Introduction
In January of 2020, Washington State became the initial epicenter of COVID-19 in the United States (Bedford et al. 2020). Within weeks after the first COVID-19 case was diagnosed in Snohomish County, it was discovered that the virus was spreading in different communities across Washington.
The increase in cases led to different government restrictions, including limitations on surgical procedures. On March 19th, 2020, all elective surgical procedures were cancelled to maintain the safety of patients, providers, and the community at large (Inslee 2020). Hospitals also needed to preserve resources for COVID-19 patients by keeping intensive care unit beds open and minimizing the amount of personal protective equipment (PPE) used. As a result of these restrictions, patients seeking elective hip and knee replacement surgery had to cancel or postpone their procedures. In addition, patients’ postoperative care was disrupted by limited access to clinics, physical therapy, and crowded emergency rooms (Bert, Hooper, and Moen 2017). Telemedicine and other substitutes became standard for these patients (Demeke et al. 2021).
Before 2015, less than 1% of total joint replacements were done as outpatients. Recent advances in surgical techniques, pain management, expedited rehabilitation protocols and cloud-based homecare solutions now allow for TJAs to be performed safely in the outpatient setting. 25% of today’s total joint surgeries are performed on an ambulatory basis, and that figure is expected to exceed 60% in the future (Bert, Hooper, and Moen 2017; Olderog 2019).
Some of the interest in ambulatory joint replacement has been fueled by the opportunity to conserve expensive hospital resources and the potential to avoid hospital-acquired complications. Until recently, inpatient stays and transfers to skilled nursing facilities were standard practice after joint replacement. In this setting, it was reasonable to cease elective joint replacement due to the COVID-19 pandemic. However, the widespread cancellation of elective joint replacements resulted in patients experiencing prolonged pain and debilitating arthritis with limited access to surgical teams, physical therapists, and other providers. It also resulted in furloughed clinical staff and considerable financial hardships in orthopedic practices, leading surgeons to adjust their practice to more outpatient settings. Nevertheless, there is a lack of knowledge regarding the safety of TJA even in an outpatient setting during the COVID-19 pandemic.
This paper investigates a dedicated early recovery protocol, cloud-based homecare, and the use of patient-reported outcomes (PROMs) to assess the outcomes of a group of patients in Washington State who underwent elective joint replacement during the initial surge of COVID-19. This study aims to gain insight into the safety of elective TJA during an active pandemic and to help validate a future study design that will combine PROMs with clinical outcomes.
Methods
Patients who underwent hip and knee arthroplasty in Washington State during the initial surge of COVID-19 between January 19th, 2020 and March 19th, 2020, were included in this retrospective case series study. A total of 14 surgeons in Washington State experienced with outpatient techniques, opiate-sparing pain management, and early discharge to home after hip and knee replacement conducted surgeries. These surgeons carried out all surgeries within Washington State facilities, either at an ambulatory surgery center (ASC) or a hospital. Patients were not recruited for these surgeries but were approved for surgery by their surgeon based on debilitating arthritis that limited their activities of daily living.
All patients registered for and participated in joint camps which utilized a standardized platform (The SwiftPath Program, LLC) for patient engagement, risk stratification, discharge planning, and homecare monitoring. This patient engagement platform included written materials, an online joint camp, multimedia videos and interactive tasks. Patient engagement and family involvement were verified with checklists and attestations. The patient experience included shared-decision-making focusing on knowledge of the procedure and the skills needed for at-home postoperative care. Patients were asked to complete a proprietary risk stratification algorithm that aided in decisions about site of care, discharge planning and homecare interventions. The algorithm uses predictive modeling and was derived from a series of evidence-based roundtable sessions using the Delphi Method with hundreds of high-volume joint replacement surgeons and other subject matter experts. In addition to screening for medical problems and co-morbidities, the algorithm quantifies patient motivation, beliefs and values, psychological issues, family engagement, physical capabilities, and home setup. In doing so, the algorithm allows for risk stratification by calculating a “pathway score” which helps surgeons decide if ambulatory surgery is appropriate. Scores range from less than 20 (outpatient surgery is ill-advised), 20-25 (consider optimization before surgery), 25-30 (outpatient surgery based on surgeon discretion), 30-35 (ideal outpatient candidate).
Postoperatively, surgeon specific notifications prompted patients to complete real-time home care and pain management assessments with opiate tracking on post operative days 0, 1, 2 and 3. Real-time alerts with preset thresholds allowed the care team to respond to patient needs “on-queue.” Home care monitoring focused on the first 3 to 4 days after surgery. Telehealth, home monitoring tools, cloud-based reporting, and alerts were used in place of traditional inpatient resources.
Patients were asked to respond to standardized PRO questionnaires. These PROMs included: HOOS JR., KOOS JR., Patient-Reported Outcomes Measurement Information System (PROMIS), as well as patient satisfaction surveys that focused on complications, readmissions, ER visits, and questions involving postoperative pain.
Patients were followed from baseline to routine post-op intervals out to 6 weeks. A follow-up “COVID-19 survey” was also sent to patients through the online platform to determine the impact of COVID-19 on ambulatory hip and knee replacements (Table 1). All responses received from the questionnaires and surveys were stored on a HIPAA-secure cloud server and were later assessed after patient health information was deidentified. Statistical analysis was not performed due to the limited amount of PROMs and survey responses received postoperatively.
Results
Of the 282 patients who were included in the study, 254 (90%) registered and had partially completed questionnaires on the online platform. The average age of the patient cohort was 67.7 years old (range 30 – 91). Of the 254 patients registered on the platform, 166 (65.4%) were knee joint replacements, and 88 (34.6%) were hip joint replacements.
Sixty patients responded on the platform stating they had their joint replacement operation at an ASC, and of these 60 patients, their average Pathway Score was 28.4. One hundred eighty-seven patients responded on the platform stating they underwent their joint replacement operation at a hospital, and of these patients, their average Pathway Score was 25.6. Seven patients out of 282 (2.48%) did not respond to whether they had surgery in a hospital or ASC setting.
Furthermore, of the 166 patients undergoing total knee arthroplasty (TKA) and who specified their surgical location (ASC vs Hospital), 36 stated they had their surgery performed in a hospital. In total, their average length of stay was 1.24 days. In addition, 36 patients stated they underwent their TKA in an ASC (Figure 1). Of the 72 patients who underwent TKA and responded to the questionnaires on the platform, there were five documented visits to the emergency room postoperatively: three hospital patients and two ASC patients.
Similarly, of the 88 patients who underwent total hip arthroplasty (THA) and specified their surgical location, 40 responded stating they had their surgery at a hospital (Figure 1). Their average length of stay was 1.25 days. Eight patients responded that they had their THA in an ASC. Of the 48 patients who underwent THA and answered on the platform, zero reported any emergency room visits.
Hospital readmission postoperatively included two TKA and no THA patients. However, twelve patients did not respond to whether they were readmitted to the hospital or not.
A total of 72 patients out of 282 (25.5%) completed the HOOS JR. and KOOS JR. questionnaires both preoperatively and postoperatively, and each patient had improved scores by six weeks post-operation. Patients’ HOOS JR. and KOOS JR. scores did not vary based on their inpatient or outpatient status (Table 2). Of the 166 patients who underwent TKA, 154 responded to the preoperative questionnaire but only 48 went on to complete the postoperative questionnaire. Out of the 88 patients undergoing THA, 83 responded to the preoperative questionnaire and 24 completed the postoperative questionnaire (Table 2).
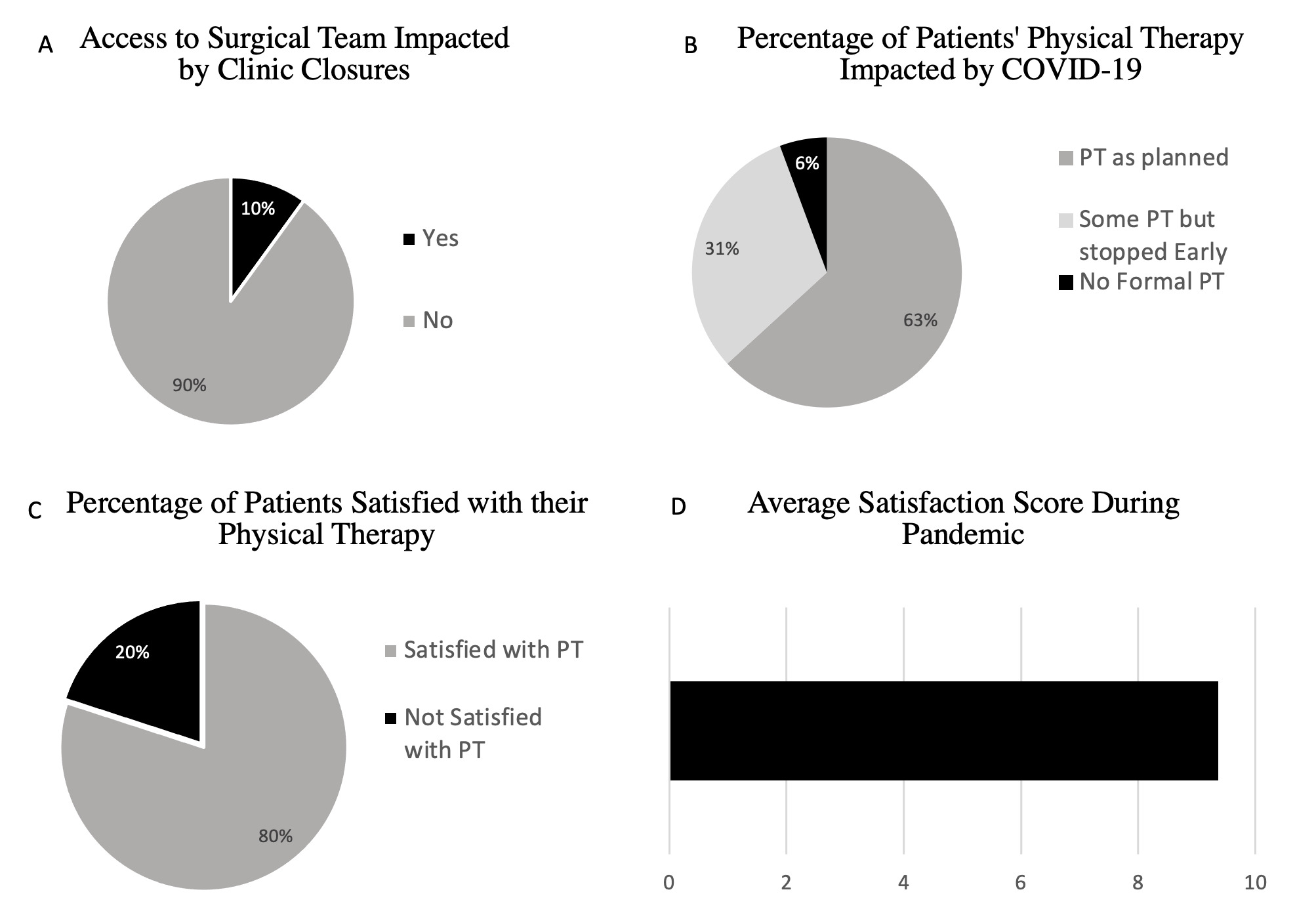
One hundred eighty patients responded to the COVID-19 survey sent out postoperatively through the online platform. No patients reported viral symptoms or developed COVID-19. However, 33% of patients reported stopping their physical therapy (PT) early, with 5% not receiving any PT due to the pandemic. Of the patients that did participate in formal PT, 20% were not satisfied with the PT care they had received (Figure 2B, Figure 2C). The average surgery satisfaction score during the COVID-19 pandemic was 9.31/10 (Figure 2D). The average postoperative pain score from postoperative days 0, 1, 2 and 3 was 4.10/10.0.
Discussion
The COVID-19 pandemic has placed substantial constraints on elective procedures, including TJA. Many patients had their surgeries cancelled or postponed and were left with painful and debilitating arthritis. Patient demand paired with a global pandemic further necessitates the significant need for care redesign, especially since it is unclear when the COVID-19 pandemic will end and when another might begin. Facilities and providers face the challenges of safely performing elective surgery, preserving resources, and minimizing risk. By utilizing an established online platform where patients can respond to clinical questionnaires and report their outcomes of ambulatory joint replacement surgery, we were able to gain some insight into the safety of TJA during an active COVID-19 pandemic and further improve cloud-based monitoring.
A number of studies have examined demographics and medical comorbidities, including sex, age, American Society of Anesthesiologists score, and cardiac risk factors, to develop checklists for patient selection for outpatient joint replacement (OJR) to reduce risks and optimize outcomes (Sibia, King, and MacDonald 2017; Berger, Cross, and Sanders 2016). However, for OJR to be successful and to prevent unplanned hospital stays (i.e. failure to launch), patient selection must go beyond checklists; tools that reliably predict which patients will be able to go home on the day of surgery are needed (Feder et al. 2020; Meneghini et al. 2017; McAllister et al. 2015). To reliably prevent hospital admission, psychological issues, anxiety, and physical capabilities should also be measured (Pearson, Moraw, and Maddern 2000; Riddle, Jiranek, and Hayes 2014; Courtney, Boniello, and Berger 2017).
Complications occur in roughly 4% of primary joint replacements, with most occurring in the first 3-4 days (Pulido et al. 2008). Concern about early complications continues as a justification for inpatient stays, daily labs, nursing, and hospitalist care following TJA. Although complication rates are low when patients are appropriately selected and are discharged home, there remains a need for alternative methods for postoperative surveillance and prevention of complications in the setting of OJR. What monitoring is needed can, for the most part, be accomplished with digital technology and nurse navigator models. Telehealth follow-up care after surgery can easily be coordinated with labs, clinical assessments, and in-home services—all done safely on an outpatient basis.
However, this study highlights the importance of assuring patients have appropriate access to PT if they are going to undergo surgery during a pandemic, as 20% of survey responders were not satisfied with the PT they had received. In addition, 33% reported limited PT access, with 6% not receiving any PT due to the pandemic (Figure 2B). If joint replacements continue throughout the pandemic, it is essential that PT is accessible.
Although patients underwent surgery during the pandemic, this study demonstrated that patients were still satisfied that they had surgery, given the average pandemic satisfaction score of 9.31/10 (Figure 2D). This highlights the debilitating nature of osteoarthritis, which can heavily impact patients’ quality of life and motivate patients to pursue surgery regardless of the pandemic status. Brown et al. found that almost 90% of patients undergoing TJA who had their procedure cancelled due to COVID-19 planned to reschedule as soon as possible (Brown et al. 2020).
This study found that no patient who responded to the COVID-19 survey had developed viral symptoms. However, the main limitation of this study is that we did not achieve an adequate response rate through the online platform. Several patients only partially completed the data, and some did not respond at all. The COVID-19 survey was only completed by 63% of patients who had registered on the platform. Therefore, the status of the other 37% of patients is unknown. Given the lack of data, we are unable to draw any direct conclusions from this study regarding the safety of outpatient joint replacement surgery during the COVID-19 pandemic. Nevertheless, the primary purpose of this study was to gather data to help us validate a study design that would enable us to more adequately investigate the safety of ambulatory joint replacements during an active pandemic.
Although HOOS JR. and KOOS JR. from preop to 6 weeks post-op followed our expectations of improved disability after surgery, the limited response rate to questionnaires prevented us from obtaining any statistical results. Of the data available, there was no apparent difference seen in the disability outcomes of patients who had surgery in the hospital compared with an ASC. However, there are clear advantages of getting surgery in an ASC versus a hospital, especially in the setting of COVID-19, where the risk of virus transmission is likely higher. Zhou et al. found that in the early COVID-19 outbreak in China, 44% of 179 COVID-19 patients in the hospital had nosocomial acquired infections (Zhou et al. 2020; Richterman, Meyerowitz, and Cevik 2020). Thus, having surgery in an ASC where there are fewer medically complex patients and less patient volume is theoretically safer in terms of viral transmission and also preserves hospital resources.
Additionally, there are many pertinent examples of proper implementation of ASCs for elective surgeries that can be taken from the Severe Acute Respiratory Syndrome (SARS) outbreak in 2002-2004. Researchers in Singapore and Hong Kong during the SARS outbreak found ACSs to be highly effective in providing essential surgical care while also minimizing patient risk from viral transmission and conserving hospital resources (Gilat et al. 2020). Thus, performing surgeries in an ASC during an active pandemic is likely a step in the right direction and may be safer for patients and potentially reduces operating costs.
The percentage of elective outpatient TJA in the orthopaedic community has increased in popularity, primarily since they have been associated with fewer complications postoperatively and higher patient satisfaction scores (Kelly et al. 2018). As surgeons and patients question the safety of surgeries in the hospital during an active pandemic, it is likely that COVID-19 will catalyze the growth of ASCs even further.
However, in order to have an effective outpatient program, substantial patient education is required to produce quality patient outcomes. This involves joint camps to enable patient engagement as well as shared decision making that is measured, validated, and operationalized throughout the episode of care. Studies confirm that patients who participate in shared decision making choose less invasive procedures, fewer medications, and have better overall results (Marinker 2003; Elwyn et al. 2012). When this is combined with the use of an online platform that provides multimedia access to written content, quizzes, checklists, informative videos, and the ability to report outcomes postoperatively, patient care and safety are positively impacted.
Although this study used an online platform to gather data regarding elective surgeries during COVID-19, there were limitations, as mentioned previously, that prevented us from drawing meaningful conclusions. Nevertheless, our study provides insight into some of the benefits of OJR surgery in the setting of an active pandemic. Further investigation with a redesigned study to more adequately explore the safety of elective surgeries during COVID-19 is needed.
Conclusion
An online patient engagement platform can help monitor the clinical course, PROMs as well as any virus-related illnesses in patients undergoing TJA. Information from PROMs can be used to evaluate outcomes during a pandemic. To continue to care for our patients, who often have debilitating hip or knee osteoarthritis, we need to determine the safety of performing elective surgery during the pandemic and keep our patients’ best interests as a top priority.
Acknowledgments
Craig McAllister MD has ownership in The SwiftPath Program, LLC and serves as its Chief Medical Officer.
IRB
This study was reviewed by Washington State University IRB and deemed exempt.