The What
For some time, the gold standard for periprosthetic joint infection has been a two-stage revision arthroplasty where the initial step is to remove the infected implant, and then debride the infected tissue. Following this, an antibiotic cement spacer is inserted to maintain soft tissue tension; then the patient undergoes at least 6 weeks of systemic antibiotic therapy. The second stage of the surgery involves implantation of the revision arthroplasty components.
This stands in contrast to a single-stage revision. In this procedure everything is done at one time—the infected components are removed, a radical debridement is performed whereby not just the infected tissue, but a margin of healthy tissue is also resected en bloc, and then the revision components are implanted.
The Why
Single-stage revision arthroplasty is becoming more popular as there are several advantages to this procedure. For example, there are fewer hospitalizations because there is only one surgery required; there is also less morbidity. On occasion there may be a shorter antibiotic duration due to the radical debridement.
Recent data has shown that infection-free success after single-stage revision can be anywhere from 77-100%, which is comparable to a two-stage revision. However, the most common cause of failure and reoperation is for a single-stage revision—especially in more recent times with reduced infection rates—remains unclear. Many recent studies suggest that aseptic loosening can be equally as common as recurrence of infection.
Thus, we set out to more definitively address this question using a meta-analysis, where we tried to assess the reoperation rates secondary to infection and aseptic loosening in single-stage revision total hips and total knees. Secondarily, we looked at the overall reoperation rate, i.e., survivorship, other etiologies of reoperations and the overall mortality rate
The How
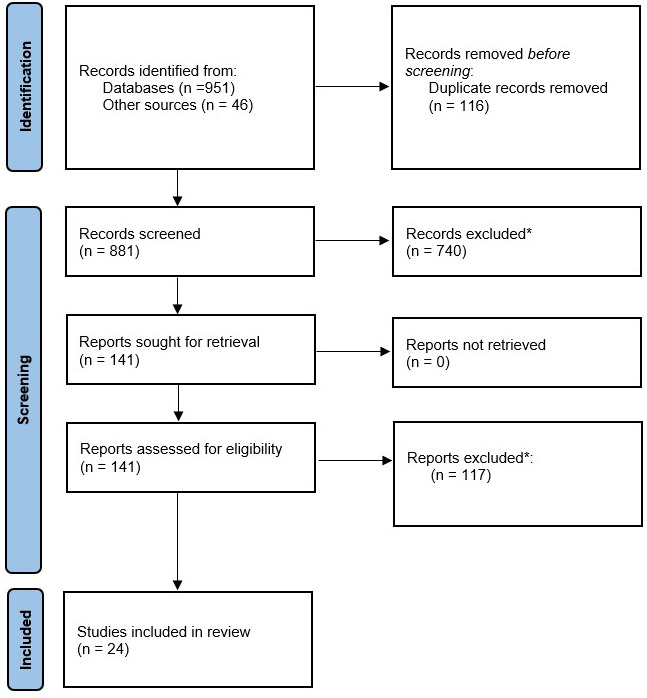
We queried the electronic database from inception through July 2020 using the following keywords: “single stage revision,” “exchange arthroplasty” “periprosthetic infection,” “PJI,” and “single stage.” We initially found 1,000 studies, and after implementing our inclusion/exclusion criteria, as well as any duplicate studies, we ended up with 24 studies in our review. Of these, 14 were Level 3 studies and the remainder were Level 2 and Level 4 studies. We required that each study have a minimum of one-year follow-up. We also only included studies that mentioned demographic data, implant survivorship, and causes of reoperations.
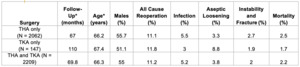
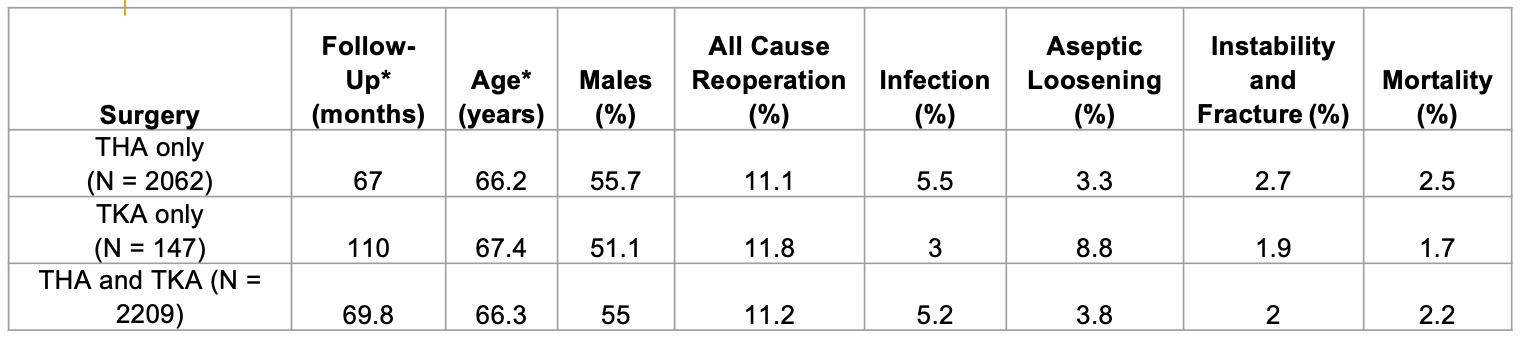
Our research team was able to analyze about 2,200 total hips and total knees in all that underwent a single-stage revision. Roughly 2,000 were total hips and about 150 were total knees. The weighted follow-up time for total hips was approximately five years and for total knees it was approximately 9-10 years.
The Results
We found that the overall all-cause reoperation rate was roughly 11-12% between hips and knees, meaning that the survivorship at 5 or 10 years was close to 90%. The reoperation rate secondary to infection for total hips was 5.5% and for aseptic loosening 3.3%; for total knees it was 3% and 8.8%, respectively. The reoperation rate due instability and fracture was 2-3% and the mortality rate was roughly 2%.
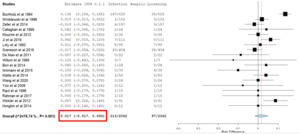
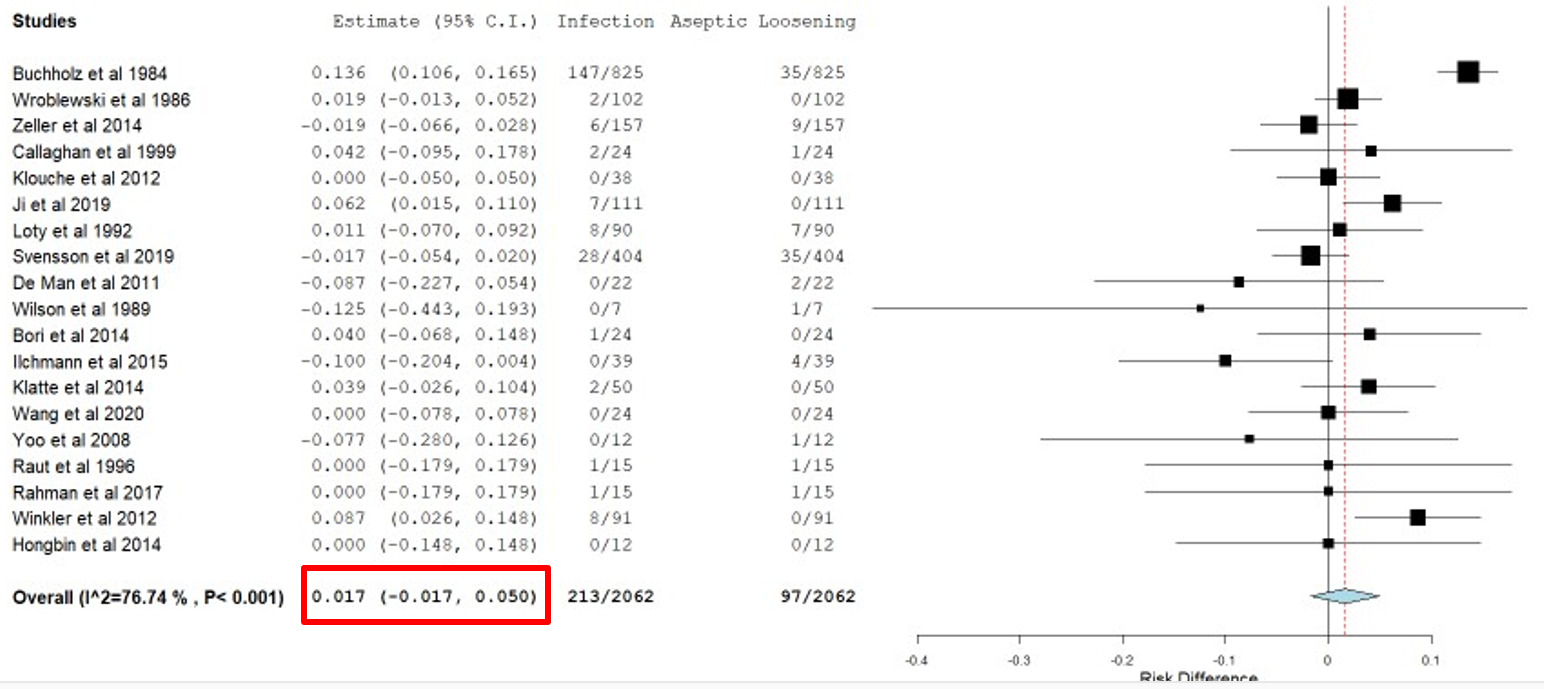
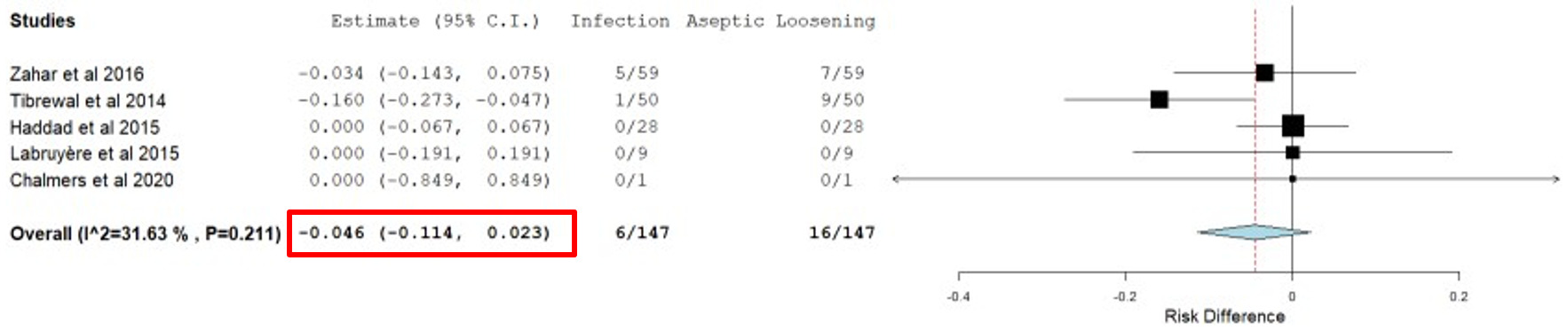
We next sought to determine if there was any statistically significant difference between the reoperation rate from infection and aseptic loosening. Starting with total hips, we constructed a forest plot; the relative risk difference was 1.7% and the 95% confidence interval included 0, so it was not statistically significant. The relative risk difference for TKA was 4.6% and did not reach statistical significance.
We found that following single-stage revision arthroplasty there is high survivorship, close to 90% at 5-10 years and low mortality (around 2%). We found that infection and aseptic loosening were the most common etiologies of revision. Even more importantly, there was no statistically significant difference between these two revision rates, indicating that the infection rates have reduced to the extent that infection and aseptic loosening are equally common causes of revision. Therefore, going forward, it is important that when surgeons consider surgical techniques and improvements, that they not just focus on improving infection rates, but also address aseptic loosening to improve the longevity of these implants.