, which could influence joint kinematics and potentially clinical outcomes (Iannotti, Lippitt, and Williams 2007; Terrier et al. 2010; Nyffeler et al. 2004; Huguet et al. 2010).
LIMITATIONS AND DISADVANTAGES
Despite the advances made in stemless humeral implant design and its associated advantages it is important to discuss several limitations and disadvantages. First, stemless implants are dependent on proximal bone quality for fixation. As such, stemless humeral implants are contraindicated in patients with acute proximal humerus fractures, inadequate metaphyseal bone stock, or extensive cystic or necrotic changes (Plachel and Scheibel 2017; Willems et al. 2021b). In these cases, other alternatives, including stemmed humeral implants, may be necessary. Second, the lack of distal diaphyseal fixation with stemless implants could cause an increased risk of loosening. This is an area of continual investigation. Finally, as with many other new technologies and products, stemless implants may have higher healthcare costs. Cost-utility analyses are in progress to better understand the economic ramifications of stemless humeral implants for both patients and health systems (Nyring et al. 2020).
FUTURE DIRECTIONS
Spherical vs Non-Spherical (Ellipsoid) Humeral Heads
The optimal shape of the humeral head to use for stemless prostheses is an area of active investigation. Although prior literature has described the shape of the native humeral head to be more elliptical than spherical, most commercially available humeral head prostheses are spherical rather than ellipsoid (Wataru et al. 2005; Iannotti et al. 1992; Hertel, Knothe, and Ballmer 2002). However, recent research has shown good clinical and biomechanical outcomes and using ellipsoid humeral heads, with some studies showing ellipsoid heads produce better anatomic restoration and joint kinematics than spherical heads (Goldberg et al. 2018; Jun et al. 2013; Goldberg et al. 2021; Iannotti et al. 2019; Cavinatto et al. 2021; Lazarus et al. 2018; Humphrey and Gale 2018). A recent study by Cavinatto et al analyzed post-operative radiographs of 117 patients and assessed the anatomic reconstruction of three different implants (stemmed spherical, stemless spherical, and stemless elliptical) (Cavinatto et al. 2021). The authors found that the stemless elliptical implant achieved the best anatomic restoration of the three implants after looking at restoration of humeral head height, percentage of prosthesis overhang, and a compound anatomic reconstruction score (Cavinatto et al. 2021). Goldberg et al recently looked at clinical outcomes using an ellipsoid stem-free humeral prosthesis in sixty-three shoulders with a minimum 2-year follow-up (Goldberg et al. 2021). The authors found statistically significant improvements in range of motion (forward elevation, external rotation, internal rotation), American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form (ASES) score, and Patient-Reported Outcomes Measurement Information System (PROMIS) physical and mental function scores (Goldberg et al. 2021). Large randomized controlled trials are needed to continue to evaluate elliptical versus spherical humeral heads for stemless implants to provide more robust evidence.
Bone Preservation
Use of stemless humeral heads compared to stemmed prostheses significantly reduces bone loss and preserves much of the native bone stock. Minimizing bone loss during humeral head resection can improve implant fixation by allowing it to fix to high-density bone, and it allows for more bone stock to be available if a revision surgery is needed (Baranek et al. 2019; Alidousti et al. 2017). However, many surgeons use a freehand osteotomy for humeral head resection during TSA, often leading to more than necessary proximal bone loss. Alternative methods for humeral head resection that minimize bone loss while maximizing implant fixation may be beneficial. A recent system developed by Dr. Steven Goldberg creates multiplanar cuts for the humeral head using cutting guides to match the prosthetic implant thickness to the thickness of the bone resected (Goldberg et al. 2018, 2021; Baranek et al. 2019). This multiplanar osteotomy system has now been validated in a cadaveric study, radiographic study, and clinical study, showing high accuracy and reliability for anatomic reconstruction of the humeral head (Goldberg et al. 2018, 2021; Baranek et al. 2019). Further studies evaluating the multiplanar osteotomy system in larger patient populations are needed while more research developing other novel systems to improve implant fixation and minimize bone loss is also necessary.
Data for Long-Term Outcomes
Moving forward, robust randomized control trials (RCTs) and large prospective studies looking at long-term (15+ years) clinical and functional outcomes using stemless humeral implants are needed. Most current literature on stemless humeral implants reports short-term or mid-term outcomes (Berth and Pap 2013a; Uschok et al. 2017; Spranz et al. 2017; Beck et al. 2018; Maier et al. 2015; Churchill et al. 2016; Hawi et al. 2017; McMillan et al. 2021). However, one recent study by Magosch et al examined outcomes at more than 10 years follow-up, showing comparable results to those of standard stemmed implants (Magosch, Lichtenberg, and Habermeyer 2021). The authors found significant improvements in pain, activities of daily living, range of motion, and strength from pre-operatively to post-operatively (Magosch, Lichtenberg, and Habermeyer 2021). Additionally, Kaplan-Meier analysis revealed a 10-year survivorship rate of 96.5% for the stemless implants, although their study was limited by only including 75 patients (Magosch, Lichtenberg, and Habermeyer 2021). Another small study by Hawi et al evaluated stemless humeral implants 9 years after surgery in 49 patients and also found significant improvements in flexion, abduction, and external rotation without clinically significant radiologic abnormalities similar to standard stemmed humeral implants (Hawi et al. 2017).
CONCLUSION
The future for stemless humeral implants for anatomic TSA is promising. There are many advantages of stemless implants including decreased blood loss, reduced stress shielding, and preservation of bone stock. Future studies examining the optimal shape of the humeral head for these implants are needed as well as more long-term clinical data looking at patient outcomes using stemless implants. With robust RCTs and many other studies underway, the use of stemless implants is likely to only increase. Shoulder surgeons should be aware of the ongoing advancements in stemless humeral implants to optimize patient care.


.jpeg)

.jpeg)

.jpeg)

.jpeg)