Background
Carpal tunnel syndrome (CTS) is one of the most common neuropathies with an estimated US prevalence of 3-5% (Atroshi et al. 1999). CTS is caused by compression of the median nerve as it travels through the carpal tunnel bounded superiorly by the transverse carpal ligament (TCL) and inferiorly by the carpal bones. The exact mechanism of injury is unclear. The prevailing explanation is that increased intra-carpal pressure from inflammation and scarring of the flexor tendons leads to compression of the microcirculation in the perineurium which then causes nerve ischemia (Amirfeyz, Gozzard, and Leslie 2005; Gelberman et al. 1981). There are several risk factors for CTS, including; increased BMI (Hlebs, Majhenic, and Vidmar 2014; de Krom et al. 1990; Werner et al. 1994), female gender (Atroshi et al. 1999; Stevens et al. 2001, 1988), genetic predisposition (Alford, Weiss, and Akelman 2004; Hakim et al. 2002), pregnancy (Meems et al. 2015), diabetes mellitus (Oktayoglu 2015), and hypothyroidism (Oktayoglu 2015). In addition, occupational exposure requiring highly repetitive manual tasks and hand/arm vibrational work have been identified as independent risk factors (Kozak et al. 2015). CTS is diagnosed through the characteristic symptoms of dull aching pain, paresthesia, and numbness on the thumb, index, and middle fingers. Symptoms are typically worse at night or after use of the hand. Usually, patients will have partial resolution of symptoms if they change hand positions (Dawson 1993). This may be accompanied by a decreased functional status and thenar atrophy; thus the diagnosis can be confirmed with nerve conduction abnormalities.
Conservative management of CTS involves splinting, exercises, oral medications, and corticosteroid injections. While some short-term benefits have been shown for conservative management of mild-moderate CTS (Meems et al. 2014), only surgery has been shown to result in long-term positive effects (Jarvik et al. 2009). Surgical management of CTS succeeds by relieving intra-carpal pressure by transecting the transverse carpal ligament (TCL) (Aroori and Spence 2008). Historically, open carpal tunnel release (OCTR) was considered the gold standard and most reliable procedure for relieving symptoms (Badger et al. 2008). OCTR is typically performed via a longitudinal incision starting from Kaplan’s cardinal line and extended in a curvilinear manner just ulnar to the thenar crease. It is thought that the increased visualization and access to the carpal canal can decrease both the risk of neurovascular injury and the rate of incomplete transection of the carpal tunnel ligament (Steinberg 2002). In recent years, modifications to OCTR and endoscopic techniques have been developed in order to minimize post-operative pain, scarring, and improve recovery times (Sabesan et al. 2012; Nazerani et al. 2014; Atroshi et al. 2006; Cellocco et al. 2005; Tessitore, Schonauer, and Moraci 2004; Elsharif, Papanna, and Helm 2014). The proponents of open procedures often cite higher complication rates and incomplete transection of the TCL as to the reason why they perform the procedure in an open manner (Atroshi et al. 2006). However, when endoscopic releases began to be described, their safety and efficacy was clearly demonstrated (Okutsu et al. 1987; Tsai et al. 1995). Endoscopic techniques have continued to improve, and a recent analysis comparing endoscopic, open, and mini-open procedures showed open and mini-open techniques have near equal efficacy for long-term outcomes compared to traditional OCTR (Sabesan et al. 2012; Nazerani et al. 2014; Elsharif, Papanna, and Helm 2014; Gerritsen et al. 2001; Holmgren and Rabow 1987; Huisstede et al. 2010).
We have been performing a CTS using a mini-open technique that utilizes a pediatric nasal speculum for visualization of the TCL. This study is a 7-year retrospective analysis of our experience with this procedure. The primary goal is to evaluate the short- and long- term safety, efficacy, and aesthetic results of this technique. The secondary goal is to determine if there are any patient specific factors that are associated with positive surgical outcomes. Our hypothesis is that our mini-open technique utilizing a pediatric nasal speculum is safe and provides good outcomes to patients particularly with high scores on the Symptom Severity and Functional Status Scales.
Materials and Methods
Subjects
A retrospective review and telephone follow-up of patients having undergone this procedure was approved by our University’s Institutional Review Board prior to study initiation and all procedures conformed to the ethical guidelines of the 1975 Declaration of Helsinki. Participating patients’ consent was obtained verbally and recoded by members of the study team. Consent and HIPAA notification forms are on file.
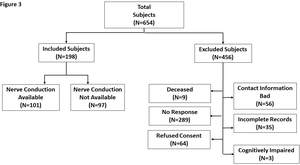
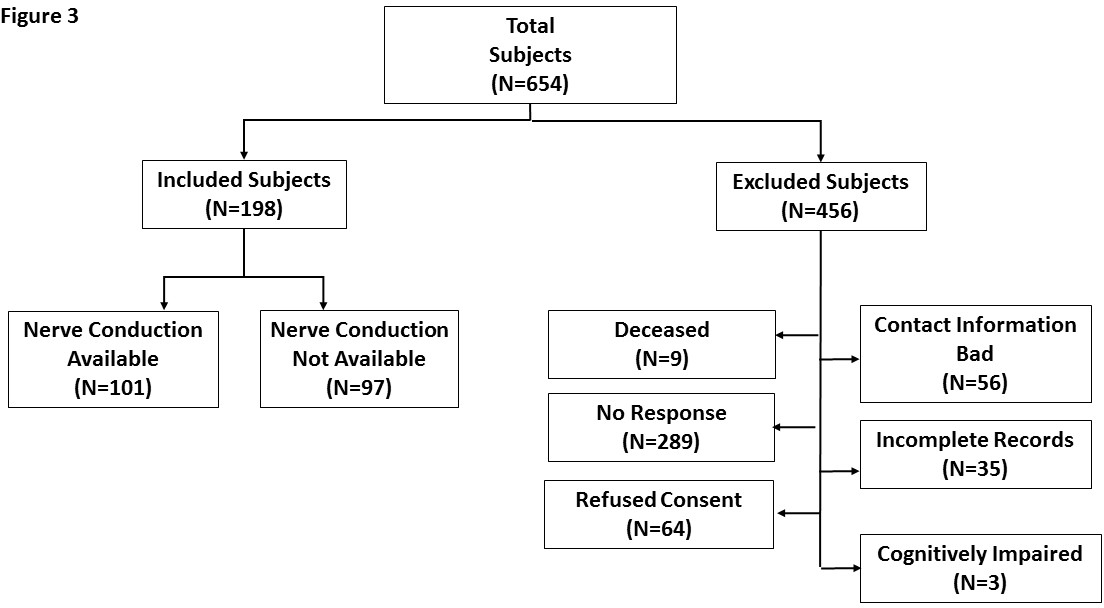
During a six year time-period, a single orthopedic hand surgeon performed mini-open carpal tunnel release surgeries on 654 subjects. Three attempts were made to contact each of the subjects by telephone in order to consent them into the study and interview them. A total of 198 unique subjects were successfully consented to the study (Fig. 3).
Each case had a chart review performed to identify demographics (gender, age, height, weight, race, and dominant hand), comorbidities (hypothyroidism, obesity, pregnancy, diabetes, osteoarthritis, rheumatoid arthritis, and neck, wrist or UE injury), patient history (wake up at night from pain/numbness, pain, numbness, paresthesias, weakness, difficulty with fine motor skills), documented pre-operative Boston Carpal Tunnel Questionnaire, physical exam (light touch, Tinel’s, Compression Test/Durkin’s, thenar atrophy, thenar strength; Atroshi et al. 1999; Amirfeyz, Gozzard, and Leslie 2005; Gelberman et al. 1981; Hlebs, Majhenic, and Vidmar 2014; de Krom et al. 1990), post-operative information (surgery completed, surgical date, surgical complications, release successful), and follow-up findings including pain, numbness, and paresthesia.
During the phone interviews, the patients answered exclusion criteria questions (i.e., trauma to the hand since surgery, stroke affecting limb operated on since surgery, neuropathy other than CTS, cognitive impairment, and nerve injury to the affected hand). They were then asked yes or no questions on whether they still experience pain, numbness/paresthesias, whether the incision was still visible, if the incision was aesthetically pleasing, and if their hand was better or worse since the surgery. Finally, participants were given the Boston Carpal Tunnel Questionnaire to assess their current symptoms compared to the documented preoperative questionnaire in the chart (Levine et al. 1993).
Surgical Procedure
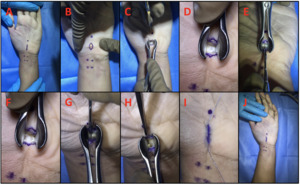
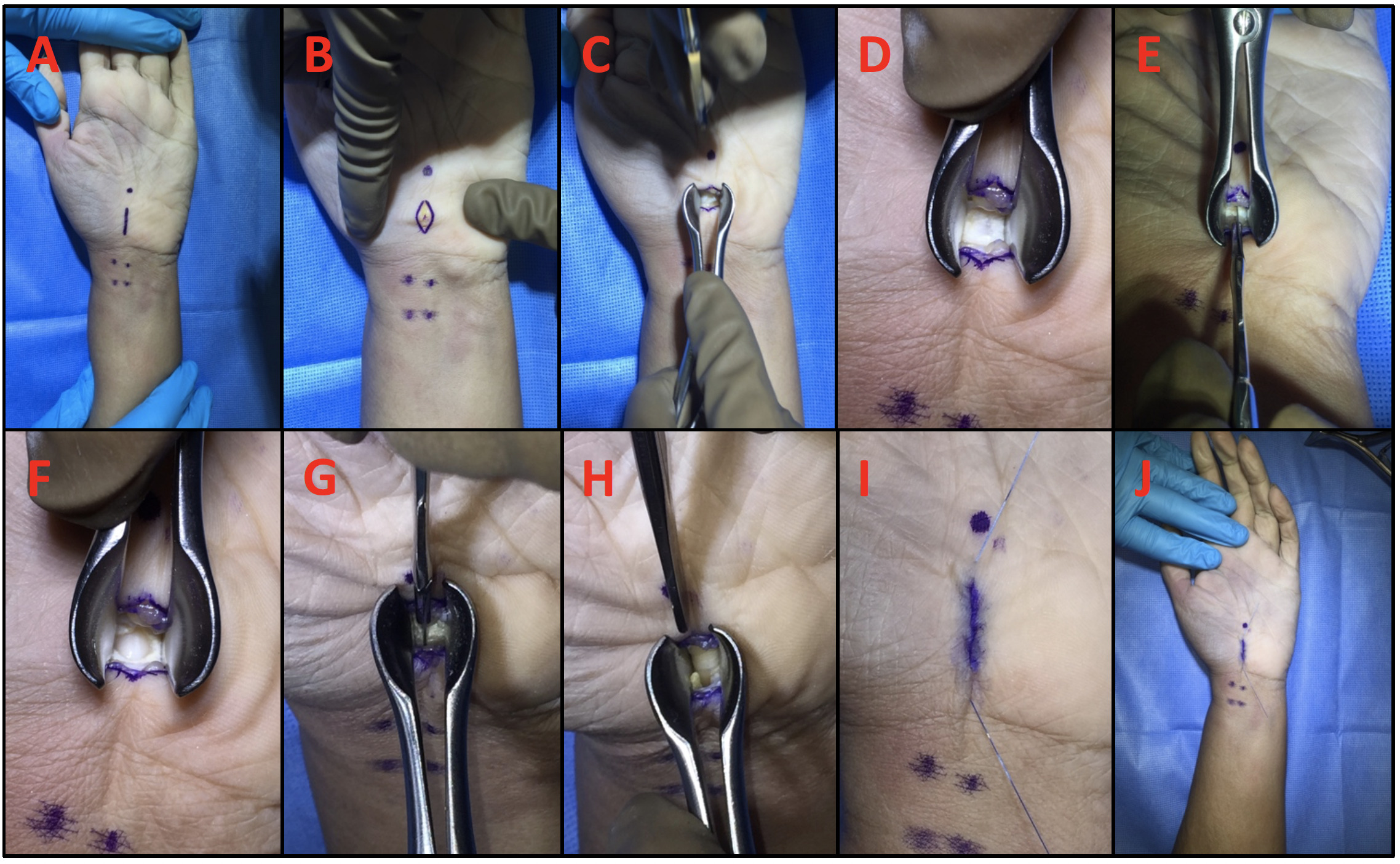
The palmaris longus (PL) and the flexor carpi radialis (FCR) are identified and their locations indicated with a surgical marker (Fig 1A). The superficial palmar arch is identified and marked distally. A ~10mm incision line over the transverse carpal ligament (TCL) is then drawn. The skin is next incised using a #15 blade and then blunt dissected to expose the palmar fascia (Fig1B). A pediatric nasal speculum is then introduced to the incision (Fig 1CD) and a mini-blade (69, Beaver) is used to open the palmar fascia and visualize the TCL (Fig 1EF). The TCL is then released using the Hans Lee CT blade (Fig 1GH) and care is made to release the volar antebrachial fascia. After ensuring complete release, the incision is then closed with poliglecaprone sutures (MONOCRYL, Johnson and Johnson) (Fig 1IJ). The complete set of surgical instruments used in this procedure is shown in Figure 2.
Statistical Analyses
In the multivariable regression analysis, answers to all of the questions from the two questionnaires were re-organized, i.e., the first two of 5 ordinal categories were grouped together as one level, and the rest were re-grouped together as another level. For example, for answers to question 1 of the Symptom Severity Questionnaire, no pain or mild pain were grouped together as not severe pain, and answers for moderate pain to very severe pain were grouped together as severe pain.
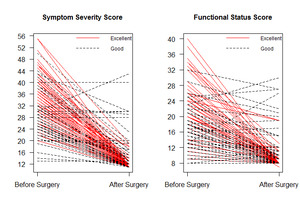
An excellent surgical outcome was defined as having at least a 60% decrease in either the Symptom Severity Scale sum score (SSS) or the Functional Status Scale sum score (FSS) after surgery. All other results were defined as good outcomes. Welch’s T-tests were utilized to compare the continuous variables in the excellent surgical outcome group to the rest. Fisher’s exact tests and Chi-square tests with exact p-values based on the Monte Carlo simulation were utilized to test the association between the excellent surgical outcomes and categorical variables with binary outcomes or multi-level outcomes, respectively. Generalized Estimating Equation (GEE) models were employed to investigate variables associated with excellent surgical outcomes, considering the correlations of observations from the same patients. Exchangeable working correlation matrices proved to be better than the independent or autoregressive working correlation matrices, and were used in all of the GEE models. The associations between excellent surgical outcome and patients’ demographic information, pre-operative measures, SSS, and FSS before surgery were examined one by one in univariate analysis. Then any variables that had a p-value <0.05 in univariate GEE models were further put into a multiple GEE models to study each factor’s association with excellent surgical outcomes after controlling for the rest factors using stepwise selection due to the limited event size (Atroshi et al. 1999). Odds ratios and their corresponding 95% confidence intervals were reported. The c-statistic was calculated to demonstrate the performance of the final predictive model. Statistical significance was set at 0.05 and analysis was done using SAS 9.3 (SAS Institute, Inc., Cary, NC) (Peduzzi et al. 1996).
Results
One hundred ninety-eight cases met study criteria and were included in the analysis. Chart review of demographics and clinic visits found no significant difference in age, pre-operative severity of symptoms as measured in the Boston Carpal Tunnel Questionnaire, and incidences of immediate 3-month postoperative complications, wound breakdown, or pillar pain between the study patients and those who could not be reached by telephone. The mean surgical to interview follow-up time was 4.01 years, mean age at time of surgery was 58 years, 55.7% were female, and 44.3% were male. There were no cases that required revision CTS and all cases had full transection of the transverse carpal ligament without complications. The pre and post-operative SSS scores were 32.17 and 13.08, respectively. The pre and post-operative FSS scores were 20.17 and 9.71, respectively (Table 1). In total, 113 (57%) of the cases met criteria for excellent outcome (Fig. 4).
Using univariate analysis with patients’ demographics and clinical variables separated based upon surgical outcomes, we found that patients’ age at surgery, rheumatoid arthritis, latency at the wrist, latency at the elbow, amplitude at the wrist, amplitude at the elbow, conduction velocity at the elbow, and thenar atrophy were significantly associated with surgical outcomes (all p-values <0.04). In addition, patients with excellent outcomes had longer follow up time (4.24 vs 3.59 years) and younger age (55.29 vs 64.77 years old). Complete patients’ demographics and clinical variables are shown in Table 2.
The surgical outcomes from the Boston Carpal Tunnel Questionnaire are presented in Tables 3 and 4. Pre-operative SSS and FSS scores by surgical outcome initially had 5 answer options and were categorized as either severe or not (Responses to the patient’s answers were categorized as either severe or not severe). Univariate analysis showed that all pre-operative SSS questions and most of pre-operative FSS questions were significantly associated with surgical outcomes.
The odds ratio estimates and the corresponding 95% CI from the fitted multiple GEE model (C-statistic=0.83) are shown in Table 5. The final multiple GEE model included these four variables: gripping a telephone handle before surgery, how long an episode of pain last during daytime before surgery, how severe is numbness or tingling at night before surgery, and difficulty with bathing and dressing before surgery (all p-values <0.03), indicating that these four variables had the strongest association with surgical outcomes. For instance, patients with no severe difficulty in gripping a telephone handle before hand operations had 83.56% lower odds of having excellent surgical outcomes compared to patients with severe difficulty (95% CI: 61.34%-93.01%, p-value <0.01), i.e., patients with severe difficulty in gripping a telephone handle before surgery tended to have a higher chance of achieving excellent improvement.
Discussion
CTS is the most common neuropathy and many surgical techniques have been developed for its treatment (Atroshi et al. 1999). Historically, OCTR was the most reliable procedure for relieving the symptoms of CTS (Badger et al. 2008). However, mini-open and endoscopic procedures have been developed to minimize post-operative pain, scarring and shorter recovery times (Sabesan et al. 2012; Nazerani et al. 2014; Atroshi et al. 2006; Cellocco et al. 2005; Tessitore, Schonauer, and Moraci 2004; Elsharif, Papanna, and Helm 2014). Endoscopic procedures have been criticized for their increased cost due to the need for additional instrumentation along with high rates of vessel injury and incomplete release (Lorgelly et al. 2005). Proponents of the endoscopic approach claim that the shorter recovery time allows for earlier return to work, which cancels out these higher costs (Trumble et al. 2002; Vasiliadis et al. 2014). The nasal speculum assisted approach has the benefit of a single small incision, which gives the same benefits of faster recovery time without the need for expensive instrumentation and training. However, the mini-open approach has been criticized because this procedure does not allow full visualization of the carpal tunnel ligament (CTL) leading to incomplete transections of the CTL and increased complications (Wong et al. 2003). We therefore performed a retrospective analysis to see if this criticism was valid.
In our nasal speculum assisted carpal tunnel release (CTR) study, we had 100% success in transecting the CTL and no operative complications. A similar nasal speculum approach of 101 patients confirms the safety and efficacy of this approach (Muppavarapu et al. 2015). While the major disadvantage of the mini-open technique includes limited visualization, no cases of blood vessel and nerve damage or incomplete transection occurred in order to preserve a small incision site. Mini-open release has been shown to increase the flattening ratio of the median nerve while decreasing pathologic swelling, allowing for fewer wound complications and shorter postoperative pain. In addition, 97.7% of patients reported their mini incisions were aesthetically pleasing and only 78.7% reported their incisions were still visible. However, it is important for surgeons to understand the difficulty of inserting the nasal speculum into a small incision site while avoiding damage to the median nerve.
Prior studies have found poor surgical outcomes with high Boston pre-operative scores, delay of surgery, and poor EMG results (Rege and Sher 2001; Aksekili, Bicici, Isik, et al. 2015). However, no study has ever analyzed all the pre-operative risk factors and symptoms associated with good surgical outcomes. Through this study, we found that only four questions are needed to predict whether the patient would have a good surgical outcome or not. While previous studies have reported improved objective measurements of sensation, pinch, and grip strength using nasal instrumentation, our study focuses on subjective evaluation, which may more accurately reflect functional improvements as judged by the patient (Sever et al. 2010; Karnezis and Fragkiadakis 2002). As seen in our results, patients with more severe preoperative symptom severity had a higher likelihood of excellent surgical outcome compared with patients with less severe symptoms. These results may reflect the idea that patients with more severe preoperative symptoms may experience greater improved physical and emotional changes postoperatively not always correlated with motor tests.
The reliability of clinical signs, motor tests, outcome questionnaires, and electrophysiological studies for outcome measures after CTS surgery remains unknown. Past studies have shown severity scoring using the Boston Questionnaire to be predictive of outcome measures and in identifying patients likely to respond to surgery (Yucel and Seyithanoglu 2015). Improvements in Boston Questionnaire scores correlate with a decrease in the carpal tunnel inlet cross sectional area suggesting reduced pathologic swelling and perceived symptom severity are associated (Oh et al. 2017). While most aspects of symptom severity and functional status were associated with excellent outcomes on univariate analysis, our fitted multiple GEE model predicted duration of pain episode and severity of numbness or tingling at night to be symptoms most predictive of surgical outcome. Routine daily activities, such as gripping a telephone handle, bathing, and dressing were functional measures that if severely impaired would be predictive of favorable postoperative results. Compared to other components of the functional status scale, telephone gripping and bathing are daily routine tasks where improved limitation and discomfort is most noticeable on follow up. It is important for surgeons to be aware of demographic, history, and physical exam components associated with excellent surgical outcomes in order to communicate appropriate expectations and return to functioning with patients. Clinicians should consider mini-open incision as a safe, satisfactory procedure in patients with CTS coming to clinic who present with severe pain, prolonged daytime numbness, and inability to bathe and use the telephone.
Because this study is a retrospective case series, limitations include prolonged mean follow-up time and recall bias. Patient reported outcomes measurements are subject to recall bias as prior studies have found retrospective subjective outcomes produce more favorable results than prospectively monitored health status data (Gotlin et al. 2019). Review of literature suggests many subjective outcomes after CTS are similar three months postoperatively (Wong et al. 2003). However, the excellent surgical outcomes recorded from our mean time to follow up of 4.08 years may be explained by expected symptom relief from extended recovery from natural healing processes. Many subjects were excluded due to no responses on telephone interview attempts, thus limiting our study to selection bias. Finally, from a surgical technique perspective, the insertion of the nasal speculum into the carpal tunnel is challenging and makes for further tunnel exploration and synovectomy difficult.
Conclusion
Overall, this study provides evidence that surgeons should consider nasal-speculum assisted mini-open carpal tunnel release as a safe, satisfactory procedure in patients presenting with CTS. Patients with more severe preoperative symptom severity had a higher likelihood of excellent surgical outcome compared with patients with less severe symptoms. Duration and severity of pain episodes along with difficulties in bathing and gripping a telephone were found to be most predictive of improved subjective evaluation. As healthcare economics prioritizes patient satisfaction outcomes, it is important for surgeons to consider this mini-open technique as a way for patients with difficulties in routine daily activities to experience improved self-reported assessments, which may more closely reflect functional improvements as judged by the patient.
List of Abbreviations
CTR: Carpal Tunnel Release
CTS: Carpal Tunnel Syndrome
CTL: Carpal Tunnel Ligament
GEE: Generalized Estimating Equation
EMG: Electromyography
OCTR: Open Carpal Tunnel Release
SSS: Symptom Severity Scale
FSS: Functional Status Scale
TCL: Transverse Carpal Ligament
Ethics approval and consent to participate
A retrospective review and telephone follow-up of patients having undergone this procedure was approved by our University’s Institutional Review Board prior to study initiation and all procedures conformed to the ethical guidelines of the 1975 Declaration of Helsinki.
Consent for publication
Participating patients’ consents were obtained verbally and recoded by members of the study team. Consent and HIPAA notification forms are on file.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Competing Interests
The authors declare that they have no competing interests.
Funding
The authors report no external funding for this study.