Introduction
In recent years, blockchain has emerged as a foundational technology primed to change how our world functions. Bitcoin, Ethereum, and other forms of blockchain technology have been at the forefront of this discussion; however, it is blockchain, the technology that supports all these platforms, that merits our attention. While full implementation remains years to decades from realization, this article will define blockchain and discuss why orthopaedic surgeons and physicians should learn about blockchain along with future applications of this technology (Iansiti and Lakhani 2017).
To begin, what is blockchain? Part of understanding this technology is recognizing its challenges. It is a foundational technology, not a disruptive one, meaning its implementation is limited by the novelty and complexity of the technology. Examples of foundational technologies are the internet and electricity. These are transformative technologies that have been critical to the scaling of all industries including medicine. Once a technology achieves critical mass then further development and utility can be achieved (Iansiti and Lakhani 2017).
Understanding the technology and ease of use are key for adoption. While cryptocurrency has primed the blockchain conversation, there are multiple avenues for blockchain application from smart contracts, surgical billing, inventory management and supply chain, the QR codes used to pull up menus at restaurants or check in at airports, non-fungible tokens (NFTs), data storage, real-time disease tracking (Covid19 pandemic and vaccination), and health insurance claims. The value of blockchain is that anything and everything can have a unique identifier, be recorded, and tracked.
Blockchain has the ability to unlock future growth and value with unmet efficiency and transparency by providing the foundation to be a system of record for all transactions. The primary aim of this article is to highlight how this technology can be utilized to improve our understanding of surgical billing, supply chain in medical care, and to introduce smart contracts.
Blockchain basics
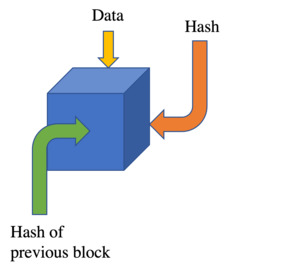
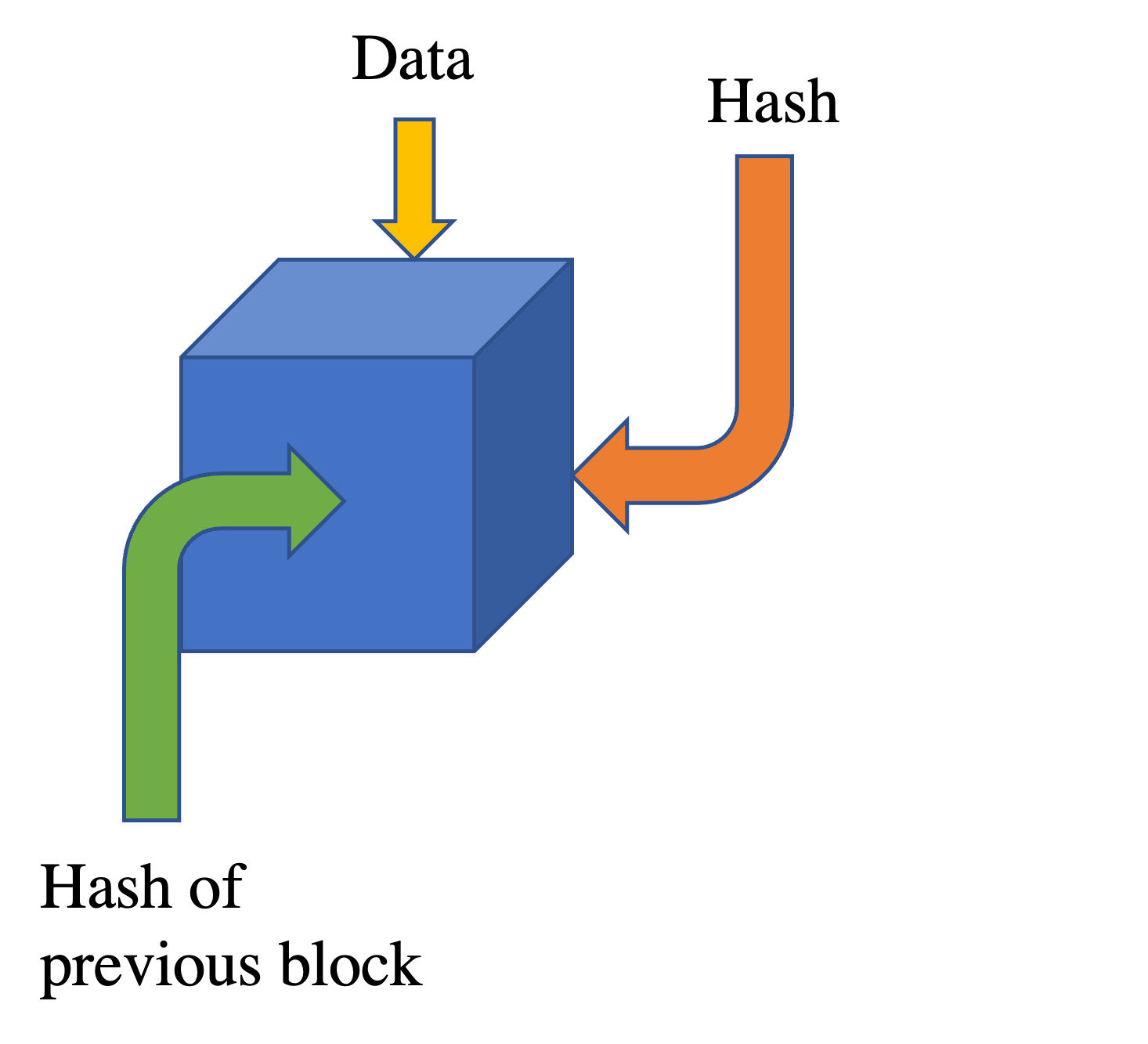
Broken down to its simplest form and definition, blockchain is an open distributable ledger that can efficiently, verifiably, permanently, and nearly instantaneously record transactions between two parties (Iansiti and Lakhani 2017). It represents an automated and secure record that cannot be altered. See Appendix for a more detailed explanation of how blockchain technology works to create this ledger.
To illustrate this, imagine you are hungry and wish to purchase some fruit. You enter the local grocery, pick up your fruit of choice, in your case a pear from Brazil. Like many other grocery products, this Brazilian pear has a sticker on it. This particular sticker is a QR code linked to a blockchain record. You take this Brazilian pear with its sticker to the counter, scan it, and purchase it with your digital wallet. Unfortunately, a few hours later after eating your pear, you develop food poisoning. Convinced and concerned for other pear consumers, you return to the store to report this. Because this pear with its scannable QR code is part of a blockchain network, you are able to collect the following reliably and instantaneously: the region of Brazil where and when this pear was picked, which parcel it was stored in, what was the temperature of storage, and its path from Brazilian farm to packaging to shipping to store to your grocery bag. Moreover, you are able to isolate this particular parcel of pears and locate where other possibly defective pears ended up (Figure 1).
Without blockchain technology, collecting this degree of granular detail would be impractically labor- and resource-intensive. Blockchain brings the promise of alleviating the administrative albatross required to navigate the healthcare system. Herein lies the untapped value of blockchain and why as physicians we should care.
Blockchain technologies have shown enormous promise in other sectors. The World Food Program, a humanitarian nonprofit organization delivering food assistance in emergences worldwide, has implemented blockchain with great success with one pilot program realizing a savings of $2.4 million USD alone in reduced transactions and administrative costs (“Building Blocks | WFP Innovation,” n.d.).
Healthcare and blockchain
For the most part, the healthcare system is amongst the largest industries in the United States economy, spending $4 trillion annually (Shrank, Rogstad, and Parekh 2019). Yet alarmingly, this industry is rife with inefficiency with some estimates up to 25% (or ~ $953 billion) annually in wasteful spending (Shrank, Rogstad, and Parekh 2019). Moreover, inefficiencies in supply chain operations can account for up to 50% of total operation costs (Alicke and Lösch, n.d.).
Presently, surgical billing remains a “black box” in medicine. For a variety of reasons (regulatory, insurance, hospitals, and overall complexity), the ability to provide real-time, accurate, and transparent costs for surgical procedures has never been feasible. Despite the recent enactment of cost transparency guidelines, healthcare costs are still often difficult to calculate and remain undisclosed (“Medicare and Medicaid Programs: CY 2020 Hospital Outpatient PPS Policy Changes and Payment Rates and Ambulatory Surgical Center Payment System Policy Changes and Payment Rates. Price Transparency Requirements for Hospitals To Make Standard Charges Public” 2019). Current accounting methods provide no efficient method for attributing the myriad of resources (human, supply, time, etc.) to a specific patient. Furthermore, the ability to reconcile individual records across multiple divisions is time-intensive and error-prone.
Key challenges for more efficient accounting are deeply rooted in how costs are documented and reported. Currently, facilities can provide estimated cost figures for procedures, but have no way of determining the true cost difference between operations. These estimates are primarily derived from charges for big-ticket items such as the facility, surgeon fee, and anesthesia fee, which are based on a multiple of the Medicare fee schedule. However, many line-item costs (i.e., surgical packs, gauze, dressing, etc.) are sometimes not even accounted for in the bill as these are contingent on manual documentation by the operating room (OR) nursing circulators. While speculation for surgical billing is standard practice, more advanced, accurate, and available methods should be implemented.
Recently, efforts have been made to use time-driven activity-based cost accounting (TDABC) to curtail this. TDABC centers around an algorithmic approach to defining each step in the healthcare process and the analysis of associated costs and outcomes divided per unit time. Studies have proven TDABC to be more accurate than traditional hospital accounting measures in quantifying costs in orthopaedic surgery (Akhavan, Ward, and Bozic 2016; Husted et al. 2018; Jayakumar, Triana, and Bozic 2021; Kaplan and Anderson 2004; Koolmees, Bernstein, and Makhni 2021; Palsis et al. 2018). However, TDABC accounting methods are built on a series of assumptions, are time/labor intensive, and error-prone.
The ability to provide transparent cost data quickly and accurately for specific procedures, facilities, and providers would be revolutionary. The application of blockchain technology to this real-world problem could be the solution. Many in the healthcare system, especially patients (and insurance providers) would benefit from real-time cost transparency in decision making regarding their care. While blockchain can provide granular detail for per patient cost in the form of facility cost (OR room), anesthesia cost, surgeon cost, per minute employee cost in the OR, cost of disposable equipment used, and cost of medications used, it can also account for uncaptured value. For example, room turnover between procedures is an often-neglected value in the calculation of cost. Under current accounting methods, this time is essentially vacant time that does not generate revenue. However, understanding it results in enormous value in how care is delivered along with realizing its untapped potential.
Healthcare is the only sector where consumers cannot receive a real itemized estimate and final bill that are reflective of all the line-item costs with granularity. The implementation of blockchain algorithms can allow the disorganized healthcare system to create real granularity and organization. Much like in the financial sector, the savings in healthcare realized would be tremendous in a sector that represents the largest part of the GDP (20% by 2025) (Keehan et al. 2016). Currently, the technology used is primitive (at best TDABC), as well as labor and time intensive for the facility staff. Blockchain technology has the potential to realize this unmet need. As each transaction occurs, everything attributed to the patient’s care journey can be tracked and recorded. The ability to continuously keep past records of performance will provide insight into future needs. Furthermore, blockchain is a self-verifying network, thus trust, a vital component for successful transactions, is built in. Ultimately, this ledger holds promise to reduce the need for intermediaries from a supply and reimbursement standpoint.
1) Surgical Billing & Supply Chain
To highlight the benefit of blockchain technology in supply chain management, an ambulatory surgical center (ASC) will serve as the example.
First, blockchain may replace the current slow, manual processes of managing inventory. Presently, ASCs have several staff responsible for documentation of all supplies from office equipment (i.e., toner, pens), surgical supplies (i.e. gowns, gloves), and surgical implants (i.e., prostheses, anchors, etc.) to list a few. This maintenance requires constant upkeep and vigilance yet remains error-prone. While full implementation of an automated blockchain supply inventory will take further advances and years to realize, the promise of accelerating supply chain timelines and reducing errors is clear.
Second, blockchain can improve the traceability of supplies. From assisting in root cause analysis of adverse events to quality control of supplies, blockchain’s degree of transparency underscores areas of improvement across supply chain operations.
Third, blockchain may reduce transaction costs and thus improve margins. With the inclusion of smart contracts (defined below), many supply chain operations may be triggered automatically as conditions are met. Smart contracts can monitor follow-through or breach of contract and trigger action immediately. This automation will reduce operation time, reduce costs, and reduce reliance on intermediaries or third-party verification. The potential to know with certainty the amount of resources needed and used, not to mention items available, will steeply reduce the cost to verify, thus lowering transactional costs.
2) Smart Contracts
Newer blockchain platforms, such as Ethereum, possess the ability to include the transformative technology of smart contracts into their network. Smart contracts are contracts integrated in the blockchain itself that can continuously monitor information and simultaneously automate responses once a series of negotiated conditions are met. Smart contracts can replace intermediaries, reduce mismanagement, and ultimately improve efficiency.
Smart contracts can be structured to automatically adjust costs and compensation of members in the chain (Bottoni et al. 2020). For example, in ASCs, many implant supplier contracts require a percentage of utilization to trigger a discount. For instance, a smart contract can send payments to a supplier as soon as shipment is delivered. This provides an opportunity for automation and the honoring of contracts.
Smart contracts have enormous potential from a health insurance processing perspective. Blockchain provides an audit trail to prove and verify your work instantly. Presently, it is not uncommon for providers to be denied reimbursement for services rendered weeks earlier due to the failure of proper documentation. Providers and patients routinely wait weeks for insurance approval for a particular treatment (i.e., injectables, diagnostic studies, invasive procedures) (“How Insurance Companies’ Red Tape Can Delay Patient Care,” n.d.). The challenge of the current system is the significant time delays between services rendered, documentation, and ultimately verification and approval. Currently, contracts between insurance companies and providers base reimbursement/approval on predetermined requirements such as diagnostic indications, treatment protocols, and quality metrics. However, with smart contracts, verification of service rendered can be accelerated and the equally important recognition of documentation errors can be corrected in real time. Smart contracts can change how medicine is practiced, reducing the burden of administrative barriers for many health systems.
Conclusion
While blockchain’s detractors will cite security concerns, it must be recognized that the current data systems are less secure than perceived. In 2019, there were over 500 healthcare data breaches resulting in 40 million records exposed or stolen (Winder, n.d.). These breaches reached a 17-year high in 2021 with extremely costly recoveries associated per breach—on average $9.4 million USD per breach in the US (“The Average Cost of a Healthcare Data Breach Is Now $9.42 Million” 2021; “Cost of a Data Breach Report 2021” 2021).
Full implementation is years away, however, one step physicians can take to incorporate this promising technology into their ASC and practice is to add Bitcoin or some form of cryptocurrency as a payment option. Starting small and focusing on single use applications is key. This will in turn allow multiple departments such as the business office, information technology (IT), finance, accounting, and sales to build up blockchain capabilities.
Ultimately, as these processes become automated, roles will change for intermediaries such as lawyers, accountants, and administrators. As physicians, understanding this technology and being actively involved provides an opportunity to influence the future of how medicine and care is delivered.