This is the first of four award-winning presentations from the inaugural Medical School Orthopedic Society (MSOS) symposium. MSOS is a medical student-run initiative with a mission to support “research and educational opportunities for students interested in orthopedic surgery.”
This presentation was given by Rachel Joujon-Roche, a fourth-year medical student at Zucker School of Medicine and a research fellow under the guidance of spine surgeon, Dr. Peter Passias.
Surgical correction of adult spinal deformity (ASD) is associated with a relatively high rate of post-operative complications and revisions. At the same time, non-operative alternatives have not shown to be particularly effective in improving quality of life for ASD patients.

In this context, this study aimed to compare deformity and health relative quality of life (HRQoL) metrics in patients with suboptimal surgical outcomes to those undergoing non-operative management, which presumably approximates the natural history of ASD.
Based on clinical experience, we hypothesized that despite suboptimal outcomes, operative patients would demonstrate greater improvement in HRQLs and deformity when compared to the natural history of disease.

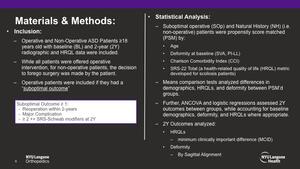
This is a retrospective analysis of patients prospectively enrolled in a single-center ASD database. All database patients were ≥ 18 years old and met at least one of the following radiographic requirements: Pelvic Tilt (PT) > 25°, Cobb angle > 20°, Sagittal Vertical Axis (SVA) >5cm or Thoracic kyphosis (TK) >60°.

Operative and Non-Operative ASD Patients ≥18 years old with baseline (BL) and 2-year (2Y) radiographic and HRQL data were included. While all patients were offered operative intervention, for non-operative patients, the decision to forego surgery was made by the patient. Operative patients were included if they had a “suboptimal outcome,” which was defined as reoperation within 2-years, any major complication, or presence of ≥ 2 severe (++) SRS-Schwab modifiers at follow-up.
Suboptimal operative (SOp) and Natural History (NH) patients were propensity score matched (PSM) by baseline age, deformity, Charlson Comorbidity Index (CCI) and SRS-22 Total. Means comparison tests analyzed differences in demographics, HRQLs, and deformity between PSM’d groups. Further, ANCOVA and logistic regressions assessed 2Y HRQL and deformity outcomes between groups, while accounting for baseline demographics, deformity, and HRQLs where appropriate.
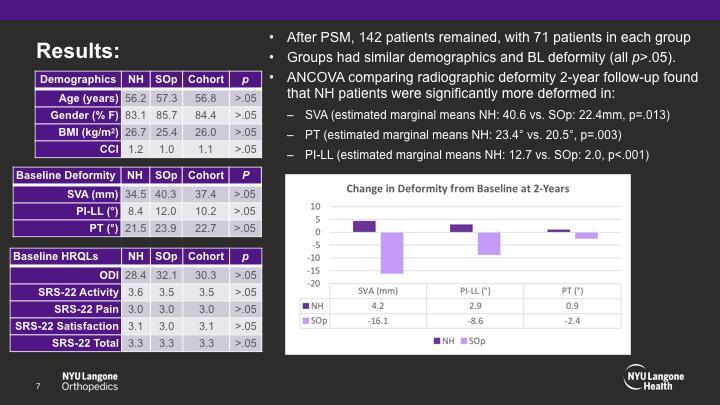
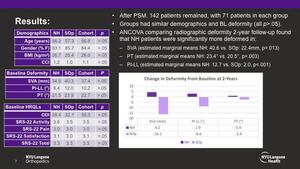
After PSM, 142 patients remained, with 71 patients in each group. Groups had similar age, gender, BMI, CCI, and baseline deformity (all p>.05). ANCOVA comparing radiographic deformity 2-year follow-up found that NH patients were significantly more deformed in SVA (NH: 40.6 vs. SOp: 22.4mm, p=.013), PT (NH: 23.4° vs. 20.5°, p=.003), and PI-LL (NH: 12.7 vs. SOp: 2.0, p<.001).

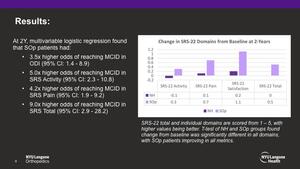
Further, multivariable logistic regression found that SOp patients had 3.5x higher odds of reaching minimum clinically important difference (MCID) in ODI (95% CI: 1.4 - 8.9), 5.0x higher odds of reaching MCID in SRS Activity (95% CI: 2.3 - 10.8), 4.2x higher odds of reaching MCID in SRS Pain (95% CI: 1.9 - 9.2), and 9.0x higher odds of reaching MCID in SRS Total (95% CI: 2.9 - 28.2).
Similar to previous findings, patients in the natural history group did not demonstrate improved quality of life outcomes at 2-year follow-up. Moreover, across HRQL metrics studied, suboptimal operative patients had 3.5x – 9.0x higher odds of achieving MCID. Furthermore, despite including severe SRS-Schwab modifiers at 2-years in the definition of suboptimal outcomes, ANCOVA found that SOp patients were significantly less deformed in all sagittal deformity measures compared to those in the natural history group.
Compared to the natural history of ASD, operative patients with suboptimal outcomes still experience significantly greater improvements in HRQLs postoperatively. Such divergent outcomes at 2Y highlight the stagnation and deterioration in outcomes associated with the natural history of ASD. Spine surgeons and patients should consider the outcomes associated with the non-operative course when weighing risks and benefits of operative intervention.
The other authors reported nothing to disclose.