Hyperglycemia is closely associated with poor postoperative outcomes. Preoperative protocols that do not identify poorly controlled diabetics may be placing patients at an increased risk of postoperative complications, including superficial and deep infections. Thus, my colleagues and I set out to assess the prevalence of undiagnosed diabetes among elective orthopedic surgery patients using a preoperative hemoglobin A1c (HbA1c) test. We also aimed to evaluate short term clinical outcomes and any possible surgical delays due to poor glycemic control.
The How
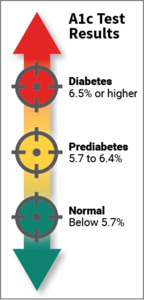
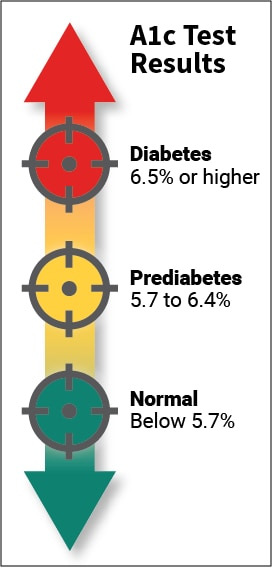
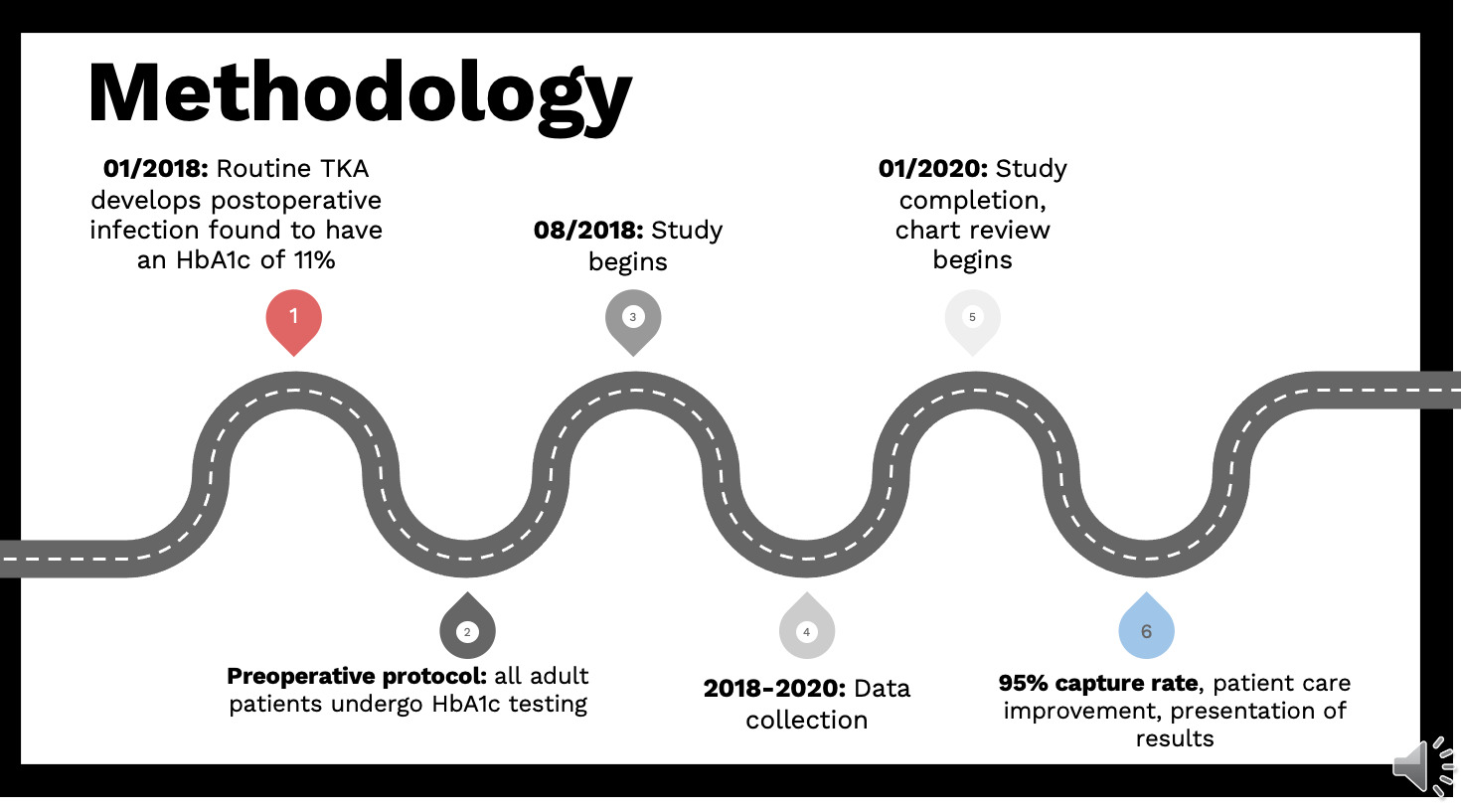
The inception of this work was in January 2018 when a patient underwent a routine total knee arthroplasty (TKA) and subsequently developed a postoperative infection. The patient was found to be a previously undiagnosed diabetic and a hemoglobin (HbA1c) obtained postoperatively was 11%. We decided to undertake a prospective analysis of orthopedic patients over the age of 18 presenting for elective orthopedic surgery at our community clinic. All clinic patients had an HbA1c test drawn within three months of surgery. From August 1, 2018 to January 1, 2020 we were able to obtain over 200 patients for our study with a 95% capture rate (253 patients met the inclusion criteria). We evaluated patients’ medical records for demographic, surgical and perioperative data. From our study we were able to determine the local community prevalence of undiagnosed diabetes and prediabetes among all previously undiagnosed dysglycemic patients.
The Results
Concerning the 173 patients with no known medical history of prediabetes or diabetes, we found that one third of that group was diagnosed with prediabetes or diabetes using a simple HbA1c test. 5 of those individuals were diagnosed with diabetes, while 43 patients were diagnosed with prediabetes. The postoperative complication rate was 6.2% with no direct association to preoperative HbA1c or any of the demographic variables. We found that a body mass index (BMI) over 30 was associated with an elevated preoperative hemoglobin HbA1c value. Obese patients had an average HbA1c of 5.78, while non-obese patients had an average HbA1c of 5.49.
Of the cancellations, 20% had an elevated preoperative HbA1c value with no previous diagnosis of diabetes or prediabetes. However, none of the undiagnosed dysglycemia patients had an elevated HbA1c above 6.6 and surgery cancellation occurred for reasons other than for improved glucose control. Of the cancelled patient group 3 out of 17 (17.6%) patients with past medical history of diabetes or prediabetes had surgery postponed because of a need for improved glucose control prior to surgery.
Diabetes and uncontrolled perioperative glucose levels can lead to an increase in postoperative complications and thus increased healthcare cost. As the prevalence of dysglycemia increases, appropriate screening and perioperative management continue to have important clinical consequences. Understanding the relationship between glycemic control and postoperative complications is imperative in preoperative optimization. The goal of preoperative testing is to avoid intraoperative and postoperative surprises and improve any potentially modifiable risk factors. Implementation of a reproducible preoperative protocol that requires all adult patients who undergo elective orthopedic surgery to have a simple HbA1c test can lead to identification of a high number of patients with unknown dysglycemia.