Introduction
Arthroscopic surgery is the most common orthopedic procedure in the United States, with close to 1.8 million procedures performed in 2017 (Shah, Solow, Kelly, et al. 2018). By 2027, the arthroscopic market value is expected to rise to US $16.3BN (“Acumen Research and Consulting” 2021). Arthroscopic surgery has become the standard for many procedures, as it allows surgeons to visualize various joints of the body via small incisions—a key advantage over the larger incisions of open surgery. The history of arthroscopic surgery can be divided into three eras: the incandescent era (1912 to 1970), the fiber-optic era (1970 to 2022) and the wireless era (2022 and beyond). Despite many advances in the fiber-optic era, key aspects of arthroscopic devices remain unchanged. Most notably, the power requirements of current light technology have kept arthroscopic cameras tethered by both light and power cables to the surgical tower. Traditional arthroscopic camera systems have several drawbacks. Fiber-optic connectivity requires high wattage and significant attendant heat and can sometimes cause OR fires and patient burns. Likewise, the long cables that connect the remote tower to the sterile field require significant setup and takedown times and put OR staff at risk for trips and falls.
The ArthroFree wireless surgical camera system recently received market clearance from the FDA.
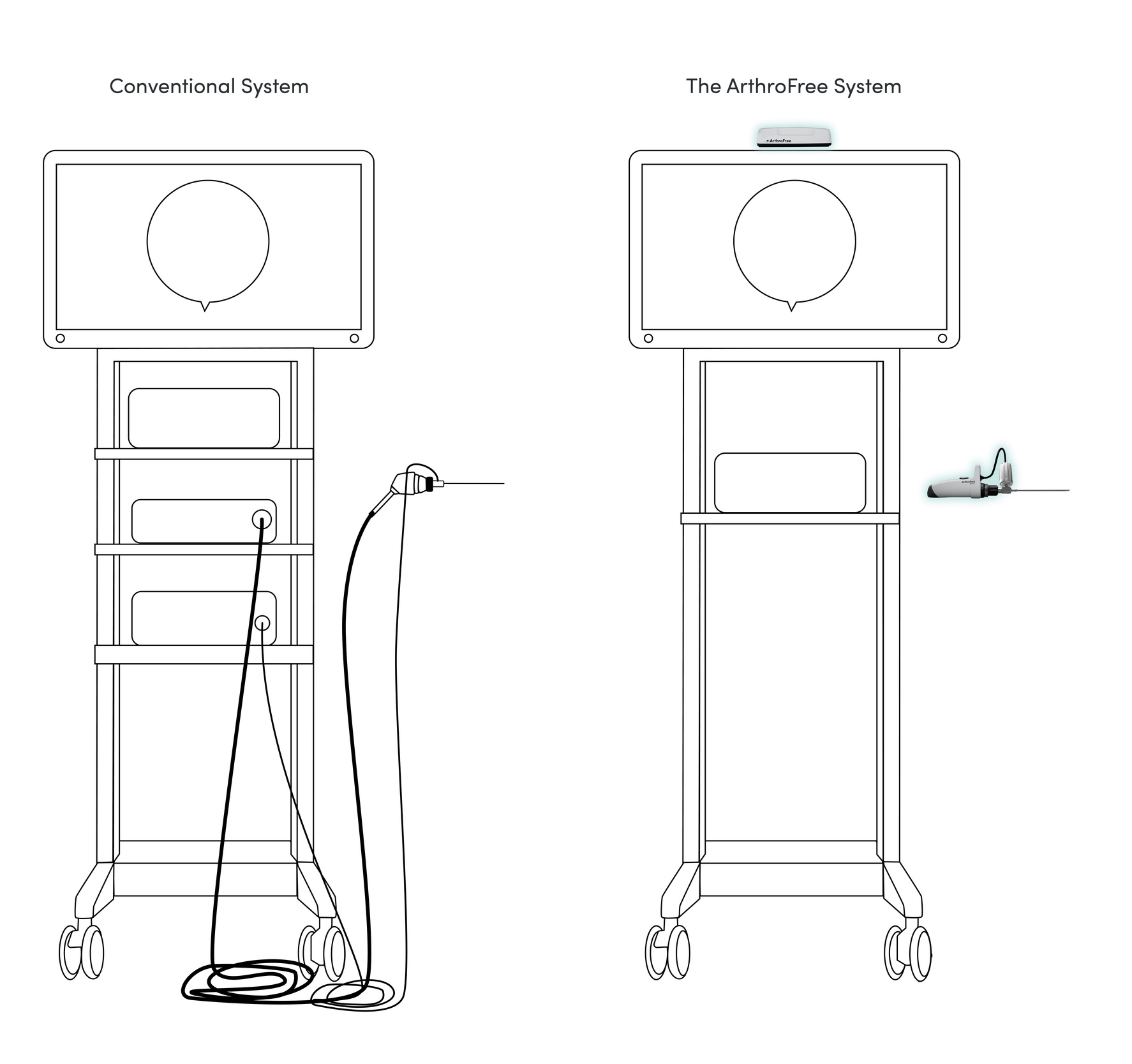
This system is designed to free the surgeon from the tethers of video power cables and fiber-optic light cables, in order to allow more ergonomic and efficient surgical movements, which will likely shorten procedure time. With fewer items in the sterile field, the ArthroFree System is expected to improve OR efficiency via shorter setup and takedown times. The power box and light box on the tower, as well as their connecting cables, are no longer necessary. With fewer items to purchase and replace, as well as improvements in OR efficiency, costs per case are expected to decrease. The ArthroFree System is also expected to make arthroscopic surgery safer for staff and patients: having fewer cables reduces potential trip hazards making it safer for OR staff, and elimination of light source-induced heat injuries (OR fires and patient burns) equals better patient outcomes. The wireless arthroscopic era has now begun with the FDA clearance of the ArthroFree system.
The Arthroscopic Incandescent Era
For centuries, man’s long-standing fascination with what lies inside the human body has been hampered by how to get light into the body and how to display an image outside the body. Initial attempts at solutions entailed placing a tube into an orifice (i.e., direct visualization). The earliest evidence of this method includes the vaginal spectrum and proctoscope discovered in the ruins of Pompeii (Jackson 1996).
In the early 19th century, Dr. Philipp Bozzini develop the Lichtleiter: a cystoscope that included a tube for visualization and a tube for a candle-powered light source (“From Lichtleiter to Fiber Optics” 1973). In 1853, Dr. Antonin Jean Desormeaux improved the cystoscope by using mirrors to reflect light from a turpentine and gasoline lamp into the body (Figdor 2004). Historians consider this to be the first endoscopic instrument. The technology limits of illumination continued past 1879, the year Thomas Edison invented the light bulb. In 1886, Dr. Joseph Leiter was the first to incorporate an incandescent bulb into a cystoscope (Bassler and Yang 2012). Advancements in the visualization of joints soon followed. In 1912, Dr. Severin Nordentoft used a laparoscope to examine the interior of the knee: a procedure he described as “arthroscopy (Kieser and Jackson 2001).” “Arthroscopy” has Greek origins: arthro for “joint” and scope for “view.” Dr. Kenji Takagi, long recognized as the father of arthroscopy, used a cystoscope in 1918 to visualize the knee joint (Takagi 1933, 1939). Dr. Masaki Watanabe, a student of Dr. Takagi, developed the first arthroscope for clinical use in the 1950s (Masaki Watanabe 1986; M. Watanabe 1954). Dr. Watanabe represents a compelling rival for the designation of father of modern arthroscopy, based on his development of the Watanabe number 21, which entered production in 1959. It proved far more advanced than the devices developed by his mentor. Watanabe’s arthroscope contained a straight-ahead optical system and an incandescent bulb at the tip. Due to problems related to the incandescent bulb, which often became dislodged from the tip of the scope, the “21” was the last arthroscope produced with an incandescent light source. In 1970, Dr. Watanabe produced the number 25, the first ultrathin fiber-optic arthroscope.
The Fiber-Optic Era
Soon after the introduction of fiber-optic cables, technological advancements resulted in the ability of surgical cameras to project an image of the interior of the knee joint onto a monitor. This occurred in the mid-1970s and allowed surgeons to see directly inside the knee without looking directly through the arthroscope. The advent of the first rod-lens arthroscope by Dr. Richard O’Connor made it easier to shift from (mostly) diagnostic arthroscopy to the surgical treatment of joint pathology (Kieser and Jackson 2006). Arthroscopy as a surgical technique grew slowly. The International Arthroscopy Association was established in 1972 with Dr. Watanabe serving as the inaugural president. In 1975 Dr. John B. McGinty was the first to mount a video camera to an arthroscope and operate via a television monitor (McGinty 1976). This was soon followed by Dr. Lanny Johnson’s motorized shaver. These advancements allowed surgeons to develop reconstructive procedures (e.g., anterior cruciate ligament reconstruction). In 1982, the Arthroscopy Association of North America (AANA) was founded to promote arthroscopic surgery by the education of orthopedists. Soon thereafter, the field grew exponentially. The volume and complexity of arthroscopic procedures, techniques, equipment, and outcomes followed suit. These developments made many open-surgical treatments unnecessary. Today, surgeons use arthroscopic instruments and techniques to treat a variety of pathologic states for almost every joint of the body.
Technological advancements in arthroscopic equipment have been subject to refinement and revision over the last 50 years. Med-tech companies have repeatedly refined the image quality, monitor size, video latency, and even camera shapes. The shift from Xenon to LED lighting improved the visualization process; current data capture methods are also much improved. Still, as the “untethered era” approaches, the arthroscopic camera remains tethered to the surgical tower—just as it was 50 years ago. The technological advances needed to cut loose from the power cable and the fiber-optic cable have long been prohibitive.
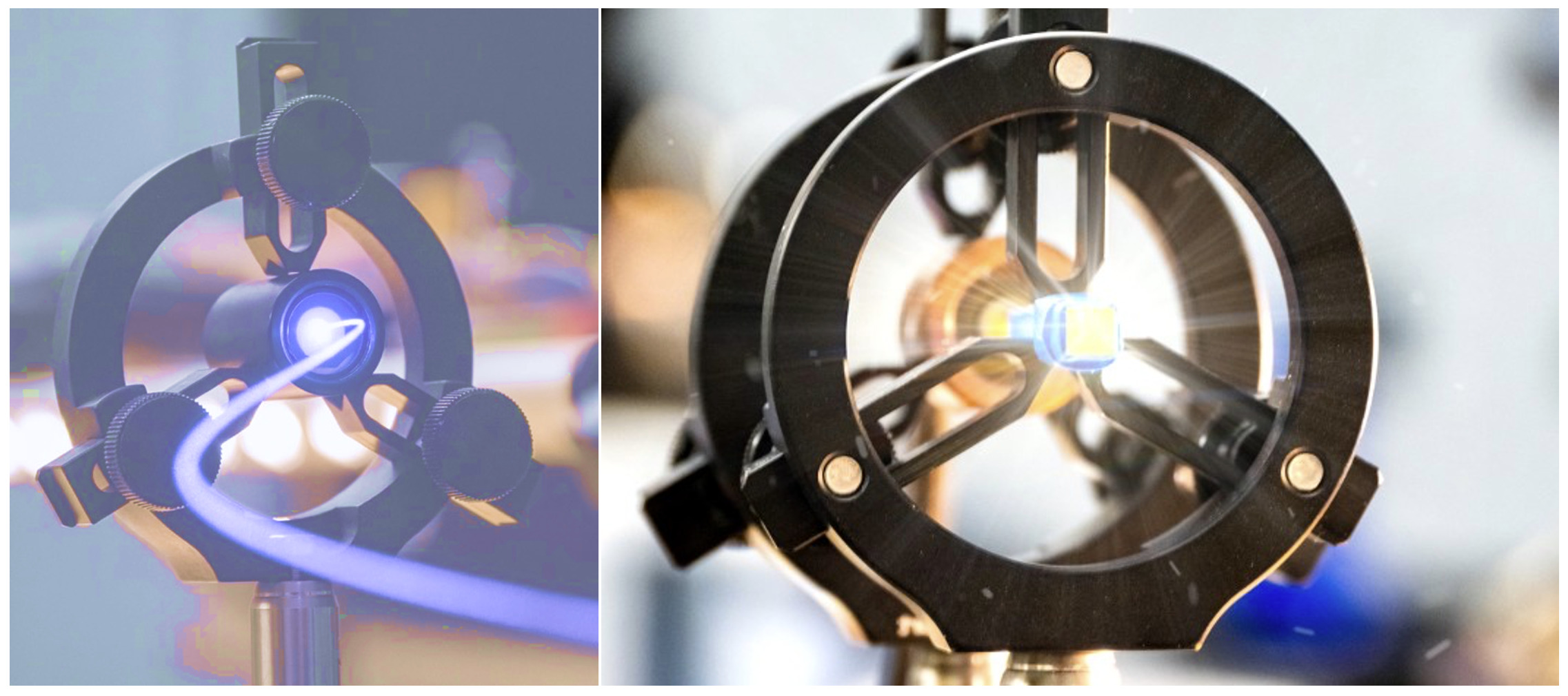
Attempts to make a wireless camera using an LED light source have failed largely due to energy consumption and heat generation. Even the most efficient rechargeable batteries last only a short time, and the camera becomes too hot to hold. In 2015, though, the engineers at Lazurite invented a low-heat, laser-based light source. The light engine inside the ArthroFree wireless camera utilizes MeridiemTM light technology, one of the key entries in the IP portfolio of Lazurite. This MeridiemTM light engine requires less than 1% of the energy used to power current LED surgical camera systems.
Lazurite also engaged surgeons to determine the best size and shape of the ArthroFree camera. Their engineers invited 20 arthroscopic surgeons to choose from eight camera shapes: 80% chose ArthroFree’s current camera shape. The ArthroFree wireless surgical camera—with its novel light source, rechargeable batteries, and proprietary wireless technology—eliminates the need for a remote video-power box, the light box, and the corresponding cables.
Finally: The Wireless Era
There are a host of benefits that come with the use of a wireless surgical camera in arthroscopic surgery. The foundational technologies of the ArthroFree System—the high-efficiency, low-heat light source and its military-grade wireless connectivity—pave the way toward many of these benefits. A high-efficiency battery technology in a lightweight casing powers the light engine, and the wireless connection between the camera and the receiver frees the surgical camera handset from the surgical tower. With the elimination of the fiber-optic light cable and the video power cables, OR staff can expect the surgical risk of light source-induced patient burns and OR fires, OR staff trips and falls, and the incidence of surgical site infections via cable contamination will see a reduction or be eliminated. 3MTM indicates that their IobanTM antimicrobial incision drapes have a flashpoint of 121.1°C (3M 2020). Spradling et al. (2015) measured the peak temperature of a flexible fiber-optic ureteroscope scope connected by a fiber-optic cable to be 194.5°C. Lazurite Holdings LLC measured the peak temperatures of the light source component of the ArthroFree surgical camera to be 43°C—well below the 48°C of the ISO standard 60601-1 in terms of maximum temperature for device contact with patient, for 1m 1s to 9m 59s.
All participants in the performance of an arthroscopic surgical procedure stand to benefit from a wireless surgical camera. The surgeon will be able to move more ergonomically, comfortably, and efficiently.
The wireless age will mark the end of the “short-cabled” surgeon. During the procedure, surgeons are sometimes unable to get the camera to the operative site due to inadequate length measurements prior to securing the cables to the drapes. The options at that point include either pulling potentially unsterile cables into the sterile field or removing and replacing the camera and light cord. The first puts the patient at risk for contamination and infection. The other delays the start of the case, while the circulating nurse tracks down another camera and fiber-optic cable. Surgeons also get frustrated when cables get caught or tangled. The movement of the camera from one portal to another, or the rotation of the lens to look in a different direction, can introduce additional delays to a procedure. Less equipment also means less chance of delays related to technical problems with the arthroscopic camera system.
In a human factors study performed by Lazurite, 70 arthroscopic surgeons tested the ergonomics of the ArthroFree camera. Surgeons indicated that it was comfortable to hold (80.8%), intuitive to use (93.8%), and generated very little heat (95.8%).
Surgeons also expected the ArthroFree System to improve patient safety and OR efficiency. Ninety-four percent of the surgeons in this study stated they could confidently do surgery with ArthroFree. The wireless era is expected to produce shorter surgical case times and, in turn, replenish a resource in short supply for surgeons: “free time.”
Due to fewer items in the sterile field, nurses are expected to require less time for setup and takedown. With the elimination of the light box and its corresponding cable, they will also be freed from the worries of OR fires and patient burns. Scrub nurses and techs benefit, too as there will no longer be a need to disentangle cables during setup or surgery.
Lazurite conducted an OR simulation setup and takedown pilot study with OR nurses to compare the ArthroFree wireless camera system to a traditional camera system. Results of the study demonstrated that ArthroFree was 43.6% more efficient in terms of setup, 30.7% for takedown, and 39.3% overall. The most striking finding of this study was that the setup and takedown of the ArthroFree System only required the scrub nurse/tech. With conventional camera systems, the scrub nurse/tech is needed to hand off the cables, and the circulating nurse is needed to connect (or disconnect) them. With ArthroFree, the circulating nurse is free to attend to their other OR tasks. The nurses in the Lazurite study expected ArthroFree to improve patient safety, make their jobs easier, and reduce their overall level of job stress.
Efficiencies extend to central processing, too. A Lazurite study of surgical processing department (SPD) managers concluded that ArthroFree processing will require fewer steps, take less time, cost less, improve SPD efficiency, and reduce the stress level of the SPD staff.
Hospital and ambulatory surgery center administrators will benefit as well from adoption of the ArthroFree camera system. Benefits include improved OR efficiencies, a reduction in energy and replacement expenditures, reduction in costs per case and a safer and less stressful environment for OR personnel.
The greatest beneficiary of these innovations will undoubtedly be the patient. Shorter surgery times for patients means less time under anesthesia and, in turn, a reduced chance of post-operative anesthetic complications. They will also benefit as there will be less chance of infection from contaminated cables along with the elimination of burns from the high heat light source and fiber-optic cables. The ArthroFree System is likely to usher in a new paradigm in arthroscopy.
Summary
Arthroscopic surgery has evolved from the incandescent era to the fiber-optic era and is now on the brink of the wireless era. With its disruptive technology, wireless arthroscopy will change the field of arthroscopy as we know it. Value-based care will continue to drive healthcare for the immediate future. The technology ArthroFree incorporates is sure to improve patient outcomes and demonstrate cost-effectiveness, two of the key tenets of value-based care. Wireless arthroscopy will become the standard of care in hospitals and ASCs due to its safety profile, OR efficiencies, and cost savings. As patients become more familiar with the benefits of wireless arthroscopy, it would be natural for them to seek out clinicians that deliver the safety and efficiency commensurate with arthroscopy in the wireless era.