In this article concerning the correct patient, correct time, and correct surgery, we will attempt to provide the HSS perspective on how we think value-based care can positively impact the way we take care of musculoskeletal patients.
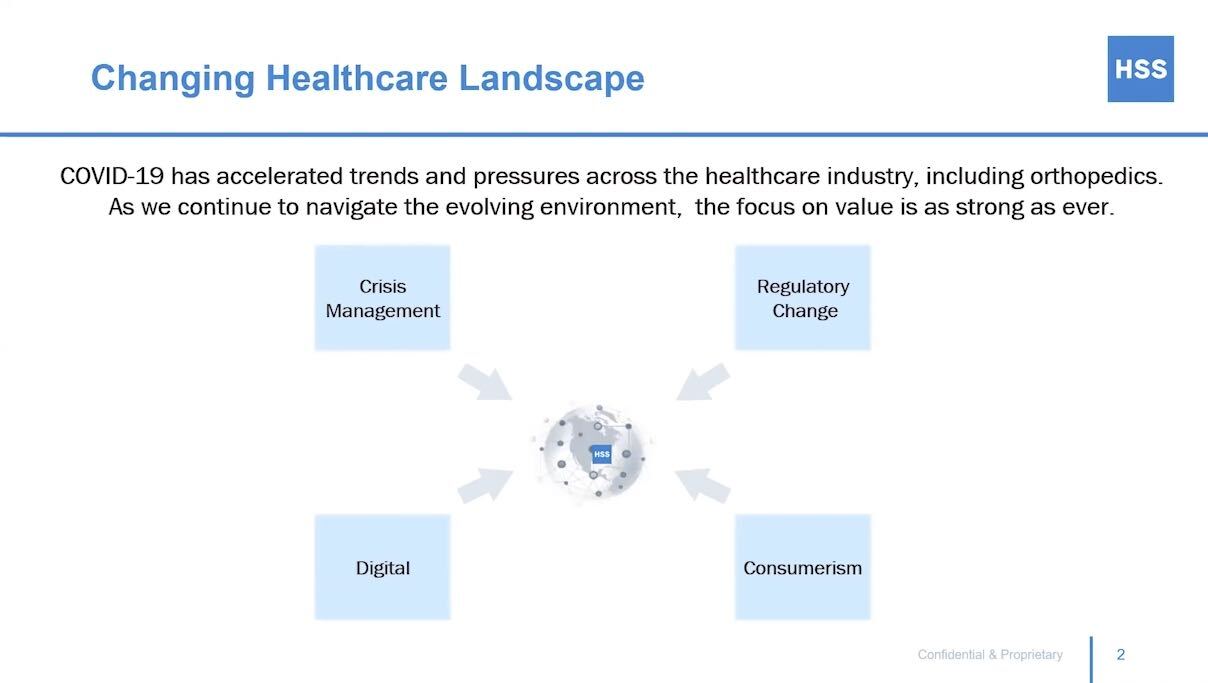
It has been a very interesting 2020, with the impact of COVID-19 on the healthcare system being immense from many different perspectives. We have indeed learned a lot from this crisis, including how to pivot on a dime and change the way we’re addressing things at our institution. Managing this crisis has allowed us to understand some of the trends and pressures across the healthcare industry—including orthopedics. All of this will be useful on the other side of COVID-19 as we aim to provide better care than before.
It is quite a challenging healthcare environment now, whether it’s all the regulatory changes that we are seeing, the advent of transparency in pricing, consumerism, or the importance and recognition of the value of digital platforms to provide patient care and easier access. All of this has been greatly accelerated by COVID-19. With regard to consumerism, we have learned that patients want to have their care brought to them rather than having to come into New York City.
The ability to utilize telemedicine and virtual care accelerated tremendously during the COVID-19 crisis, as we went from doing 1,000 virtual visits a year to almost 150,000 virtual visits—an experience which will ultimately improve the way we provide care to our patients.
Regarding how we apply the concept of value at HSS, we think it’s important to be mission-driven and have a vision and a purpose. The overarching mission for HSS is to make sure that patients are able to resume active lifestyles after injury, recognizing that movement is critical to overall well-being. We like to think that we are helping people live longer, healthier lives with high-quality care. What we have at our disposal here at HSS—being a subspecialty institution—is that we’re singularly focused on musculoskeletal injuries and care, with the foundational pillars of our institution being based on education, academics, teaching, research, and innovation.
This allows us to try and drive the field forward and understand the best and most efficient ways to take care of patients. We have been evolving into an understanding that we really feel the obligation to meet the needs of entire populations. We want to create a musculoskeletal health ecosystem that uses digital platforms to scale the HSS influence and impact across the country.

Looking at traditional metrics of quality is important, but our feeling is that they’re not sufficient and we really need to identify and improve quality measures for patient outcomes. This is critical to improving the value proposition to our patients, whether it’s being an industry leader or using metrics for identifying how we are leading in quality, understanding the culture through Gallup surveys, or using Net Promoter Scores. These are all fine to consider but the fundamental question is, “Are we really providing the highest quality care?”
We have a lot of new initiatives geared toward ensuring that we’re looking beyond the more superficial ways that quality is being evaluated and dictated to us by The Centers for Medicare and Medicaid Services (CMS). The latter include readmissions, mortality, deep vein thrombosis, i.e., the larger problems that can occur after orthopedic surgeries. We are delving deep into patient-reported outcomes, asking, “Are we really getting patients back to the quality and level of function that they desire and that they had before their injuries?” And so quality is a huge aspect of how we’re focusing our initiatives going into the future.

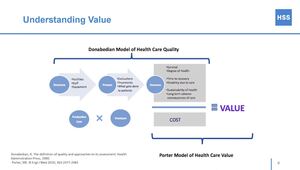
The Association of American Medical Colleges (AAMC) defines value as the quality of a health care service in relation to the total price paid for the service by care purchasers.
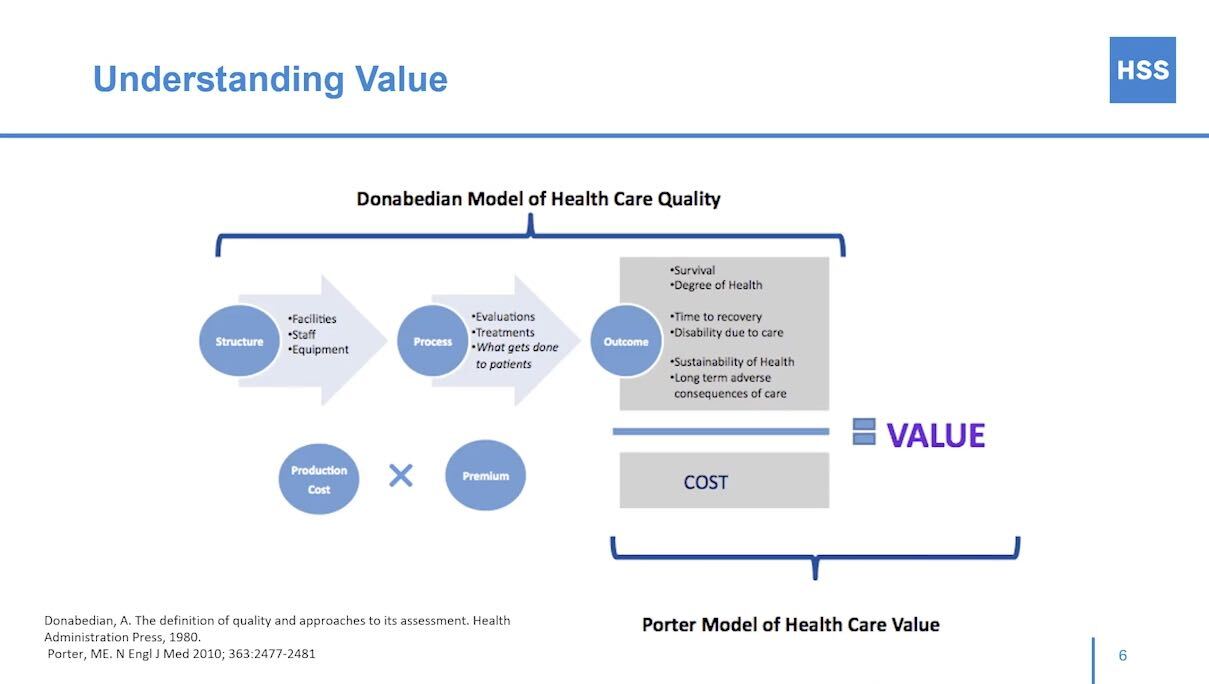
This is a pretty basic understanding of value. There are multiple models of health care quality, but it ends up being quality over cost as far as the determination of what the value is. But how do we determine what quality is? We can look at the structure, the facilities, the staff, the equipment, the process(es) used, how we’re evaluating people, how we’re treating people, what gets done to patients, and how frequently it has to get done, and what are the outcomes. This will give us some measure of quality. The cost is how much—not just per episode but for the entire episode of care—the consumer or the health insurance companies pay for the patient.
I think value can be defined from the patient’s or the purchaser’s perspective, and I think that we have increasing value opportunities. This could be at the unit level, the procedure level, the episode level, an entire condition, or ultimately, by taking a more population-based approach.
We think the highest value in orthopedics is preventative care. If we can reduce the rate of injuries or somehow impact the degree in the severity of osteoarthritis and other types of problems through preventative care, that’s where we are going to find the biggest value. The lowest value care is unneeded or inappropriate care. People getting unnecessary surgeries is a huge waste of the system. So how do we mitigate these problems at a population-based level?
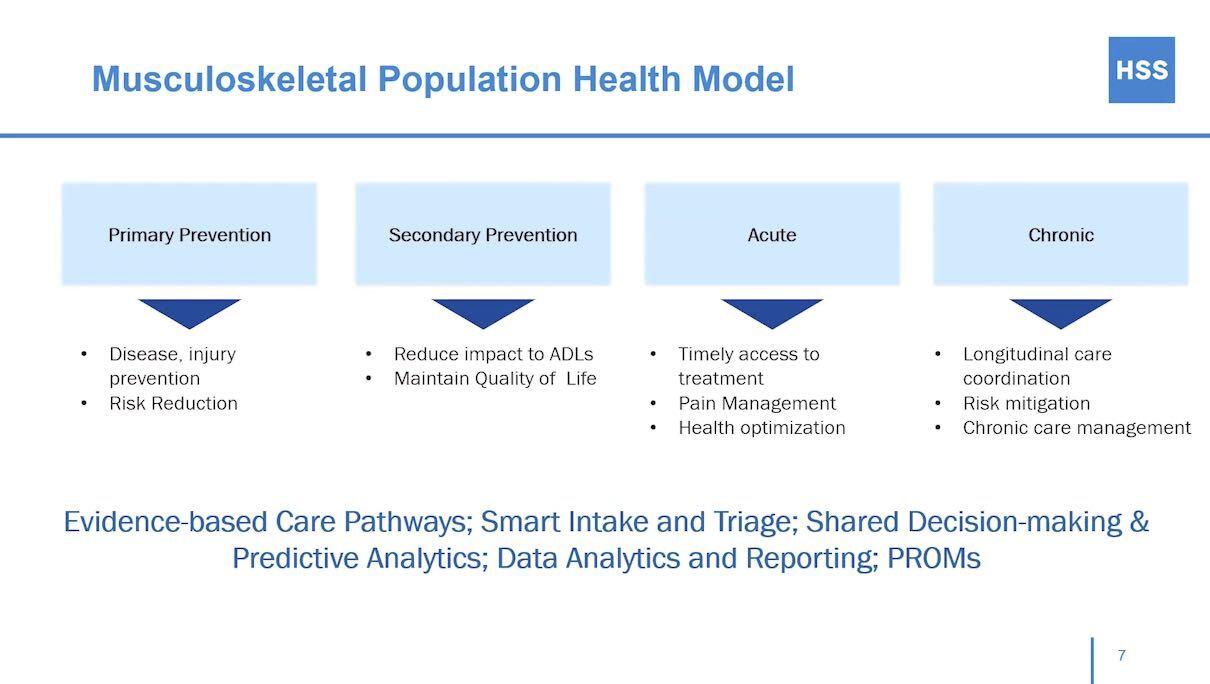
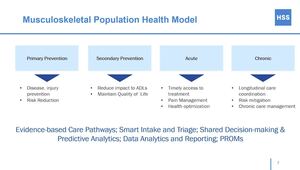
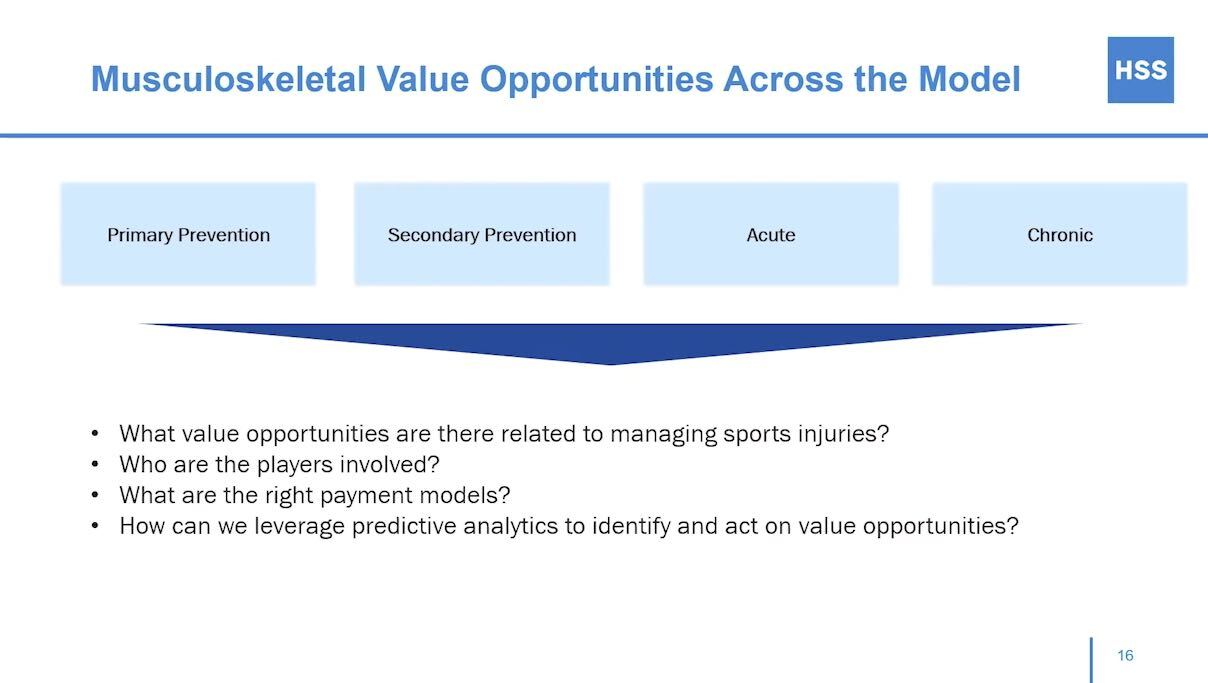
Our perspective on musculoskeletal population health is to look at it as a continuum of care from wellness education to prevention to performance —to identifying injuries early so that they can be treated non-operatively. And in the event that surgery is needed, how can patients be treated in the most efficient manner and how can we “get them back” the quickest? In this continuum of care, we want to think of patients entering the musculoskeletal ecosystem rather than coming in to get fixed and then leaving and us not being able to control what happens after that.
There are four different levels in this continuum of care. The first is primary prevention. One great example of this is anterior cruciate ligament (ACL) tear prevention programs. Research has demonstrated that 50% of ACL tears in females can be prevented using an educational program. So getting this information out and trying to prevent these types of injuries through proper conditioning and training ahead of time is probably where we will find the highest value for musculoskeletal population health.
As for secondary prevention, we are assessing how to treat people so that we reduce the impact of musculoskeletal injuries on their activities and their daily lives and allow them to maintain a high quality of life with high productivity. While we can’t prevent a car accident or some sort of accident that leads to acute musculoskeletal injury, we can make sure that patients get timely access to treatment. We also want to minimize the amount of opioids patients need throughout their recovery, with an overarching goal of optimizing their health. Chronic conditions are the most challenging, but we want to ensure that we have longitudinal care coordination so that there are more efficiencies in the system, and we can mitigate risk and have a chronic care management team in place.
There are evidence-based pathways that allow us to identify patients in each stage of these injury-potential areas via smart intake and triage, shared decision-making, predictive analytics, data analytics, and reporting. Patient-reported outcomes are also important in our efforts to understand how patients are actually faring after they’ve received treatment.
Simply put, the most efficient and the highest value of musculoskeletal care and orthopedics is achieved by identifying the right care at the right time. It’s providing more efficient care and ultimately achieving better outcomes.
You can examine different measures of value and quality through a variety of different metrics, but I still think these are insufficient—there are better ways that we should evolve as far as how we look at these patients and these outcomes.
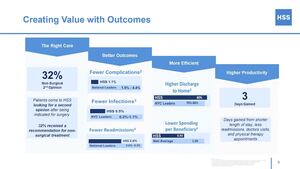
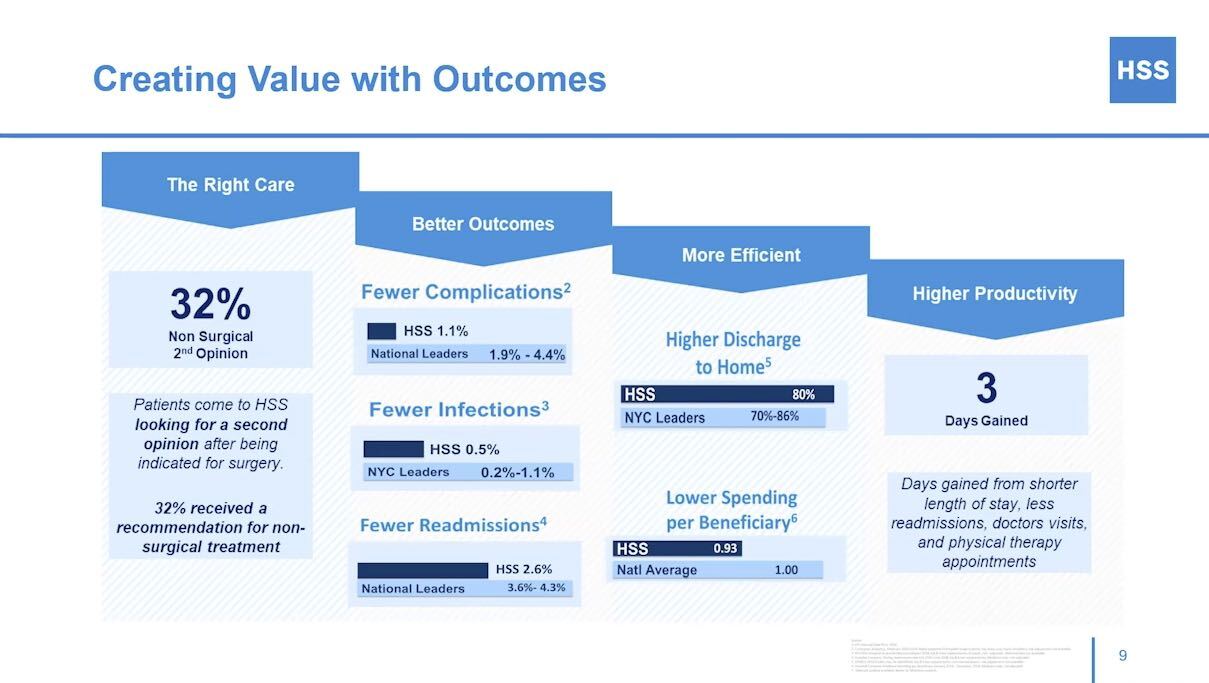
Some examples here in terms of the right care: 32 percent of patients who come to HSS for a second opinion are recommended to not have surgery when they might have been recommended to have surgery at a prior time. This is critical: If we can prevent people from having unnecessary surgeries, then that is as important if not more important than making sure that they have the right surgery when they do need it.
In terms of outcomes, we want to make sure that our complications are fewer, and that infections and readmissions are lower. Again, I think we can look deeper into those quality metrics through more specific quality measures in terms of, “Have they returned to exactly the same level of function they were at before?” and “Are they able to do the things that they want to do to make sure that they’re having a healthy and active life?”
In terms of efficiency, we want shorter hospitalizations, fewer discharges to skilled nursing facilities, higher discharges to home, and increased use of virtual physical therapy for post-op, all while lowering the spending per beneficiary. And ultimately, if we can get patients to the right place, with better outcomes and improved efficiency, then they will be more productive after they recover from their injuries.
The time saved from a shorter length of stay, fewer readmissions, doctor’s visits, and physical therapy appointments can be significant. This is days’ worth of productivity that can be put back into the community and workplaces.
I will delve into each of these three areas to show one way we can think about how we create value by doing the right thing to the right person at the right time.
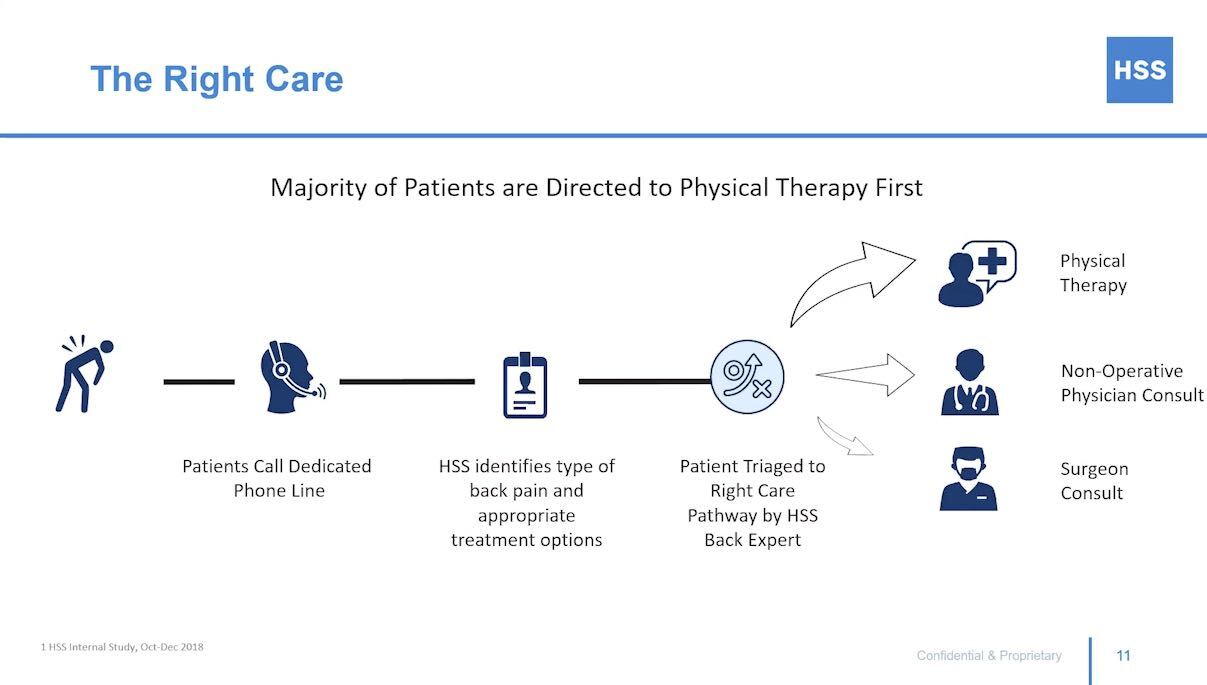
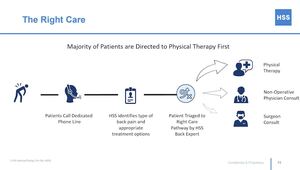
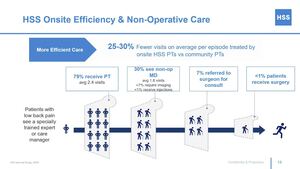
Taking back pain as an example, the majority of patients who seek us out can get triaged appropriately. We don’t want somebody who has had a week of back pain to end up at the surgeon’s office when they don’t need to be there in the first place, thus opening up the possibility of an inappropriate or unnecessary recommendation for surgery.
In our triage systems we identify the types of back pain and make sure that the appropriate treatment options are identified. And then patients are triaged to the right care pathway by the back experts. The majority will go to physical therapy, a certain percentage will go to non-operative physician consults, and then, if necessary, a certain number will go to a surgery consult.
More efficient care will continue with the back pain example.
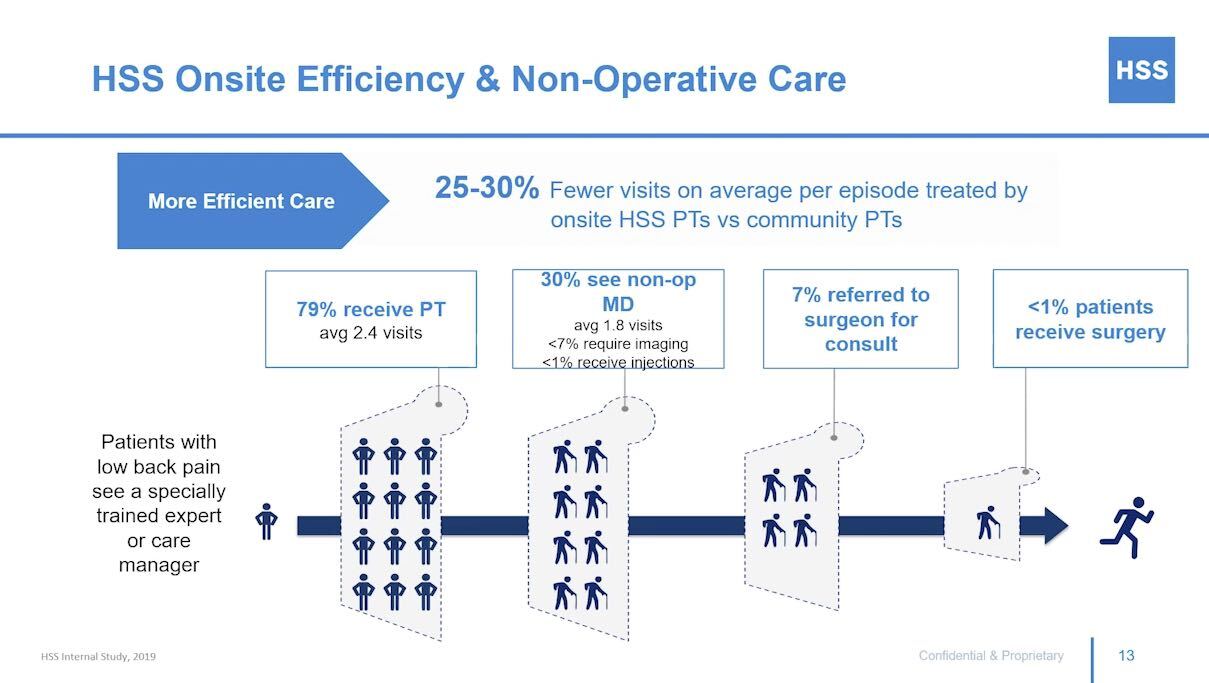
Patients with low back pain will see a specially trained expert or care manager, which may be through a digital platform or could be in person. By ensuring that they go to the right place, we can have 25 to 30% fewer visits on average per episode, treated by on-site HSS physical therapists versus community physical therapists. So 79% of patients who call for back pain will receive physical therapy for an average of 2.4 visits. Thirty percent of these patients will go on to see a non-operative MD. The average number of visits is 1.8. Less than 7% require imaging and less than 1% receive injections. Seven percent of this cohort of back pain patients will end up being referred for a surgical consult and ultimately less than 1% of patients receive surgery. So this is an example of what happens if we can get patients to the right level of care early.
We want to maximize the efficiency of treatment regardless of what “silo” someone is in. Then we can truly streamline the productivity of care, increase the value of the care that’s being provided and reduce the overall health care costs. And we’ll have higher patient satisfaction along the way.
In terms of better outcomes, again, outcomes are critical.
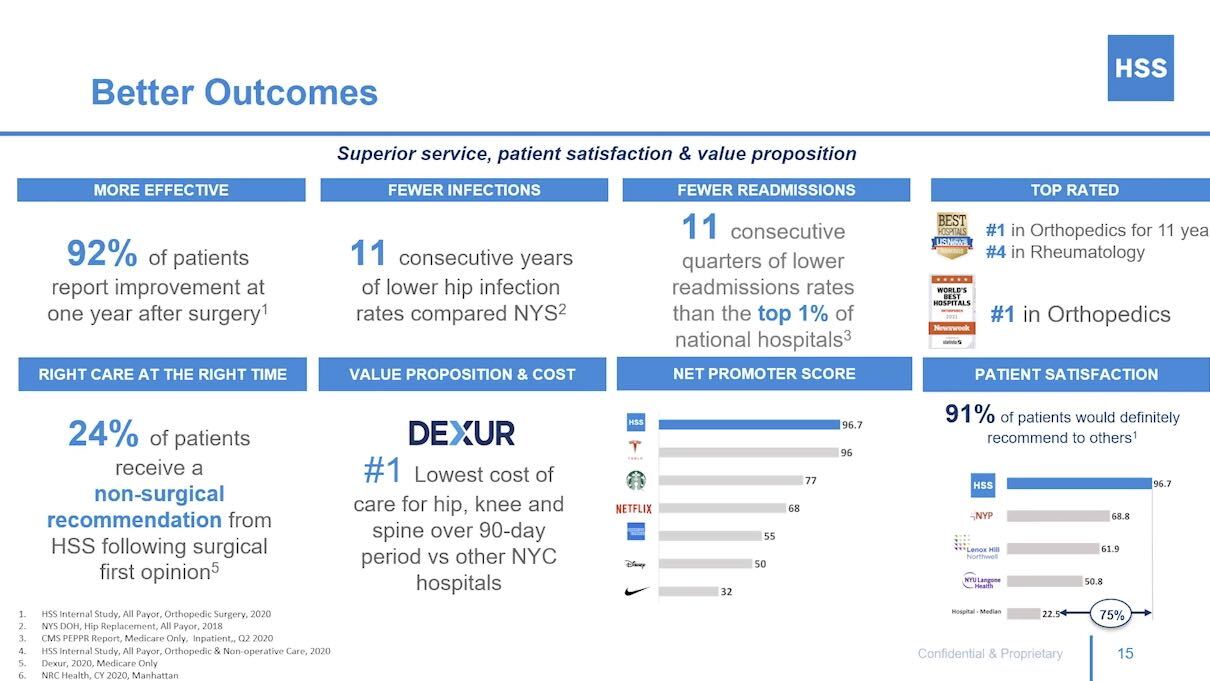
Here are some examples of the things that we look at. First, is the interaction effective? So, we’ll take surgery as an outcome here. Ninety-two percent of patients report improvement one year after surgery. Well, that’s a good number. Does it really capture a true outcome quality metric? As I mentioned before, 24% of patients receive a non-surgical recommendation from HSS following a surgical first opinion. Also, we have closely followed infections as this can be a devastating complication. Making sure that we have the lowest hip infection rates compared to New York state is critical as a definition of a better outcome and quality.
Regarding value proposition and cost, we have the lowest cost of care for hip, knee, and spine over a 90-day period versus other New York City hospitals. So, this is another way where we need to consider not only the single episode of care, but the entire continuum of care over that 90-day period. As for fewer readmissions, we want to make sure that once we discharge someone from the hospital, they don’t need to come back to the hospital for any reason. The Net Promoter Score for the hospital is 96.7%, which is incredibly high for healthcare systems. Rankings and patient satisfaction are all also important ways to look at the quality and better outcomes.
I would continue to argue though that even with these metrics, we can do better—we can find better, more granular ways to identify the quality metrics as to how patients are doing as a result of surgeries. Going forward I think this is going to be a critical component of the value proposition in musculoskeletal care.
There are a lot of opportunities. First, we need to consider musculoskeletal health as a continuous ecosystem from prevention to treatment. We shouldn’t think of ourselves as the car shop where the car gets brought in when it’s broken and then we don’t see it again until it’s broken again. We want to keep patients in the ecosystem so that we can help them out from wellness all the way to injury and illness.
I think there are a lot of questions that we are interested in addressing, some being: What are the value opportunities related to managing sports injuries? Who are the players involved? Who are the people that are most impacted by the decisions that we’re making with regard to how we are distributing care to our patients? What are the right payment models? It’s clear that payment models are evolving. We want to ensure that we can allow as many patients as possible to access our ecosystem, but there are a lot of challenges and barriers to that.
Because data is critical, one of the things we’re working on at HSS is a new center called CAMP, the Center for Analytics Modeling and Performance. CAMP will allow us to consolidate all of the data that we have with regard to outcomes, quality, and efficiencies—and put them in one comprehensive center where we can look at it very carefully and leverage things like predictive analytics, and maybe even block-chain analysis, to help us identify and act on value opportunities.

This was a quick overview of how we at HSS are thinking about the value proposition of orthopedics in the musculoskeletal health care industry. It’s an exciting field to be in right now and we have certainly learned a lot from COVID-19. We have a lot more to learn but our strategic priorities going forward are to continue to deliver the highest quality care and create a system that allows us to identify what value really is. Ultimately, we want to ensure that we are taking care of more patients and more places with better outcomes.