Introduction
Total knee arthroplasty (TKA) performed for valgus knee arthritis accounts for 10-15% of all TKAs performed annually (Nikolopoulos et al. 2015). The senior author, who has performed arthroplasty for over 35 years, noted that patients with valgus deformity and arthritis often complain about instability and giving way more than pain. Valgus knees can present a technical challenge to the arthroplasty surgeon, as the pathoanatomy often involves both bony deformity and soft tissue abnormalities (Lange and Haas 2017). Bony deformity in valgus knees is generally related to lateral femoral condyle deficiency (especially the posterolateral femoral condyle), which can lead to external rotation deformity of the tibia. In addition, or independently, there may be a defect of the lateral tibial plateau, especially in the case of posttraumatic knee osteoarthritis (OA) (Long and Scuderi 2009). In TKA, these abnormalities can be addressed during bony preparation of the femur and tibia (Lombardi et al. 2004). However, even when accounting for the bony abnormalities of valgus knees, some patients will still require soft tissue releases to achieve appropriate flexion and extension gap balancing (Whiteside 1999). While multiple authors have described a stepwise approach to soft tissue balancing in the valgus knee (Whiteside 1999; Krackow and Mihalko 1999; Elkus et al. 2004), it can be difficult to both quantify and achieve appropriate ligament balance using conventional methods. Failure to correctly balance the soft issues in valgus knees can lead to high rates of postoperative instability and lower patient satisfaction (Babazadeh 2009).
Robotic assisted surgery (RAS) with Navigation (Nav) has been proposed as a solution to improve component positioning and soft tissue balancing in TKA (Plaskos et al. 2021). Prior literature has demonstrated that robotic-assisted TKA (RAS-TKA) has been able to reduce alignment outliers and improve gap balance postoperatively as compared to conventional TKA (Song et al. 2013). Despite the improved component alignment and balancing of flexion and extension gaps, this has often failed to correlate with improvements in patient-reported outcome measures (PROMs) and satisfaction as compared to conventional TKA (Cho et al. 2019; Kim, Yoon, and Park 2020; Yang et al. 2017). Certain RAS and Nav systems use pressure sensor technology to evaluate medial and lateral gaps at static points throughout the arc of motion (generally full extension, 45 degrees of flexion, and 90 degrees of flexion) (Golladay et al. 2019). More recently, systems have been developed that allow for the measurement of medial and lateral gaps dynamically and continuously throughout the entire range of motion of the knee during TKA (Siddiqi et al. 2020). One such system is the BalanceBot device (Corin USA, Raynham, MA). Preliminary studies using this technology have demonstrated improved final balancing and patient outcomes in TKA (Keggi et al. 2021).
Here, we report a case of a patient undergoing primary TKA for severe post traumatic osteoarthritis with significant preoperative valgus deformity of the knee that was unable to be corrected and balanced solely with bony cuts. The use of a modern FDA-approved robotics system (OMNIBotics Robotic Total Knee Replacement System (Corin USA, Raynham, MA)) in conjunction with the BalanceBot, allowed us to determine the degree of residual soft tissue tightness following bone preparation and perform a series of titrated soft tissue releases. This resulted in correction of the patient’s deformity, which was verified and validated in real time prior to implantation of the final components. We also present data obtained by the OMNIBot in another case in which there was residual tightness laterally in flexion after bony cuts. This tightness also resolved after appropriate soft tissue releases.
Case Report
Clinical Presentation
The patient was a 67-year-old male who presented to the orthopaedic clinic in November 2021 with a chief complaint of left knee pain and deformity that had lasted for several years. The patient had a history of multiple injuries to the left lower extremity. Many years prior to presentation, the patient sustained a fracture of the distal femur that was treated with open reduction and cast immobilization. He subsequently went on to require arthroscopic intervention of the left knee for “scar tissue.” He later sustained a fracture about the left knee that was treated closed. He furthermore sustained an impacted fracture of the left proximal femur that was treated with two cannulated screws. These screws were later removed.
Physical examination of the left knee demonstrated a well-healed 30-35 cm incision over the lateral aspect of the knee and an obvious valgus deformity (Figure 1). Range of motion was from 5 degrees short of full extension to 105 degrees of flexion with pain and crepitus throughout the entire range of motion. Ligamentous testing demonstrated 1+ varus/valgus instability with no anterior/posterior instability. The patient was neurovascularly intact throughout the extremity.
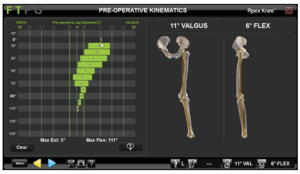
Radiographs of the left knee demonstrated Kellgren-Lawrence grade 4 changes of the knee, which were the worst in the lateral compartment with significant involvement of the medial and patellofemoral compartments as well (Figure 2). There was a 16.9-degree valgus deformity of the knee as measured on the anteroposterior (AP) radiograph.
The patient’s symptoms had not improved with multiple nonoperative modalities including activity modification, bracing, non-steroidal anti-inflammatory drugs, and corticosteroid injections. The patient was scheduled for a left robotic-assisted total knee arthroplasty with OMNIBotics and the BalanceBot System. An extensive discussion regarding the risk of peroneal nerve palsy given his valgus deformity and mild flexion contracture was carried out with the patient, and he verbalized his understanding of this risk.
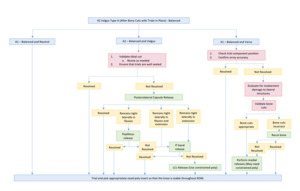
Exposure and Robot Registration
The patient was taken to the operating room (OR) electively, and a standard medial parapatellar approach to the knee was utilized. Exposure included a limited 2 cm soft tissue sleeve circumferential medial release, resection of the anterior cruciate ligament and posterior cruciate ligament and meniscal remnants, as well as removal of osteophytes from the femur, tibia, and patella. Two pins were placed in both the femur and tibia, respectively, and tracking arrays were securely fastened for the OMNIBot. Registration of the landmarks utilized by the OMNIBot was performed as previously described (Blum et al. 2021). A detailed video demonstrating the technique for using the OMNIBot system in conjunction with the BalanceBot device can be found online (https://vimeo.com/321724524). Following landmark registration, the left lower extremity was taken through a range of motion from the fullest extension that could be achieved to approximately 110 degrees of flexion and repeated with varus and valgus stress applied to the knee. The OMNIBot recorded the knee alignment and medial and lateral gaps throughout the range of motion, yielding the graph in Figure 3. During this step, the patella was kept reduced to ensure that all structures providing lateral restraint were accounted for. Regarding this patient, the graph demonstrated a 5-degree flexion contracture and valgus alignment in extension that did not correct with application of a varus force with a gradual improvement to neutral alignment in flexion.
Tibia-First Gap Balancing
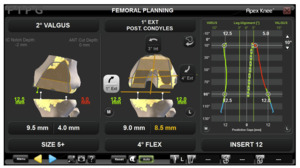
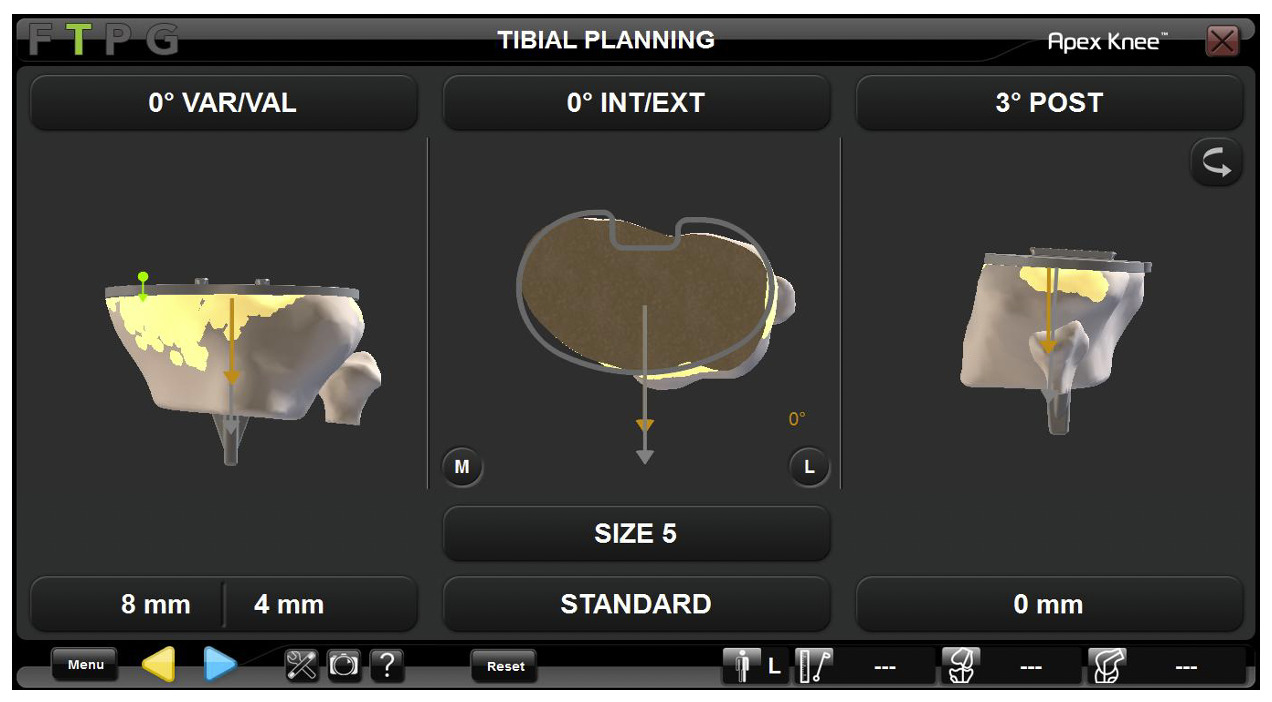
Based on the above kinematic graph, the following tibial cut plan was developed by the OmniBot software (Figure 4). The senior author (JK) generally plans for a cut orthogonal to the tibial mechanical axis (i.e., 0 degrees varus/valgus) for valgus knees with 3 degrees of posterior slope if the patient does not appear to have excessive posterior slope on lateral radiographs (as in this patient), which is represented on the tibial cut plan. The software also provides an estimate for the size of the tibial component that corresponds to the Corin Apex tibial component sizing.
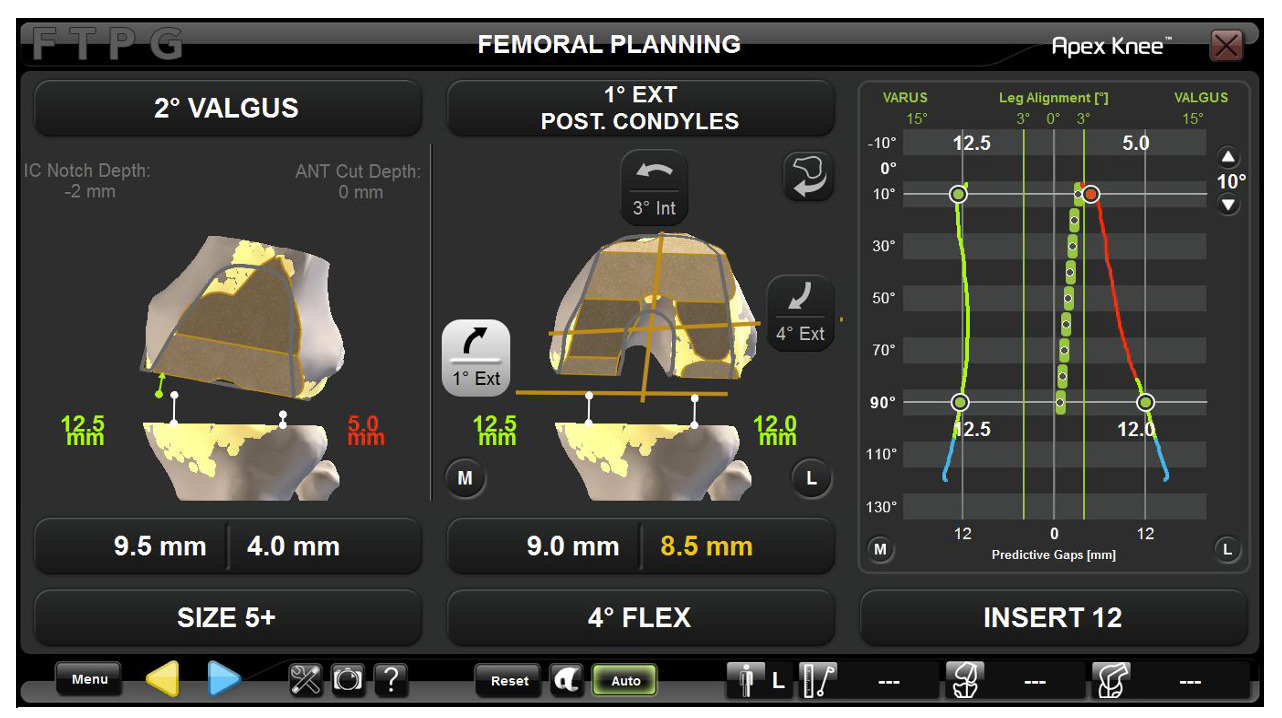
After the tibial cut was performed and validated and any remaining soft tissue in the joint (i.e., meniscus, fat pad, scar tissue, etc.) was resected, the BalanceBot was introduced into the knee joint, and another graph of the medial and lateral graphs throughout knee range of motion was obtained. To do this, the knee was first manually and repeatedly taken through a range of motion between 70-110 degrees of flexion while slowly increasing the force applied by the BalanceBot until the point that defines the toe of the ligament stress-strain curve was reached. The force required to reach this toe point was then recorded. This was repeated between 0 and 30 degrees of flexion, and again, the force required to reach the toe point in extension/near-extension was recorded. Finally, the knee was taken through a full range of motion with the previously recorded forces applied at their corresponding levels of flexion to produce the graph and femoral cut plan shown in Figure 5. Additional adjustments were made to the femoral bony cut plan in order to balance the medial and lateral flexion gaps and the medial extension gap. Afterward, significant tightness of the lateral extension gap remained. At this point, it was determined that the extension gap could not be easily balanced based solely on virtual bony cuts, so we proceeded with preparation of the femur. A brief video providing an overview of balance targets and how they are used in TKA with the OMNIBot and BalanceBot system can be found online (https://vimeo.com/526154820/9e4a319201)
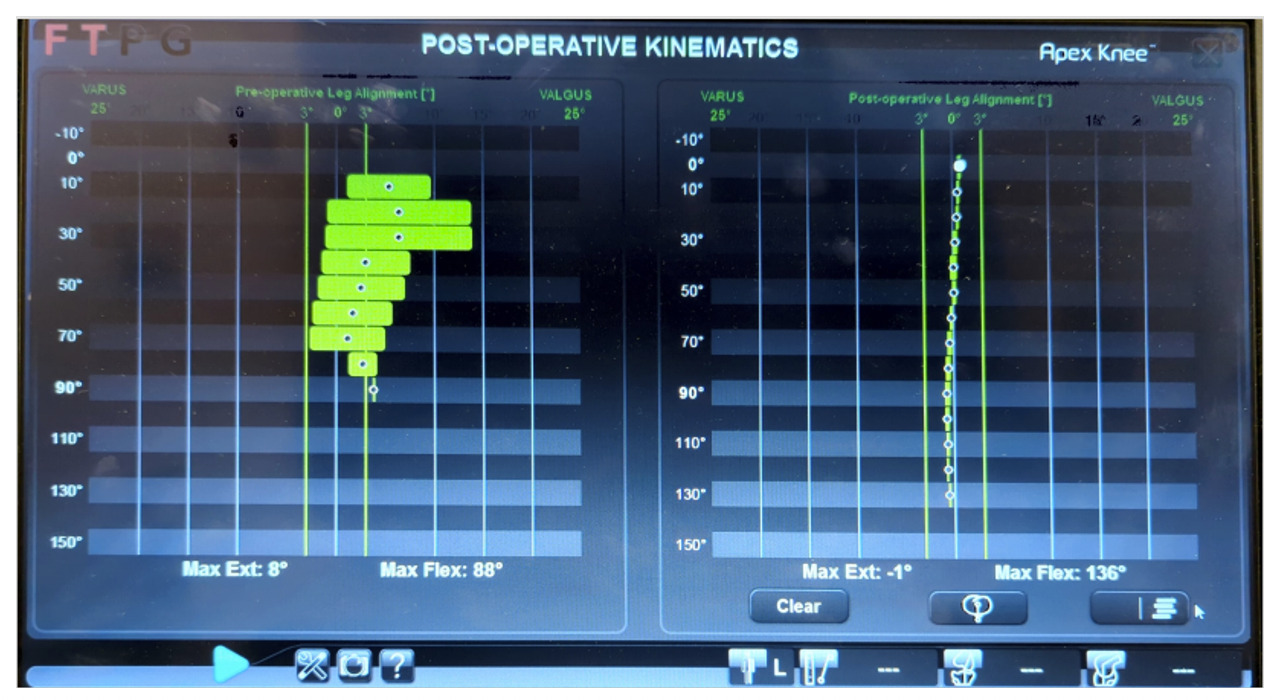
Soft Tissue Release
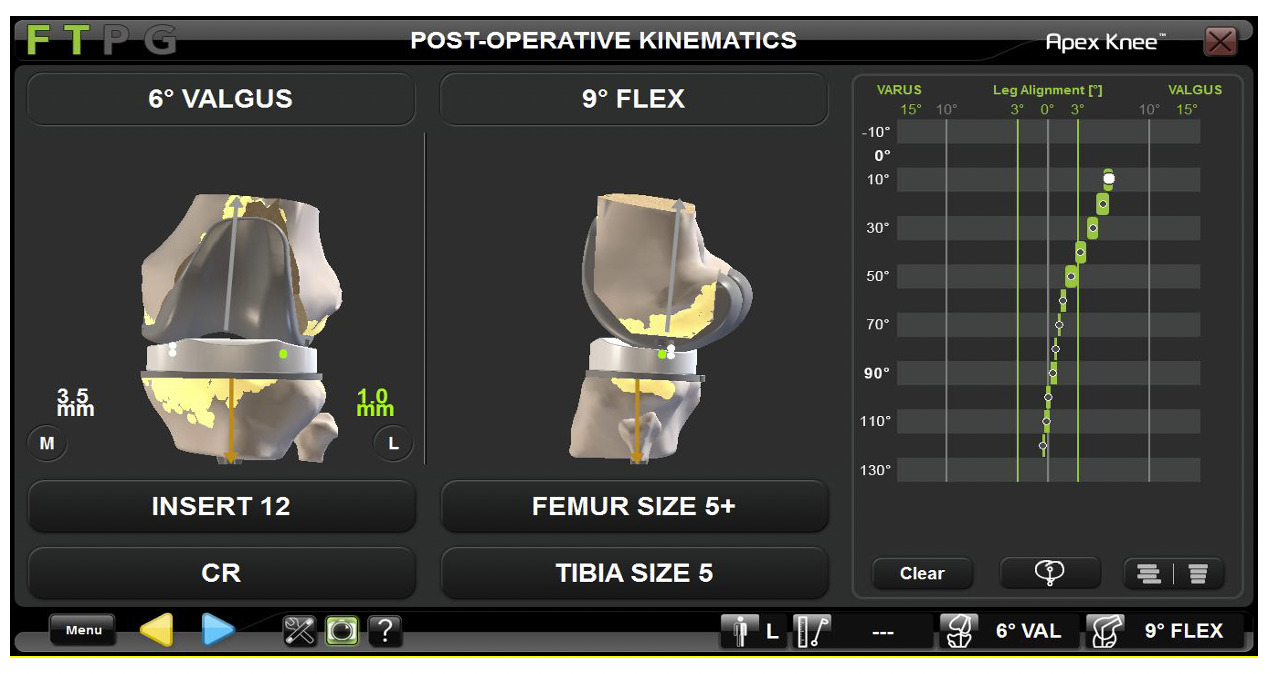
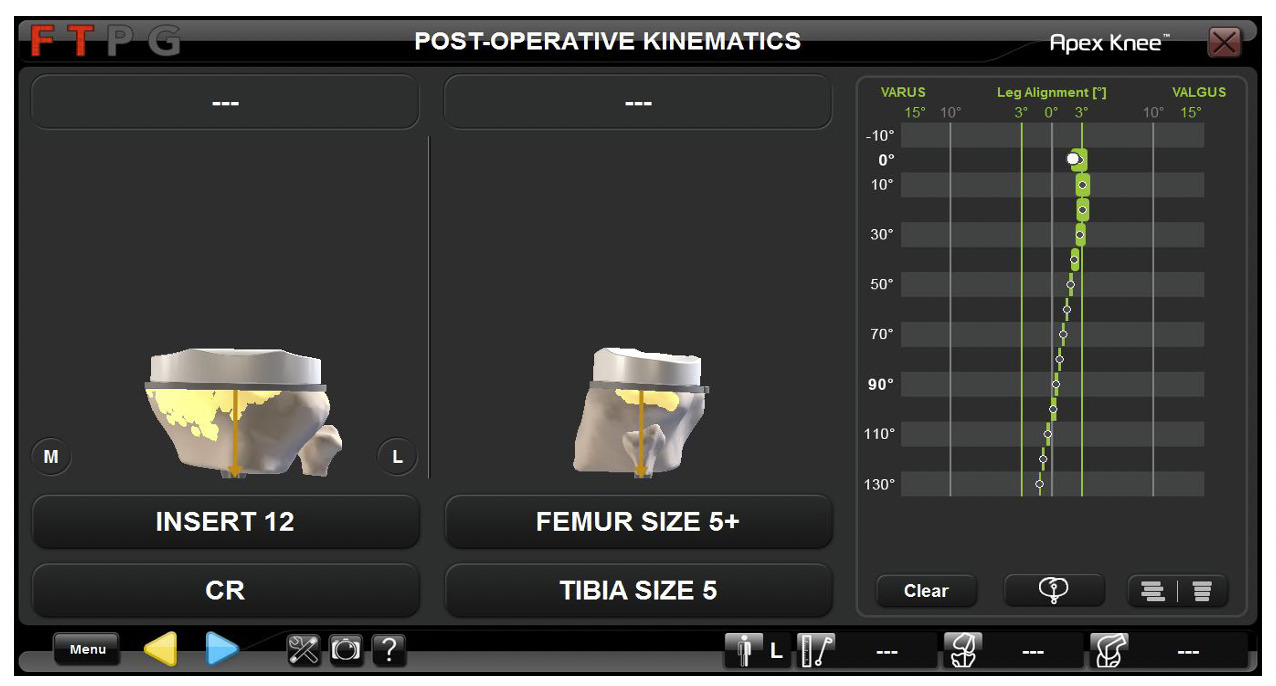
After preparation of the femur was completed and posterior osteophytes were removed, trial components were placed, and the knee was again taken through a range of motion. The graph shown in Figure 6 was recorded by the OMNIBot and demonstrated continued lateral tightness of the joint in extension with gradual correction of alignment with flexion of the knee. Given these findings, a release of the posterolateral capsule (PLC) and iliotibial (IT) band was performed as previously described by Ranawat et al. (Ranawat et al. 2005), and Elkus et al (Elkus et al. 2004). Following this soft tissue release, the knee was taken through a range of motion with trial components in place, and the graph shown in Figure 6 was obtained showing resolution of the valgus deformity to within 3 degrees of neutral. Final implants were then placed, and the final kinematic graph compared to the initial kinematic graph obtained (prior to bony cuts) showed resolution of the patient’s valgus deformity to within the acceptable alignment range, indicating excellent gap balance (Figure 8).
At six weeks postoperatively, he was progressing well with therapy with minimal discomfort in the knee. Physical examination showed a well-healed incision and resolution of the preoperative deformity (Figure 9). Range of motion of the knee was from full extension to 135 degrees of flexion (Video 1), and the knee was stable to varus/valgus and anterior/posterior stress. X-rays of the knee demonstrated a well-positioned, well-aligned left total knee arthroplasty with no acute abnormalities (Figure 10).
As a supplement to the above case, we also present the kinematic graph obtained from two additional patients with valgus osteoarthritis of the knee. The first kinematic graph (Figure 11) was obtained from a patient after bony preparation and with trial implants in place. In this case, as can be seen in Figure 11, there was residual tightness laterally which could be corrected to neutral in extension but not in flexion, suggesting tightness of the popliteus. To address this, selective release of the popliteus tendon, as described by Whiteside (Whiteside 1999), was performed. This resulted in resolution of the lateral tightness in flexion and neutral alignment throughout the range of motion as demonstrated in Figure 12.
Additionally, Figure 13 is an example of a patient with a 15-degree preoperative valgus deformity. The figure demonstrates the kinematic graph obtained after exposure and prior to any bony cuts (left) and the final kinematic graph obtained after final implantation (right) demonstrating excellent alignment and balance throughout. Appropriate alignment and “predictive” soft tissue balance were able to be achieved with bony cuts alone in this case without any need for additional soft tissue releases.
Discussion
Valgus knees present a unique challenge for the arthroplasty surgeon as far as achieving appropriate alignment and soft tissue balancing throughout the full range of motion (Lange and Haas 2017; Long and Scuderi 2009). RAS with Nav has been proposed as a novel technology to help with component positioning and soft tissue balancing, and may be particularly useful in difficult cases such as these (Plaskos et al. 2021; Held et al. 2021). Here, we report the case of a patient with significant preoperative valgus deformity in the context of posttraumatic arthritis. The patient demonstrated residual lateral tightness in extension following all bony cuts indicating that appropriate balancing of the knee was unable to be achieved by bony cuts alone.
Achieving appropriate soft tissue balance and correcting preoperative deformity is significantly more difficult in valgus knees as compared to varus knees, often requiring additional soft tissue releases (Mullaji et al. 2021). This finding has been corroborated in the senior author’s own patient population. In a cohort of 330 knees, including 38 knees with preoperative valgus deformity (11%), there was a trend (p=0.074) toward higher rates of soft tissue release in valgus knees (25%) as compared to varus (15%) and neutral (8%) knees (unpublished data). While there is only one patient who had a large preoperative valgus deformity (defined as >10 degrees MA), patients with a large preoperative varus deformity (29%) were more likely (p=0.007) to require a soft tissue release than those with a preoperative varus deformity <10 degrees (12%). With the limited numbers available, there was a trend (p=0.44) toward decreased patient satisfaction rates in patients who required a soft tissue release (89%) as compared to those that do not require a soft tissue release (97%) as measured by the new Knee Society Scoring System (Culliton et al. 2018). This is consistent with another study performed by the senior author which showed decreased rates of patient satisfaction in patients requiring a soft tissue release as compared to those patients in which appropriate balance was obtained using just bony cuts (Vigdorchik et al. 2022). Therefore, it is important to minimize the extent of the soft tissue release performed, and thus only release what is necessary to achieve balance. The OmniBot allows for an easy and reproducible evaluation of the gap balances in real time to allow the surgeon to determine the minimal extent of releases necessary for appropriate balancing.
Multiple authors have described a stepwise approach to soft tissue release that can be used to address residual tightness and laxity following bony cuts in the valgus knee (Ranawat et al. 2005; Whiteside 2018; Peters, Mohr, and Bachus 2001). The structures on the lateral aspect of the knee can be released preferentially depending on what point during the range of motion that the knee remains unbalanced. In knees that are well-balanced in extension but are tight laterally in flexion and often with associated external rotation contracture of the knee, the popliteus is released partially or completely from its insertion on the femur. If there is residual lateral tightness following release of the popliteus, the lateral collateral ligament can then be released.
In knees that are well-balanced in flexion but tight laterally in extension, soft tissue release should begin with the IT band. Whiteside describes a subcutaneous “outside-in” approach to release of the IT band; however, the IT band can also be released intra-articularly with an “inside-out” approach. If the knee remains tight in extension following release of the IT band, the posterolateral capsule (PLC) should be released next. Release of the PLC can also be performed using a pie-crusting technique. This is generally sufficient to result in resolution of the lateral tightness in extension. In rare cases where there is residual tightness, release of the LCL can be considered.
Different approaches have been described for the knee that is tight laterally in both flexion and extension. Whiteside favors release of the LCL first in these knees followed by release of the popliteus if there is residual lateral tightness, and he has achieved excellent long-term results using this technique (Whiteside 2018). Peters et al. evaluated the effect of progressive release of lateral soft tissues in cadaveric knees and found that release of the posterolateral capsule followed by the IT band and then the popliteus affects the lateral flexion and extension gaps more symmetrically than previously described techniques (Peters et al. 2013). We thus follow a similar sequence in the knee that is tight laterally in both flexion and extension.
While traditionally appropriate soft tissue balance has been determined by a surgeon’s “feel” intraoperatively, the advent of RAS with Nav has allowed for a more robust and reproducible method of assessing tightness and laxity in the knee. For this case study, the precise amount of tightness and its location throughout the range of motion of the knee was able to be quantified using the BalanceBot system. As demonstrated in Figure 6, the knee was tight only in extension and was appropriately balanced in flexion. We therefore knew that we needed to address the tightness in extension through release of the IT band and possibly the posterolateral capsule. As we progressively released first the IT band followed by the posterolateral capsule, we were able to use the BalanceBot system to determine exactly when we had performed a sufficient soft tissue release to resolve the lateral tightness. This prevented us from performing an overly aggressive soft tissue release leading to lateral laxity. The use of Nav thus allowed for a titrated release of the lateral soft tissue structures, and the resultant improvement in lateral tightness in extension was able to be confirmed using the BalanceBot system. This titrated soft tissue release, along with modern postoperative total knee protocols, could be responsible for patient’s lack of discomfort and excellent range of motion and stability as early as six weeks post-op.
Valgus knees pose other challenges beyond achieving appropriate soft tissue balance. Common peroneal palsy occurs more frequently in patients undergoing TKA with preoperative valgus deformity, occurring in 1.9% of cases, and is thought to be related to excessive lateral soft tissue release and overcorrection of the patient’s preoperative deformity (Puijk et al. 2022). It is important to perform only the minimum soft tissue release necessary to achieve appropriate balance to help prevent peroneal nerve palsy due to the proximity of the common peroneal nerve to the lateral soft tissue structures in the knee (Clarke et al. 2004; Bruzzone et al. 2010). Use of the BalanceBot allowed us to confirm that we had performed enough of a release to resolve any residual tightness without performing an excessive release or overcorrecting the patient’s preoperative deformity, as such a peroneal nerve palsy was avoided in this patient. Future research could examine the role of RAS in possibly minimizing the risk of peroneal nerve palsy in patients with severe preoperative deformity. In addition, this patient’s degree of preoperative deformity placed him at higher risk for requiring constraint to achieve appropriate balance (Goltzer et al. 2017). This was not the case in our patient as we were able to achieve appropriate balancing throughout flexion and extension simply using a cruciate-substituting, ultracongruent polyethylene insert.
While studies have shown mixed results regarding improvements in functional outcomes using RAS-TKA (Plaskos et al. 2021), recent work has shown that improvements in postoperative gap balancing led to significant improvements in PROMs (Keggi et al. 2021; Petursson et al. 2018). Further studies are needed to determine optimal balance targets, including patient-specific balance targets, which may ultimately lead to improved functional outcomes. This case, as well as the similar case presented above of a patient who was tight laterally in flexion alone, demonstrates how modern technology, including a predictive joint tensioning tool, and RAS can be used to identify areas of lateral and medial imbalance throughout the range of motion and confirm when this has resolved after minimal appropriate soft tissue releases.
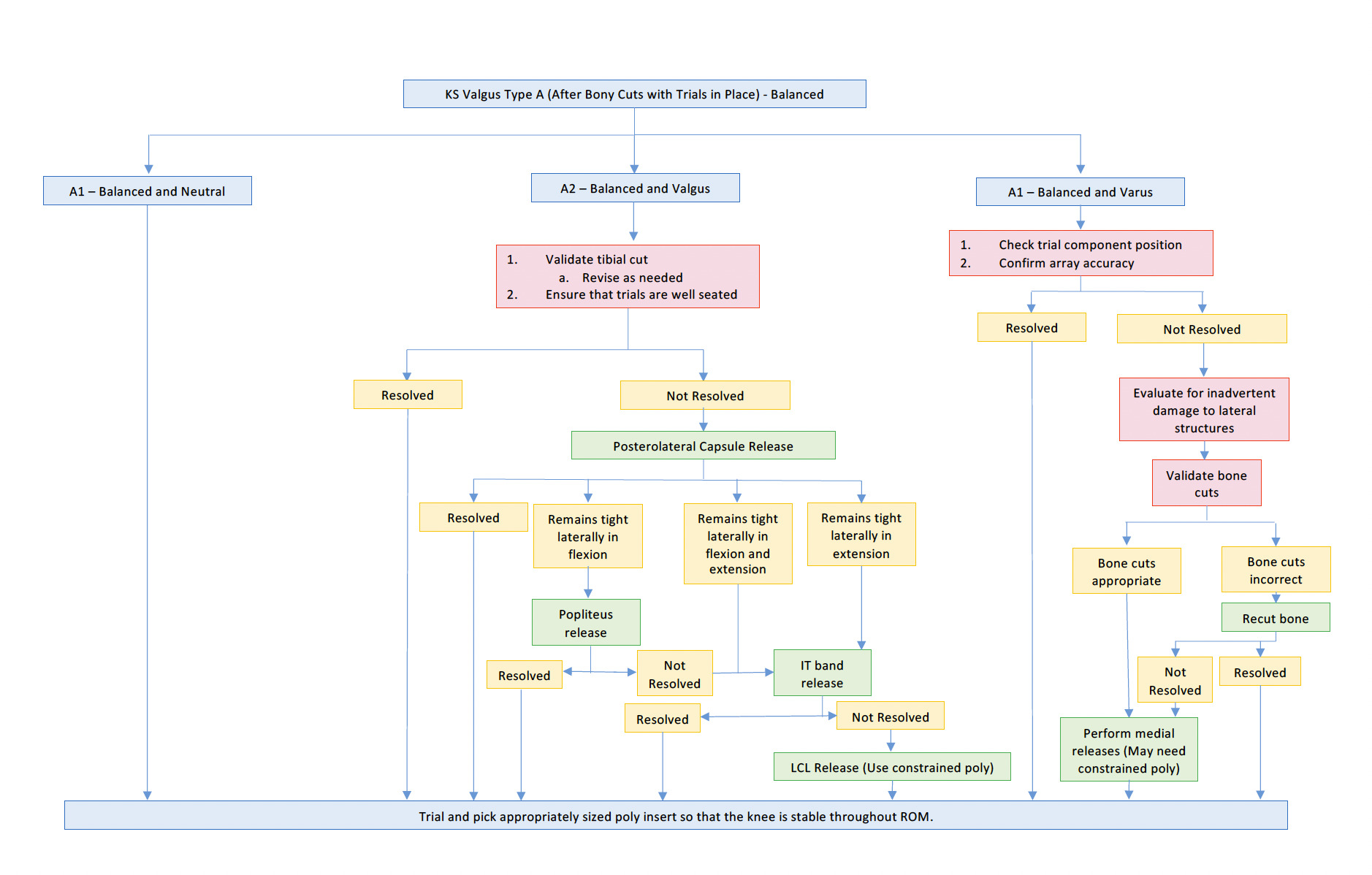
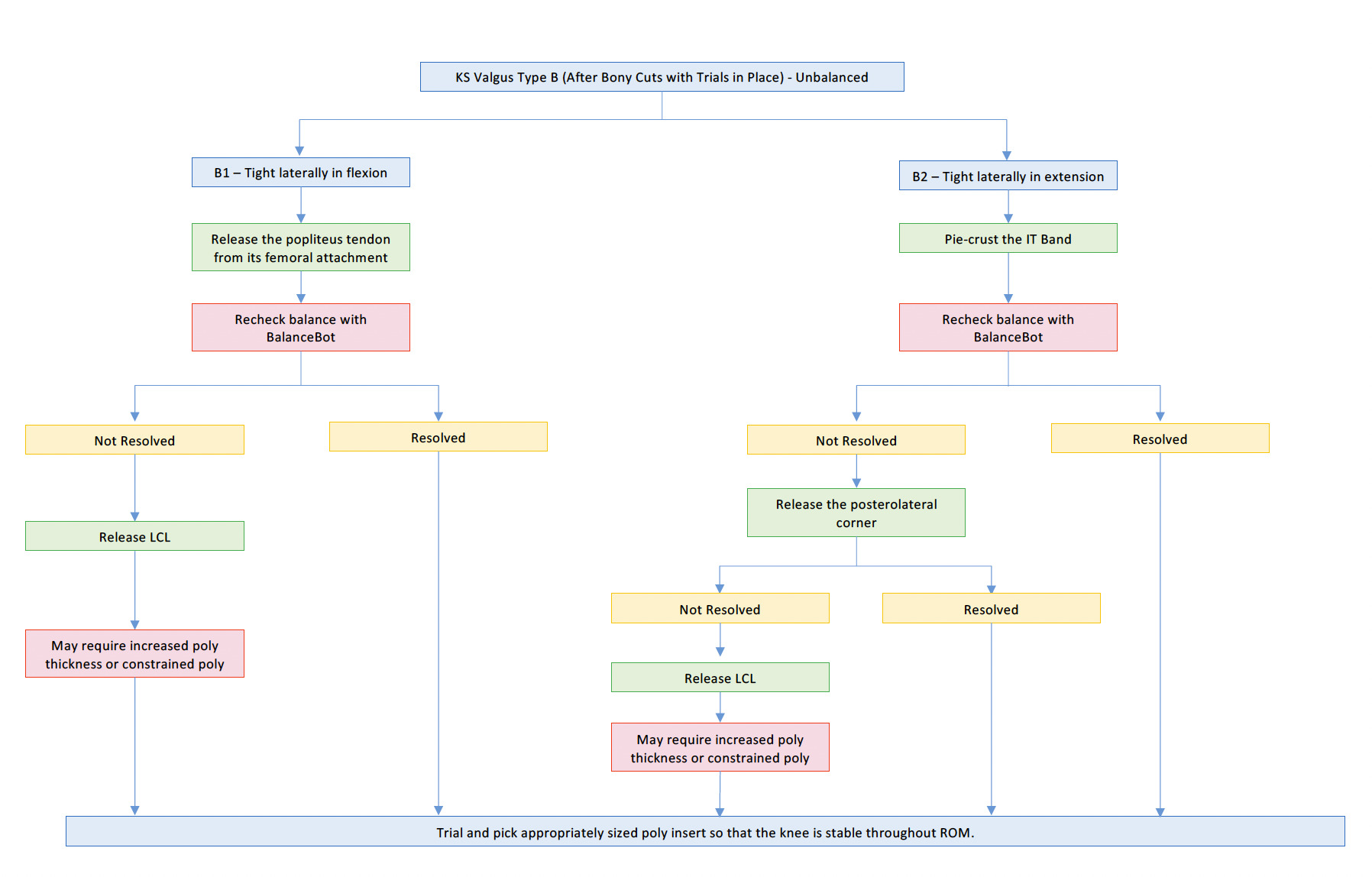
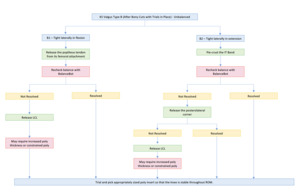
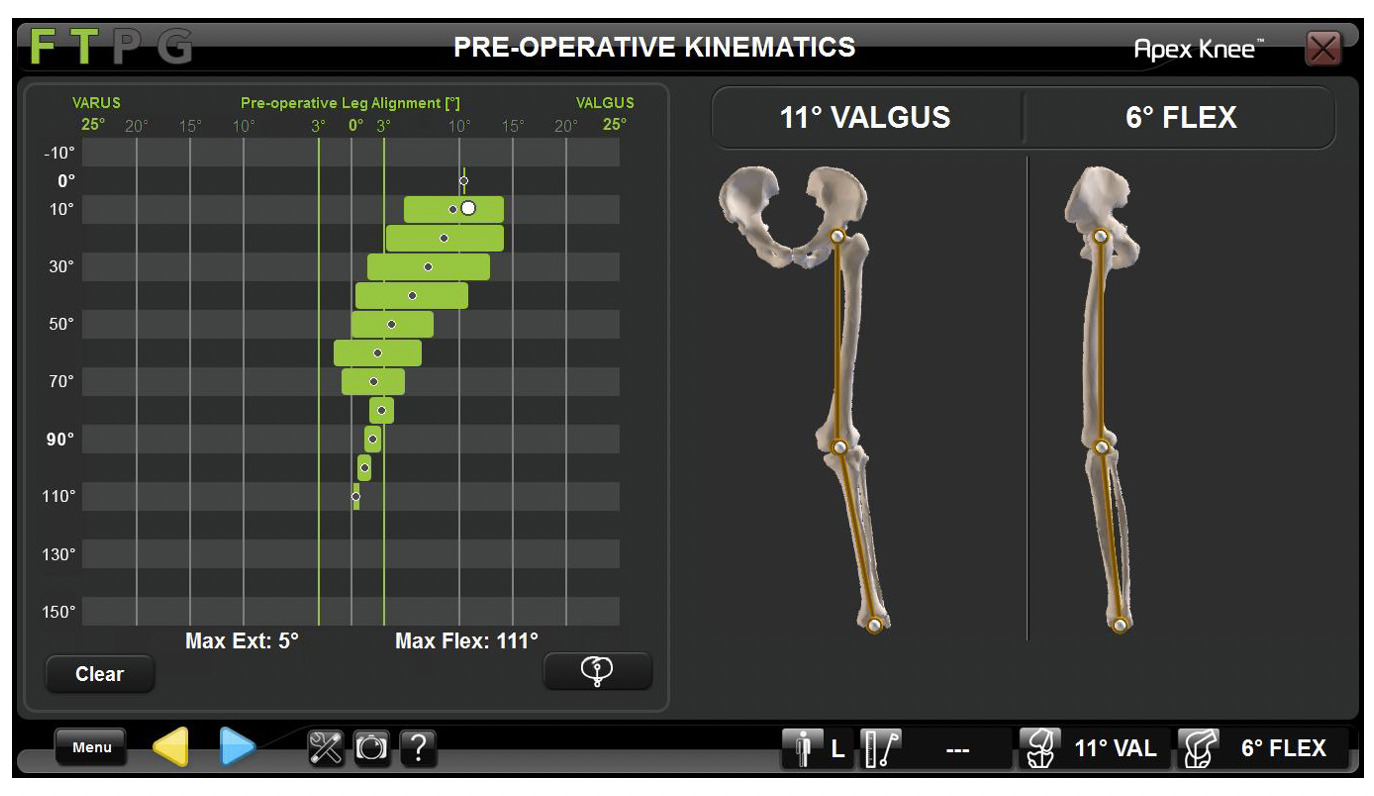
We propose the following simple algorithmic Koenig Scanlon Classification System to help arthroplasty surgeons successfully correct both the alignment and instability of arthritic knees with valgus deformity using OMNIBotics (Figures 14 and 15). Of note, this classification scheme should be employed after bony cuts have been made and with appropriate trials in place. The graph generated by the OMNIBot with the trials in place can then be used to determine how the knee should be classified. Bony cuts should be used to attain balance, if possible, as discussed above. This is achieved with the help of the OMNIBot and predictive planning prior to bony cuts. This classification scheme can then be used to help identify if further action is necessary to balance the knee.
In addition, in the case of a knee that is classified as A2, A3, B1, or B2, it is important to first validate the distal femur and tibial cuts prior to proceeding with any soft tissue releases. If validation demonstrates significant deviations from the planned cuts, then those cuts should be revised. In addition, mild residual tightness can occasionally be addressed with minor revisions to the bony cuts of the tibia or distal femur (in cases of imbalance in extension) via skim cuts of just the medial or lateral side. It is the senior author’s preference to perform a tibial cut perpendicular to the long axis of the tibia (i.e., 0 degrees of varus/valgus) for the valgus knee. However, one to two degrees of tibial valgus may be well tolerated to help reduce residual tightness in both flexion and extension. In addition, up to three degrees of valgus of the distal femur is acceptable to resolve residual lateral tightness in extension prior to soft tissue releases. Occasionally, this can be achieved with freehand skim cuts or planing of just the medial or lateral aspect of the tibia or distal femur using a saw to allow for very minor adjustments to help resolve residual tightness. However, it should be noted that this technique does not work for cases where there are large residual imbalances such as the ones presented here.
Koenig Scanlon Valgus TKA Classification System
-
KS Valgus Type A: Balanced
-
KS Valgus - A1: Balanced and neutral: Within 3 degrees of neutral throughout the entire range of motion.
-
Treatment:
-
No soft tissue releases necessary.
-
Trial and pick appropriately sized poly so the knee is stable throughout the range of motion.
-
-
-
KS Valgus - A2: Balanced and valgus: Greater than 3 degrees of valgus throughout the entire range of motion.
-
Treatment:
-
Recheck tibial cut using tracker to ensure that the cut was made and validated and registered appropriately. It is important to ensure that the tibia was not cut in varus in these cases prior to proceeding with soft tissue release, as this can lead to tightness laterally in both flexion and extension.
- If the tibial cut was not made appropriately, revise as needed and recheck.
-
Make sure trials are well seated.
-
If all is appropriate above may proceed with release of the posterolateral capsule limited.
-
If remains tight laterally throughout range of motion or in extension only, piecrust the IT band.
-
If tight only in flexion, release popliteus insertion at distal femur.
-
Recheck with BalanceBot after each step to prevent over-release of soft tissues.
- This is vital to help reduce the risk of common peroneal nerve palsy postoperatively.
-
If the knee remains tight laterally, proceed with LCL release via Leo Whiteside’s “Outside In” or Pie Crusting technique.
-
-
-
KS Valgus - A3: Balanced and Varus: Greater than 3 degrees of Varus throughout the entire range of motion. (Would be rare in valgus knees)
-
Treatment
-
Check trial component position and for array accuracy.
-
Evaluate for inadvertent damage to lateral structures.
-
If still not corrected, consider bony recuts if they were off or perform necessary medial releases after checking for and removing any residual medial osteophytes (i.e., deep medial collateral ligament release, posteromedial corner, etc.).
-
Recheck with BalanceBot to ensure neutral balance throughout. Choose appropriate poly so knee is stable throughout range of motion-may need constrained poly.
-
-
-
-
Type B: Unbalanced
-
KS Valgus - B1: Unbalanced, tight laterally in flexion: Within 3 degrees of neutral in extension but >3 degrees of valgus in flexion.
-
Treatment
-
Release the popliteus tendon from femoral attachment.
-
Recheck with BalanceBot to see if flexion tightness resolved.
-
If not, release LCL.
-
Trial and may require increase polyethylene thickness to balance.
-
-
-
KS Valgus - B2: Unbalanced, tight laterally in extension: Within 3 degrees of neutral in flexion, but >3 degrees of valgus in extension.
-
Treatment
-
Pie Crust the IT band.
-
Recheck with BalanceBot to see if extension tightness resolved.
-
If not, release the PLC. Trial and choose appropriate poly.
-
-
Conclusion
Valgus knees present a challenge to the arthroplasty surgeon in regard to achieving appropriate postoperative alignment and soft tissue balancing. The advent of RAS with Nav offers surgeons a potential solution to help prevent the need for soft tissue releases in valgus knees. When soft tissue releases are necessary after bony cuts have been completed, the ability to evaluate soft tissue balancing in real time using RAS and Nav allows the surgeon to perform a titrated soft tissue release of the necessary structures and accurately determine when an appropriate release has been performed. Our initial studies suggest that this improvement in soft tissue balancing, and alignment may result in improved PROMs postoperatively.
Acknowledgements
For their insights and collaboration over the years and for their validative review of our manuscript the authors wish to acknowledge:
Christopher Plaskos PhD
Edgar Wakelin PhD
John Keggi MD
Without their contributions this work would not have been possible.




__lateral__and_sunrise_view_x-rays_of_the_patients_left_.png)



_prior_to_any_bony_cuts__and_final_kinematic_graph_(right)_a.png)



_after_selective_popliteus_release_demon.png)





__lateral__and_sunrise_view_x-rays_of_the_patients_left_.png)
_prior_to_any_bony_cuts__and_final_kinematic_graph_(right)_a.png)



_after_selective_popliteus_release_demon.png)