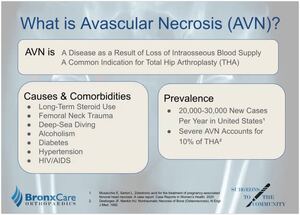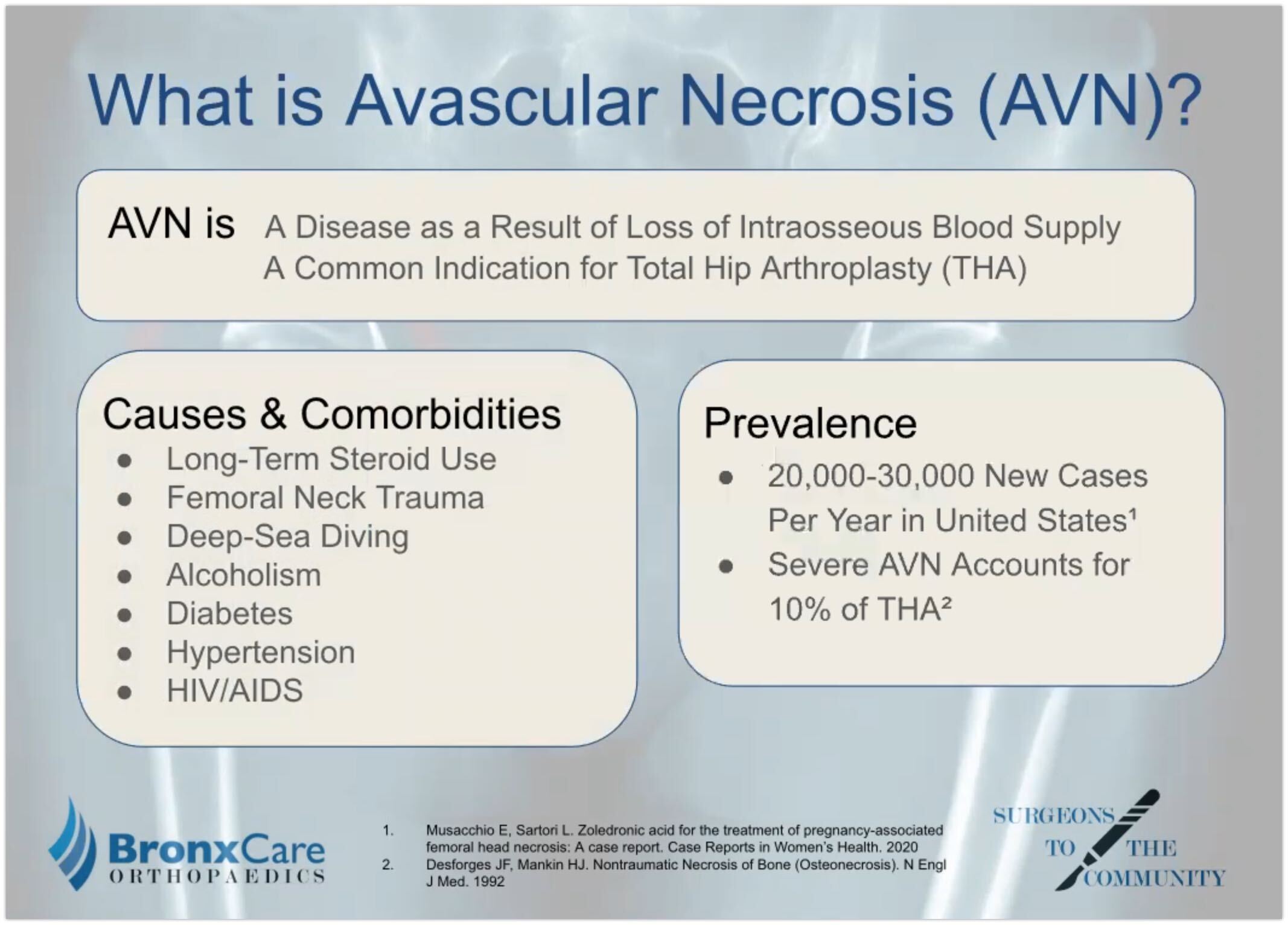
What is avascular necrosis? It’s a disease that results from a loss of intraosseous blood supply. And there is a range of causes and comorbidities, including trauma to the femoral head and neck, deep-sea diving, alcoholism, and having an HIV-positive diagnosis.
Avascular necrosis is a common indication for total hip arthroplasty, a severe cases account for 10% of the annual total hip cases.
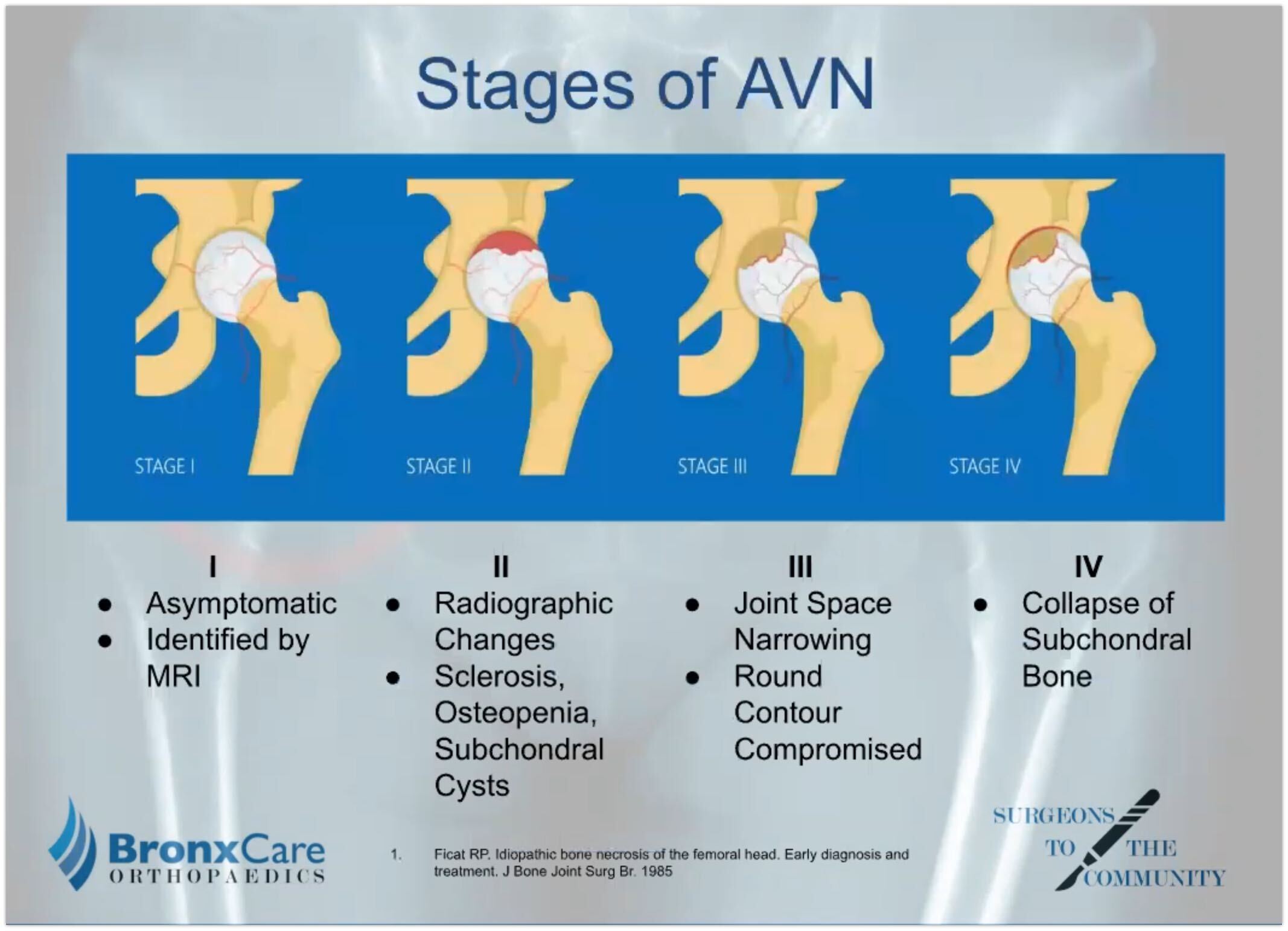
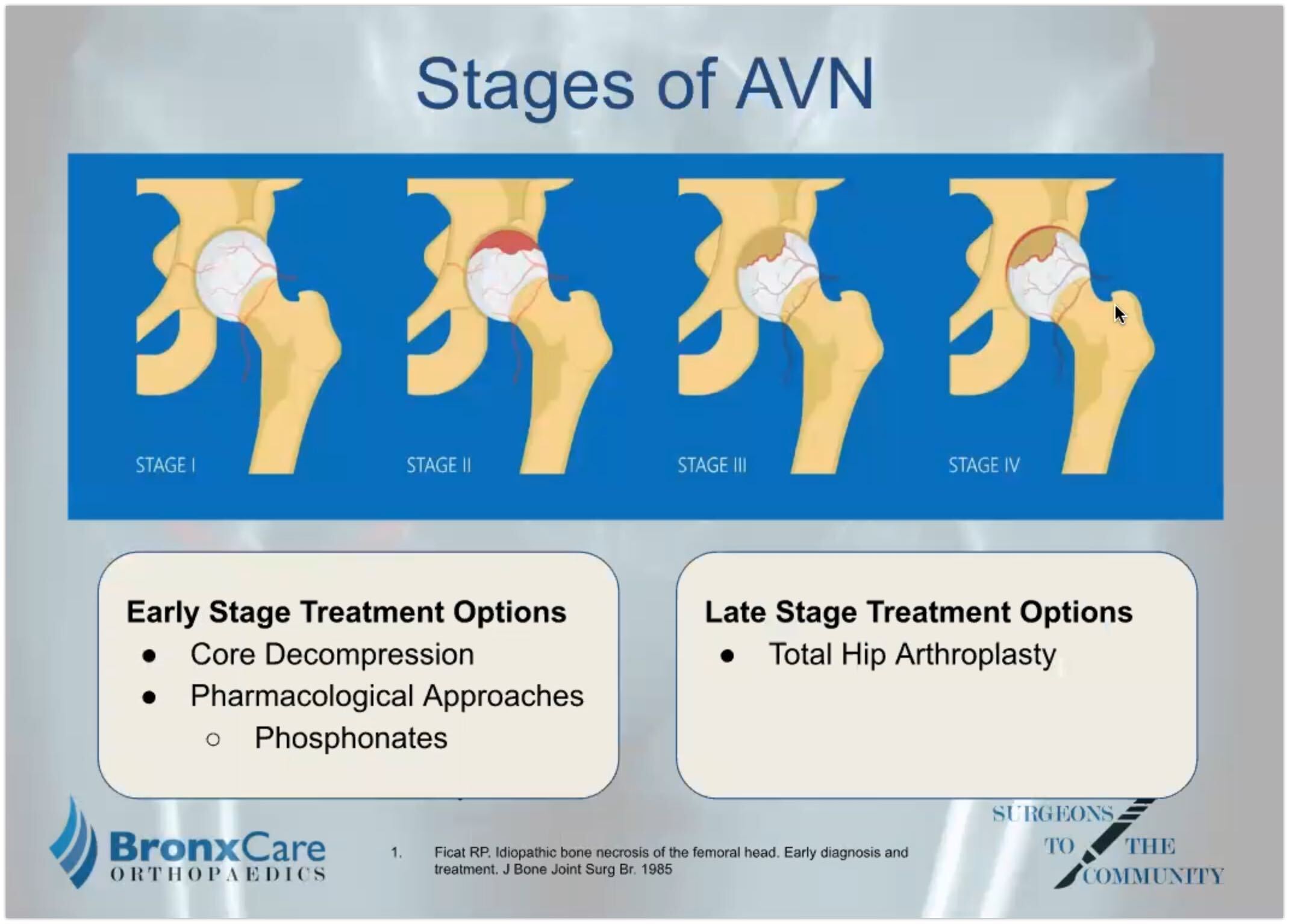
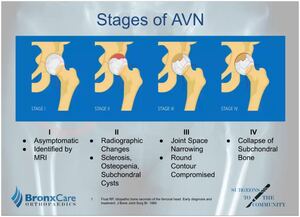
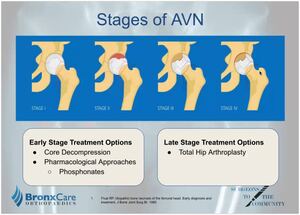
There are four stages of avascular necrosis of the femoral head ranging from asymptomatic to total collapse of the bone. Core decompression is indicated in the early stages as well as drugs such as bisphosphonates. Total hip arthroplasty is indicated for the more severe cases of AVN.
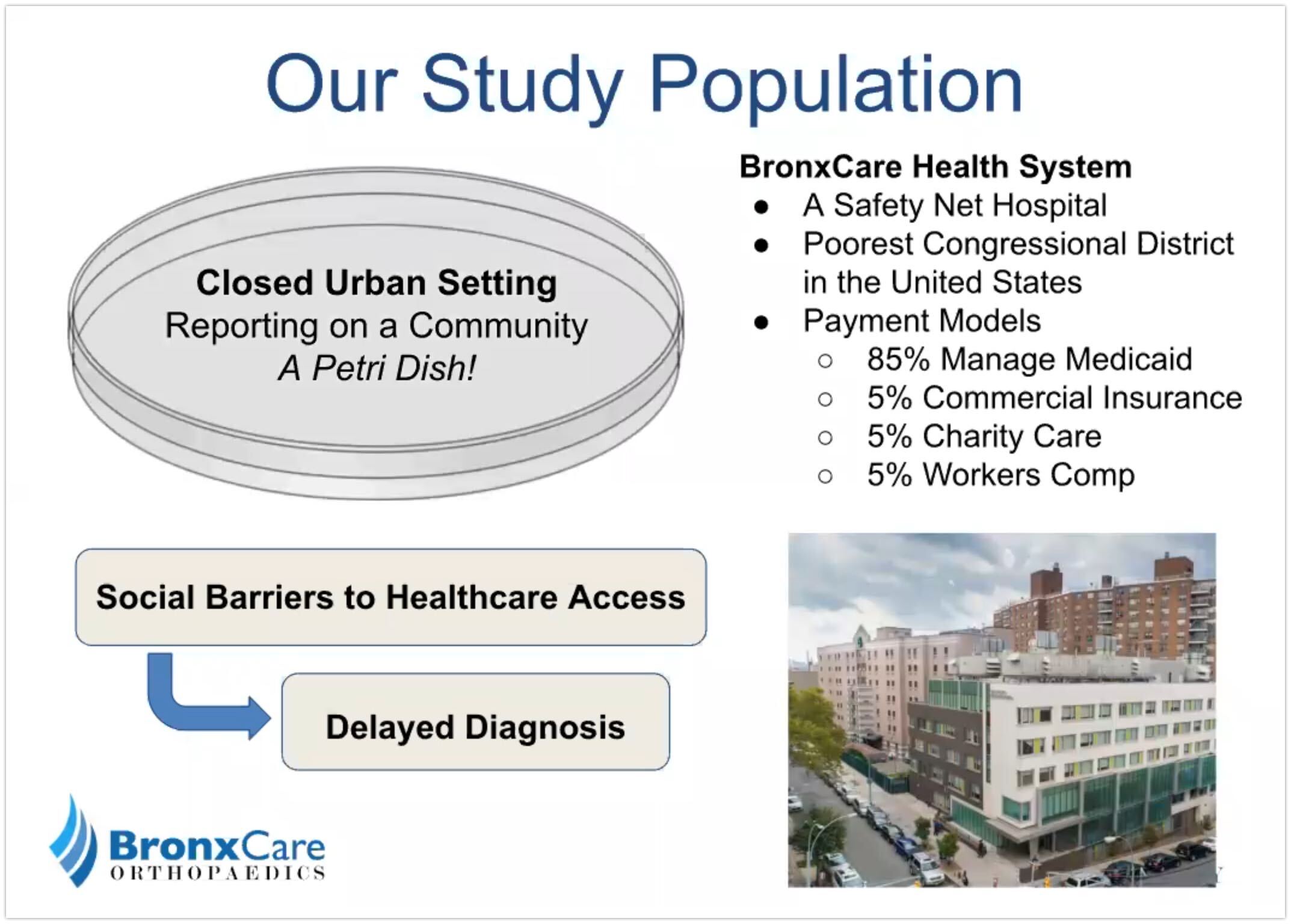
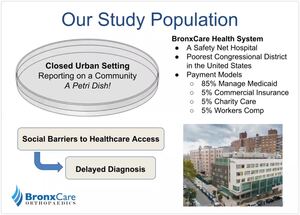
We have the privilege of working with the unique population of BronxCare. Being located in the poorest congressional district in the United States, there are many existing social barriers to healthcare.
Unfortunately, this oftentimes leads to delay diagnosis and advanced disease progression. Eighty-five percent (85%) of patients at BronxCare utilized manage Medicaid. While the remaining 15% are evenly split between Commercial Insurance, Charity Care, and Workers’ compensation payment models.
From a research lens, we can consider this community a closed urban setting. To create an analogy, this community is like a petri dish for healthcare. As patients tend not to leave the Bronx for care nor do they come into the Bronx for care.

Some of the aims of our study were to evaluate the frequency of AVN for patients who underwent a total hit. We also wanted to identify the prevalence of AVN in a closed urban setting. And also, the prevalence of comorbidities relevant to AVN within the context of a safety net hospital.
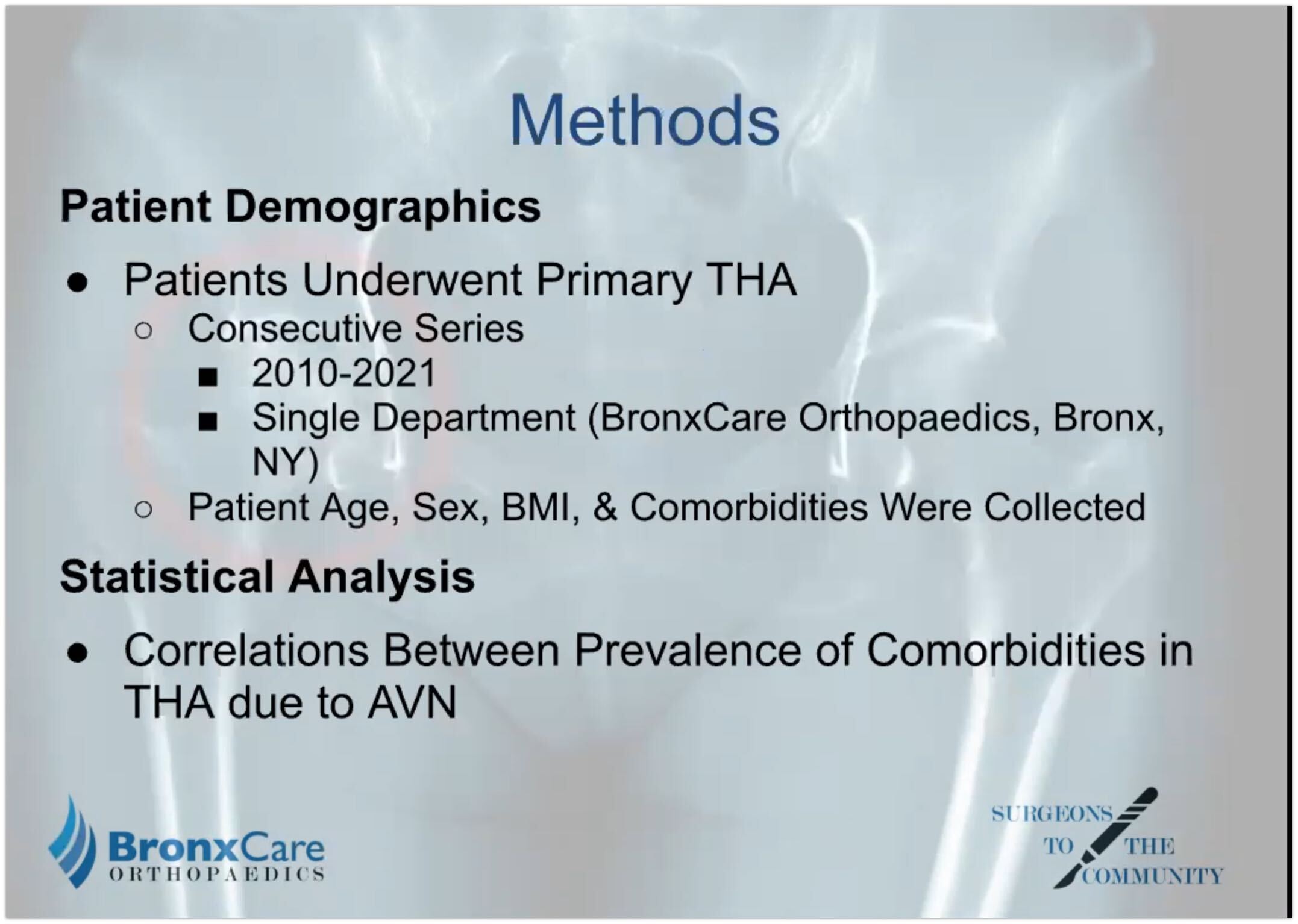
This retrospective study reported on a consecutive series of patients from 2010 to 2020 within a Single Orthopedic Department. We first collected patients’ demographic information and comorbidities and then did statistical analysis including driving correlations between common comorbidities and the prevalence of total hip arthroplasty due to AVN.
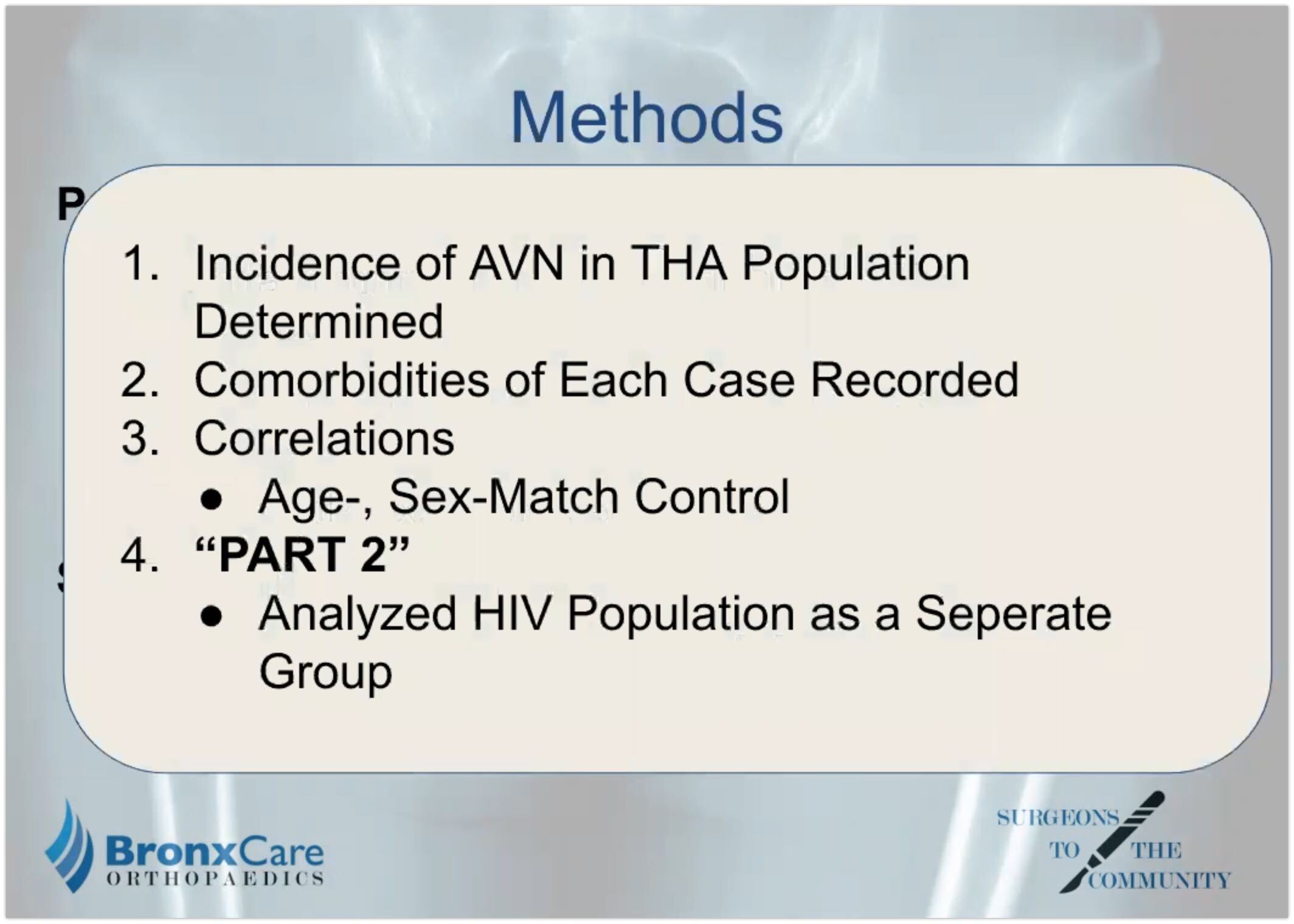
In summary, we first collected all total hip patients and identified which were indicated for a procedure due to AVN. Then, we recorded the comorbidities of the avascular necrosis patients. We generated a one-to-one agent sex match control group of total hip patients who did not have AVN. And then, we separate outpatients with HIV as specific comorbidity for further analysis.

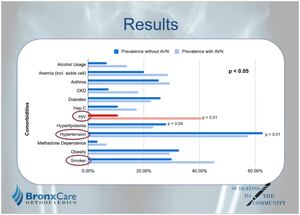
Of the 613 hips that underwent arthroplasty, 24.5% were due to AVN. Within this AVN group, 40.7% of the patients had a history of HIV. And looking at the age-sex match control group of patients who underwent a total hip without AVN, this number was only 10.7%.
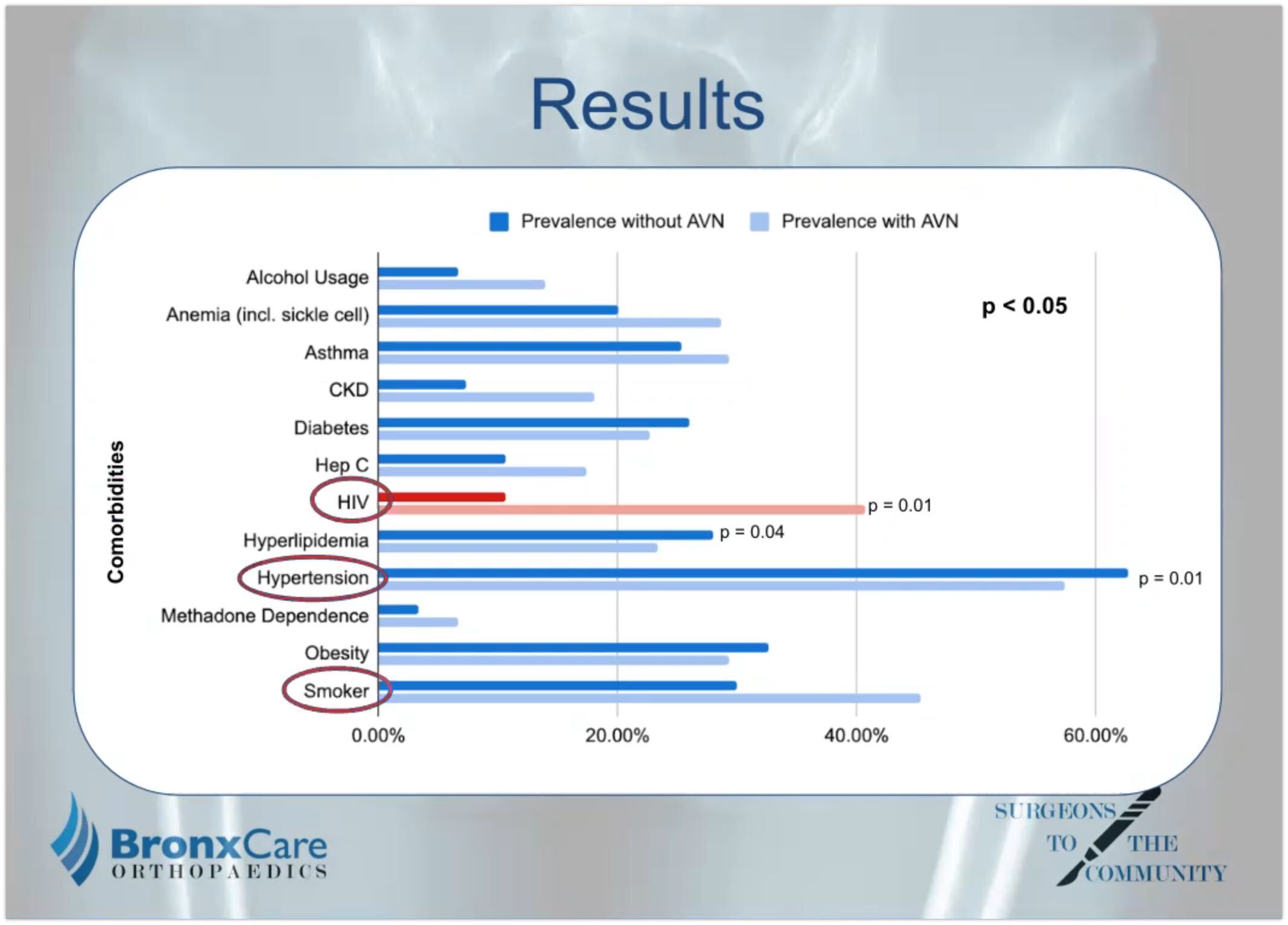
Among the comorbidities, hypertension, smoking, and HIV-positive were the most common in the AVN total hip population. Comparing total hip due to AVN and non-AVN, HIV was the only comorbidity to demonstrate a significantly higher proportion in the AVN group.
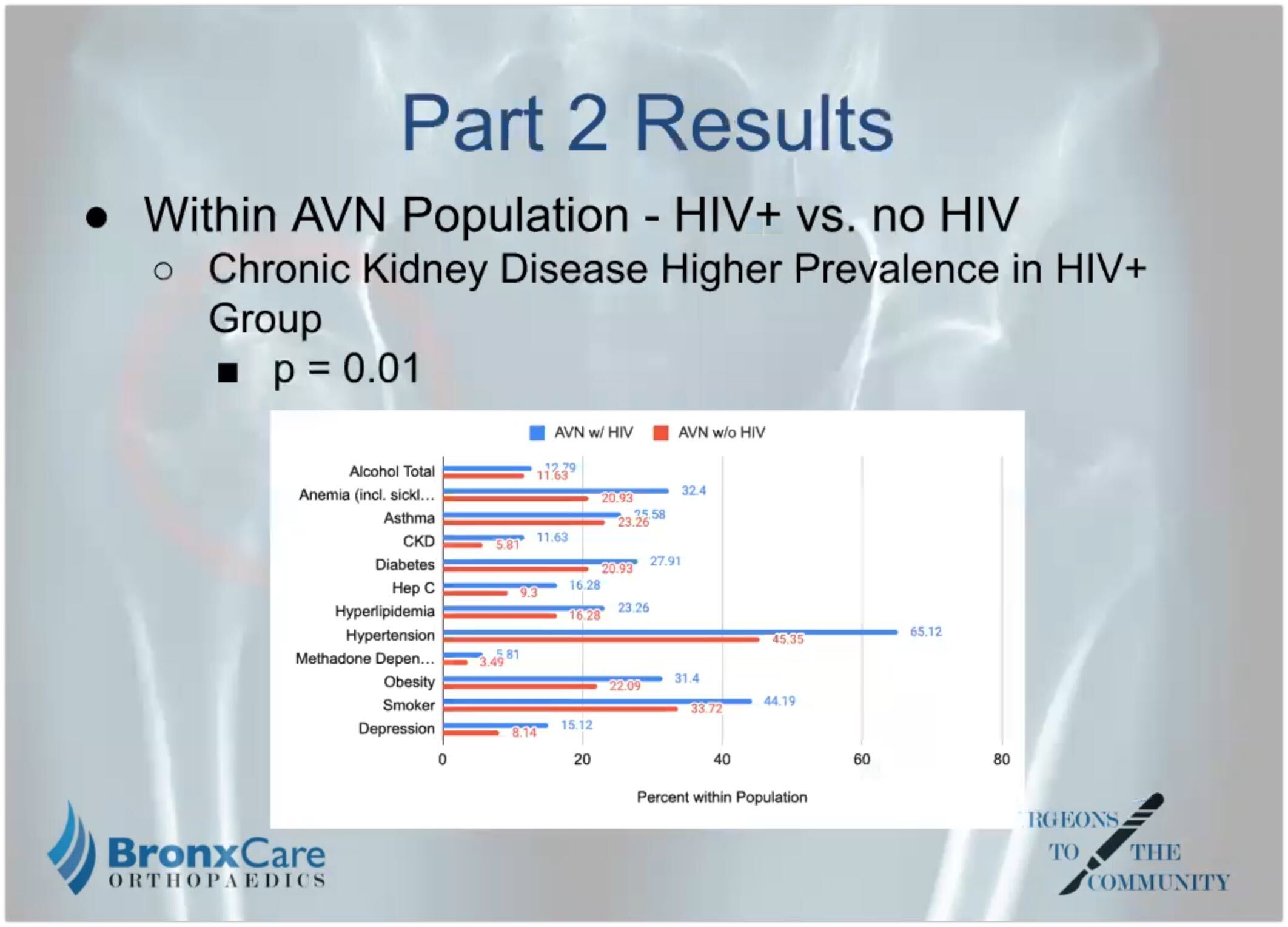
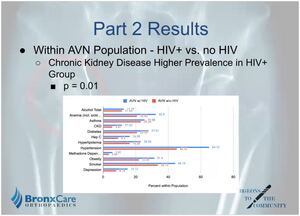
We also created an age-sex match within the AVN population looking at patients with a history of HIV and patients without HIV. Comparing the comorbidities, we found that CKD had the only significant difference. However, the HIV group had a higher prevalence of comorbidities overall.
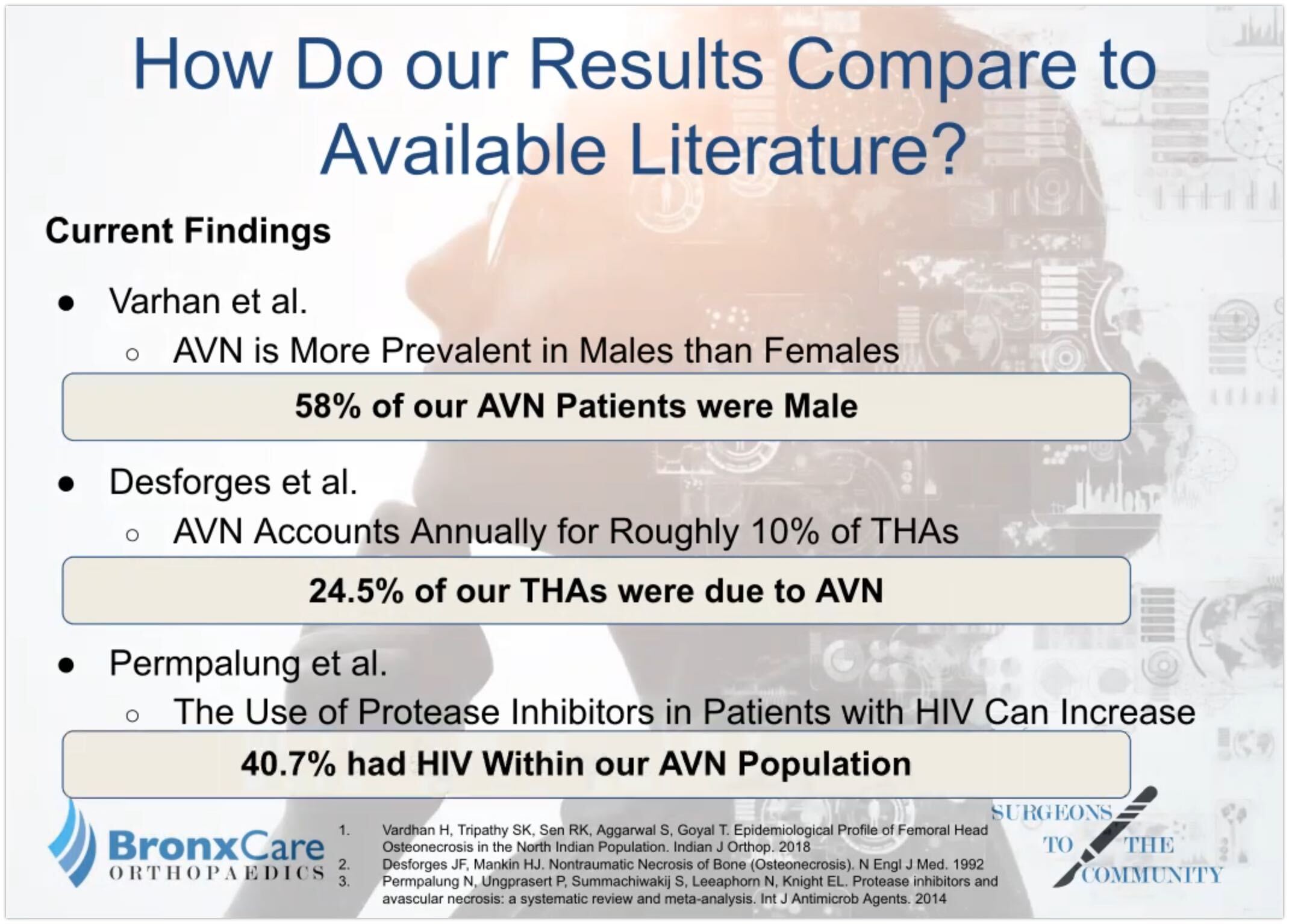
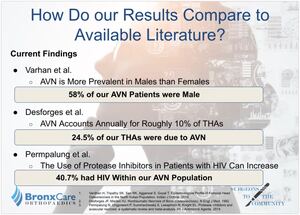
Based on our results, our study both disagrees, agrees and calls upon further research when compared to prior literature. Our say supports the notion that AVN is more prevalent in males than females.
Yet our study identified a much higher prevalence of AVN in patients requiring total hip. And within our population of a very high proportion of AVN patients were HIV-positive.
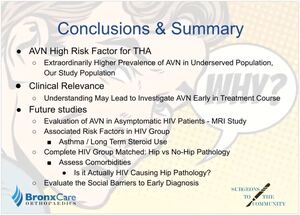
In conclusion, AVN is a high-risk factor for total hips and there is a much higher prevalence of AVN in an underserved population like the one in our study.
Understanding these results may lead to investigating AVN early. And then, communities with a high prevalence of HIV patients reporting hip pain should not be overlooked.
This study in our results went further future analysis, including evaluating AVN and asymptomatic HIV patients such as through an MRI study. Evaluating the associated risk factors in HIV groups such as asthma or long-term steroid use. Or completing an HIV group matched in hip versus no hip pathology to assess differences and comorbidities.
Overall, we believe that evaluating the social barriers to early diagnosis is most relevant in improving future patient care.