- Comparing Outcomes of Anterior versus Posterior Shoulder Instability: A Systematic Review and Meta-Analysis
- Failure of Liposomal Bupivacaine in Managing Postoperative Pain Following Shoulder Surgery
- Epidemiology of Ankle Sprain in the Military: A Systematic Review of Literature
- Grade 3/4 Chondromalacia of the Hip: Is Microfracture Worth It?
- Review of Rehabilitation Protocols Designated for Meniscal Repairs: A Systematic Review and Analysis
- Effects of Complete A4 Pulley Release on Bowstringing of FDP tendons in a Cadaveric Model
- Biologic Graft Augmentation for Glenoid Bone Loss in Revision Reverse Shoulder Arthroplasty (rTSA)
- Better Outcomes? Rotator Cuff Repair versus Reverse Shoulder Arthroplasty for Massive Rotator Cuff Tears in Elderly Population
- The Role of Preoperative Magnetic Resonance Imaging (MRI) in Surgical Decision Making for Total versus Medial Unicompartmental Knee Arthroplasty
- Psychological Burnout and Age of Sport Specialization: A Profile for Current NCAA Big 12 Student-Athletes
- Major and Minor Complications in Patients with Generalized Anxiety Disorder Undergoing Single-Level Anterior Cervical Discectomy and Fusion
- The Influence of Pharmacological Osteoporosis Treatment on Refractures Following Kyphoplasty
- How Should PROMs Be Used? The Development of Quality Measures for Using Patient Reported Outcome Measures in Hand Surgery
- Treatment of Severe Ankle and Hindfoot Deformity: Technique Using Femoral Head Allograft for Tibiotalocalcaneal Fusion Using a Cup and Cone Reamer
- Determinants of Physical Therapy Utilization Following Shoulder Surgery: A Retrospective Review
- Sex Related Outcomes Following Anterior Cruciate Ligament Reconstruction (ACLR): A Systematic Review and Meta-Analysis
- Ambulatory Hip and Knee Replacement Outcomes During COVID Outbreak in Washington State
- The Effectiveness of Bedside Low Pressure Irrigation on Pistol Caliber Gun Shot Wounds Bacterial Contamination
- Health Literacy in English vs. Spanish-Speaking Orthopaedic Chronic Pain Patients in a Closed Urban Setting
- Characterizing Comorbidities in Total Joint Arthroplasty Patients in a Safety-Net Hospital Using the Age-Adjusted Charlson Comorbidity Index
- Stemless Anatomic Total Shoulder Arthroplasty with an Inlay Glenoid: Analysis of 90-Day and 2-Year Complications
- Implementation of an Injury Prevention Program in NCAA Division I Athletics Reduces Injury-Related Healthcare Costs
- Post-operative advantages of use of tranexamic acid combined with local anesthesia at graft site in single bundle arthroscopic anterior cruciate ligament reconstruction
- Clinical Outcomes of Primary versus Revision Surgery using Arthroscopic Anatomic Glenoid Reconstruction for Anterior Shoulder Instability
- An Alternative 1-stage Exchange Arthroplasty Technique: for the Chronic Infected Total Hip
- Calculating Glenoid Bone Loss Based on Glenoid Height Using Ipsilateral 3-Dimensional Computed Tomography
- MPFL Graft Tensioning to Treat Patellar Instability Related to Patella Alta: Dynamic Simulation
- What is Driving Increased Numbers of Applications in the Orthopaedic Surgery Match and What are Applicant Opinions of the Process – An Anonymous Survey of 4th Year Applicants
- Onlay versus Inlay Prosthesis for Reverse Shoulder Arthroplasty: Retrospective Comparison of Radiographic and Clinical Outcomes
- Comparison of CMCJ Resection Arthroplasty and Ligament Reconstruction with Tendon or Biosynthetic Collagen Interposition For the Management of Basal Thumb Arthritis
- Complete Capsule Closure Provides Clinically Significant Outcome Improvement and Higher Survivorship After Hip Arthroscopy at Minimum 5-year Follow-up
- Opioid Use and Complication Rates after Unicompartmental Knee Arthroplasty: A PearlDiver Study of Medicare Advantage Patients
- Total Joint Arthroplasty Outcomes in the Outpatient Ambulatory Surgery Center Setting
- Return to Sport and Weightlifting Analysis Following Distal Biceps Tendon Repair
- Twitter Use Amongst Orthopedic Surgery Journals: Does a Tweet Increase Citations?
- The Effect of Recovery Period on Injury Patterns and Trends among Athletes in the National Football League
- Outcomes of Obstructive Sleep Apnea Patients Undergoing Rotator Cuff Repair
- The Fate of Patients Undergoing ACI/MACI Biopsy
- Physician Burnout: Understanding the Risk Factors, Warning Signs and Prevention Strategies. How Stigma can lead to Tragedy
- Emergency Department Visits and Admissions after Total Joint Replacement in a Closed Urban Setting
- Reverse Total Shoulder Arthroplasty for Patients with Minimal Pre-Operative Pain: A Matched Cohort Analysis
- High Complication Rates for Morbidly Obese Patients After Total Hip Arthroplasty in a Predominantly African American and Hispanic Population
- Increased 90 Day Mortality and Morbidity in Recovering Elective Arthroplasty Patients During the 2019 Coronavirus Pandemic in New York City
- Pericapsular Nerve Group Block in Total Hip Arthroplasty Reduces Peri-operative Complications
- Medial Patellofemoral Ligament Reconstruction With and Without Mersilene Tape Augmentation
- The Effectiveness of Injection with Orthosis for the Treatment of Trigger Finger
- MPFL Reconstruction in the Pediatric Population: Does Skeletal Maturity Affect Outcomes?
- Systematic review and meta-analysis of anterior cervical discectomy and fusion with plate and screw construct versus anchored cage
- Optimizing The Use of Liposomal Bupivacaine in Shoulder Arthroplasty
- Location of the Digital Neurovascular Bundles in Relation to a Mid-axial Incision Line: A Cadaveric Study
- Location of the Flexor Carpi Radialis Myotendinous Junction: A Cadaveric Study
- Identifying the Location of the Flexor Digitorum Superficialis Tendon Insertion
- Onlay Patellofemoral Arthroplasty in Patients with Isolated Patellofemoral Arthritis - A Systematic Review
- A Three-Dimensional Magnetic Resonance Imaging Based Morphologic Study of Post-Arthroscopy Hip Instability
- Evaluation of Rotator Cuff Repair with Concomitant Biceps Treatment: A Retrospective Review of Patient Outcomes
- Real World Survey Burden of Common Patient-Reported Outcome Measures Utilized in Shoulder Surgery
- Pigmented Villonodular Synovitis of the Hip in Patients Undergoing Total Hip Arthroplasty: A Retrospective Case-Controlled Analysis
- Intraoperative Testing of Hip Capsular Repair Demonstrates Restoration of Axial Distraction Resistance
- The Effect of Age and Activity Level on SLAP Repair Outcomes
- Factors Affecting Pelvis Position During THA in the Lateral Decubitus Position
- Freestyle skiing is associated with similar proximal femur and lumbar spine adaptations and lower body mass index as compared to skiers in non-freestyle events
- Quantifying Survival and Mortality Among Geriatric Orthopaedic Trauma Patients: A Retrospective Chart Review
- Manipulation Under Anesthesia following Two-Team Simultaneous Primary Total Knee Arthroplasty
- Optimal Treatment For Glenoid Bone Loss: Augmented Versus Standard Reverse Shoulder Arthroplasty?
- Arthroscopic Repair of Femoral-Sided PCL Avulsions Using a Transosseous Drilling Technique - a Retrospective Review
- Before or After? An Assessment of 1-Year Complications in Spinal Fusion and Total Hip Arthroplasty
- Far Cortical Locking Versus Standard Locking Screw Fixation in Simulated Femoral Fractures: A Biomechanical Meta-Analysis
- Orthopaedic Fellowship Information for an AOA applicant
- Bilateral Simultaneous Anterior Cruciate Ligament Ruptures in a Female Skier with Systemic Lupus Erythematosus
- Case Study: The Effect of Medicaid Expansion on Payments to Orthopedic Surgeons from Industry
- Impact of HIV Status on Surgical Outcomes after Primary Total Hip Arthroplasty
- Prolonged LOS After Primary TKA in an Urban, High-Volume Joints Center Serving Socioeconomically Disadvantaged Minority Populations
- Non-narcotic Total Joint Arthroplasty using an Alternative to Opioids (ALTO) Multimodal Pain Protocol: a Comparison of 90-day Outcomes
- Tissue-Engineered Augmentation of A Rotator Cuff Tendon Using A Novel Bio-Inductive Biocomposite Scaffold: A Preliminary Study In Sheep
- Impact of Resident Involvement on Complication Rates in Revision Total Knee Arthroplasty
- Operative Room Time Comparison between General and Spinal Anesthesia in Total Hip Arthroplasty: An Institutional Review
Comparing Outcomes of Anterior versus Posterior Shoulder Instability: A Systematic Review and Meta-Analysis
- Presenting Author: Reed Coda
- Additional Authors: Matthew Vopat, Nick Giusti, Jordan Baker, Armin Tarakemeh, John Paul Schroeppel, Scott Mullen, Jeffrey Randall, Matthew Provencher, Bryan Vopat
Introduction: The purpose of this study was to conduct a systematic review and meta-analysis to evaluate and compare outcomes between anterior versus posterior shoulder instability.
Methods: A systematic review was performed using the PubMed, Cochrane Library, and MEDLINE databases (inception – September 2019) according to Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. Outcomes from anterior and posterior shoulder instability including percentage to return to sport (RTS), post-treatment instability, and pre-/post-treatment American Shoulder and Elbow Surgeons (ASES) Shoulder Score were recorded and analyzed.
Results: Patients with anterior instability were significantly more likely to RTS than patients with posterior instability (Odds Ratio: 2.5558, p < 0.001, 95% CI: [1.9674, 3.3209]). Patients with anterior instability were significantly more likely to have post-treatment instability than patients with posterior instability (Odds Ratio: 3.4294, p < 0.001, 95% CI: [2.4502, 4.9047]). Within patients who underwent an operation, patients with anterior instability were significantly more likely to RTS than patients with posterior instability (Odds Ratio: 2.3118, p <0.001, 95% CI: [1.7591, 3.0379]). Within anterior instability, patients who had operations were significantly less likely to have post-treatment instability than non- operative patients (Odds Ratio: 0.1439, p <0.001, 95% CI: [0.1153, 0.1791]). ASES functional scores in patients with anterior instability were not significantly different than patients with posterior instability (Difference of means: 0.0012, p = 0.9996, 95% CI: [-4.5351, 4.5375]). Males were significantly more likely to have anterior instability while females were significantly more likely to have posterior instability (Odds Ratio: 1.5677, p = 0.001, 95% CI: [1.2405, 1.9744]).
Conclusions: Patients with anterior shoulder instability are associated with better outcomes with regards to RTS but are more likely to have post-treatment instability compared to patients with posterior instability. Compared to non-operative patients with anterior instability, patients with anterior instability who underwent operative interventions were more likely to RTS and suffered from less post-treatment instability.
Failure of Liposomal Bupivacaine in Managing Postoperative Pain Following Shoulder Surgery
-
Presenting author: Wilfredo Borroto
-
Additional authors: Joel Grunhut, Vani Sabesan, Kiran Chatha, Matthew Wilneff, Gregory Gilot
Introduction: As the US is in the midst of an opioid crisis, increased focus has been placed on reducing opioid consumption. Novel multimodal pain protocols including the use of liposomal bupivacaine (LB) has shown success in minimizing opioid usage. However, to optimize utilization of LB treatment further research is needed to better understand its limitations. Understanding why these protocols fail may help predict and prevent these failures. The purpose of our study was to analyze the risk factors and determinants of liposomal bupivacaine failure in orthopedic shoulder surgeries.
Methods: This was a retrospective review of 119 patients undergoing shoulder surgery. Twenty one patients were included in the LB failure group (LBF) and 99 in the control group. Patients were included in the LBF group if they had reported VAS pain scores of 7 or greater at either time surveyed. All patients received a standardized multimodal pain management protocol that included an interscalene block and a local infiltration of LB at incision closure. Visual analog scales (VAS) were administered at 24 and 48 hours and 7 days postoperatively. Patient demographics, pain scores and opioid consumption were compared.
Results: There were a total of 65 males and 54 females with an average age of 66.7 years old included in the study. The LBF group had higher average ASA classes at 2.23 compared to 1.88 (p=0.026), but there were no differences in gender distribution and BMI between groups. The LBF group had 31% patients with a history of chronic opioid use compared to none in the control (p<0.001). The LBF had a higher incidence of comorbidities, and significantly higher proportions of chronic pain syndromes (100% vs 23%) (p<0.001)) and history of surgical procedures (46% vs 17%) (p<0.0001). The LBF group had average pain scores of 8.3 and 6.7 at 24 and 48 hours compared to 2.7 and 3.3 in the control group (p<0.001). At 7 days postoperatively the LBF group still had significantly higher pain scores than the control at 4.1 compared to 2.0 (p=0.03). There were no differences in opioid consumption between groups.
Discussion and conclusions: LB may not be effective in older patients with chronic pain syndromes, history of opioid use and past surgeries. It is important for surgeons to include these factors in recognizing limitations of multimodal pain regimens and designing an appropriate postoperative pain management plan for patients undergoing shoulder surgery. Future studies should integrate these factors into postoperative pain management risk assessment tools in these patient populations.
Epidemiology of Ankle Sprain in the Military: A Systematic Review of Literature
-
Presenting author: Allison Goodrich
-
Additional authors: Matthew Mackay, Brandon Morris, Christina Hermanns, Ashley Herda, Armin Tarakemeh, Bryan Vopat
Introduction: Ankle sprains occur frequently within the general population, however, the extent to which this injury impacts the military population remains unknown. Lateral ankle ligament injury may impact military readiness and incur costs to the military healthcare system. The purpose of this study is to systematically review the literature describing lateral ankle ligament injury in the military population.
Methods: Following PRISMA guidelines, articles were retrieved from PubMed, Embase, and Cochrane Library using the search terms “military,” “epidemiology,” “incidence,” “prevalence,” “ankle sprain,” and “ankle instability.” Inclusion criteria consisted of active military duty status, English language, and levels of evidence I-IV.
Results: Nineteen articles were included, representing 1,671,763 study participants from six countries and four branches of the military—Army, Navy, Air Force, and Marine Corps. Among the ten studies that reported ankle sprain incidence in terms of overall injury incidence, seven studies reported ankle sprain as the most common injury, with an incidence ranging from 2.20% to nearly one third of all injuries in the paratrooper population. Two studies reported ankle sprain as the second and third most common injury, with incidences of 15.1% and 7.82%, respectively. Ankle sprain was also reported as the most common injury among lower extremity injuries in two studies, with incidences of 35% and 38.7%, respectively. Ankle sprain incidence rate per 1,000 person-years was reported in four studies, with values ranging from 15.3 to 58.4. Incidence rate was also reported for males and females separately in three of these studies, ranging from 33.89 to 52.7 for males, and 41.17 to 96.4 for females. One study reported physical therapy volume and found ankle sprains to have the greatest contribution to overall volume. The number of days lost to ankle sprain ranged from one to eight days per servicemember, and one study reported a cumulative 4,252 days lost to ankle sprain over a three-year period.
Conclusion: Ankle sprains are among the most prevalent injuries within the military population. This injury results in significant time away from active duty, which impacts overall readiness within the military system.
Grade 3/4 Chondromalacia of the Hip: Is Microfracture Worth It?
-
Presenting author: Mathew Meade
-
Additional authors: Patrick Szukics, John Salvo, Andrew Wolff, Shane Nho, John Christoforetti, Dean Matsuda, Dominic Carreira, Ben Kivlan
Introduction: There are no studies evaluating the necessity of microfracturing in patients with grade three or four chondromalacia of the hip. Therefore, we sought to compare the two-year functional outcomes and pain scores in patients with grade three and four chondromalacia of the hip who underwent hip arthroscopy with microfracturing compared to those without microfracturing.
Methods: Data between 2013 and 2017 was retrospectively reviewed. Patients included were those undergoing hip arthroscopy for an Outerbridge grade three or four chondral defect and a minimum two- year follow up with International Hip Outcome Tool (iHot) and visual analog scale (VAS) for pain scores. Patients were then matched for age, gender, preoperative VAS pain scores, and preoperative iHOT scores.
Results: 249 patients were included in the study, with 24 patients undergoing microfracture and 225 patients not undergoing microfracture. The preoperative age (microfracture=36.48, non-microfracture= 6.62), VAS pain score (microfracture=46.01, non-microfracture=52.01), and iHOT score (microfracture=31.62, non-microfracture=36.41) were similar between the two groups. The two-year VAS pain scores (microfracture=24.47, non-microfracture=23.07) and iHOT scores (microfracture=70.31, non-microfracture=70.94) were similar between the two groups. When matched for age, gender, preoperative VAS pain scores and preoperative iHOT scores, the microfracture group had improved two-year VAS pain scores (microfracture=25.12, non-microfracture=35.62, p=0.12) and improved two-year iHot scores (microfracture=70.25, non-microfracture=58.05, p=0.09), although the results were not statistically significant.
Conclusion: In patients undergoing hip arthroscopy for Outerbridge grade three and four chondral defects, there is a trend towards improved two-year VAS pain scores and iHot scores in the microfracture group compared to the non-microfracture group, although it was not statistically significant. Microfracture should be considered as a treatment option in patients undergoing hip arthroscopy for Outerbridge grade three and four chondral defects. Further studies are needed to evaluate for the effectiveness of microfracture in this patient population.
Review of Rehabilitation Protocols Designated for Meniscal Repairs: A Systematic Review and Analysis
-
Presenting author: Seth Carder
-
Additional Authors: William Messamore, David Scheffer, Nick Giusti, John Schroeppel, Scott Mullen, Bryan Vopat
Introduction: The purpose of this paper is to compare publicly available rehabilitation protocols designated for meniscal repairs published online by academic residency programs and private practice institutions to determine the variability in radial versus non-radial repair protocols.
Methods: Using the Fellowship and Residency Electronic Interactive Database Access System, a list of available academic residency programs and orthopedic sports medicine fellowships was obtained. Utilizing this list, an electronic search using Google was performed looking for meniscal repair rehabilitation protocols. Private practice organizations with published meniscus repair rehabilitation protocols found during the search were also examined.
Results: Altogether, 30 academic institutions and 29 private practices had protocols that met inclusion criteria. Six of the 59 specified radial repair. For return to full range of motion (ROM), non-radial protocols averaged 6.7 weeks and radial protocols averaged 7.3 weeks. For return to full weight bearing, non-radial protocols averaged 6.2 weeks and radial protocols averaged 7.5 weeks. For return to sport (RTS), non-radial protocols averaged 17.8 weeks and radial protocols averaged 23.3 weeks. For time spent in a brace, non-radial protocols averaged 5.7 weeks and radial protocols averaged 6.7 weeks.
Conclusion: Of available meniscal repair rehabilitation protocols, only 10.2% changed their protocol in relation to tear type. Protocols for radial tear patterns braced patients longer, limited their ROM longer, delayed full weight bearing, and delayed RTS. Future studies are needed to help specify which rehabilitation protocol would be optimal for each patient’s repair based on tear pattern and location
Effects of Complete A4 Pulley Release on Bowstringing of FDP tendons in a Cadaveric Model
-
Presenting author: Daniel Lara II
-
Additional authors: Michael Holmboe, Shayne R Kelly, Brenden Cutter, Eric Huish, Marc A Trzeciak
Background: The A4 pulley aids in proper flexor tendon mechanics. Although its importance in preventing bowstringing has been well established, partial or complete release of the A4 pulley has gained attention in the setting of flexor tendon repair recently. If done properly, releasing these pulleys can improve functional recovery and is unlikely to cause clinical problems. The purpose of our cadaveric study was to examine bowstringing of the flexor tendon when the A4 pulley is released. We also examined bowstringing with additional release of C1, A3, and C2 pulleys.
Methods: The index, long, ring and small finger flexor digitorum profundus (FDP) tendons were studied on five cadaveric hands. The FDP tendon was exposed on each of the digits from the MCP to DIP joints through a midline volar incision. Manual traction was applied to the FDP tendon in order to form a composite fist. Measurements of pulp to palm distance and flexor tendon bowstringing were measured with intact pulley and with subsequent release of the A4 pulley, followed by the release of the C1, A3, and C2 pulleys as a unit. Bowstringing was measured using the distance from the middle phalanx to the dorsal aspect of the FDP tendon, using digital calipers.
Results: ANOVA showed no difference in bowstringing between finger types with A4 released (p=0.119) or with C1-A4 released (p=0.467). The mean (± SD) bowstringing present as measured by the widest gap between the tendon and bone was 1.55 (± 1.00) mm in the A4 released group vs. 3.54 (± 1.30) mm in the C1-A4 released group. This difference was statistically significant (p=0.0002).
Conclusions: Our results support the evidence that the loss of the A4 pulley alone may be mechanically well-tolerated. However complete transection of A4-C1 results in significant anatomical bowstringing. Clinically, it is important for the surgeon to decide which window to work in. They can use either C1, A3, C2 window or A4 window but not both
Biologic Graft Augmentation for Glenoid Bone Loss in Revision Reverse Shoulder Arthroplasty (rTSA)
-
Presenting author: Elizabeth Ford
-
Additional Authors: Sean McMillan, Paul Favorito
Introduction: Glenoid bone loss presents a challenging dilemma for the surgeon, particularly in the setting of failed arthroplasty requiring conversion to a reverse total shoulder arthroplasty (rTSA). Risks involved with significant glenoid bone loss include: scapular notching, glenoid loosening, instability, pain, reduced function, and potentially catastrophic failure. Current options for addressing this deformity are custom baseplates and glenospheres, eccentric reaming, metallic glenoid augments and biologic glenoid grafting. The use of biologic glenoid bone grafting to address vault deficiencies has been met with mixed results in the literature, however, may provide advantages over other options.
Methods: A systematic review of the literature using a PUBMED search of articles related to: revision to reverse shoulder arthroplasty, bone grafting, and glenoid bone loss was performed. 383 articles were identified and after abstract review 21 papers were selected for complete review. After removal of articles that did not pertain to glenoid bone deficiency secondary to OA or failed previous procedures; 7 articles consisting of 87 patients were deemed to meet criteria.
Results: Outcomes were reviewed with the primary endpoint of success being failure of the graft to incorporate resulting in the need for further intervention. 16/87 patients had a structural autograft from tri-cortical iliac crest grafting. 15/87 had non-structural allografting. 56/87 had structural allografting from either the femoral head, proximal humerus, or iliac crest. The overall failure rate of grafting was 24% (21/87). Allograft demonstrated a 15% failure rate (11/87) and autograft demonstrated a 38% failure rate (6/16). Other causes of failure such as infection, fracture, and iatrogenic nerve injury were noted across all graft types.
Conclusion: Grafting for glenoid bone loss in the setting of conversion to reverse shoulder arthroplasty (rTSA) has been shown to have positive outcomes. Proper technique and patient selection can help avoid potential complications associated with glenoid vault medialization and posterior wear. In the setting of rTSA, the primary mode of function is premised upon the stability of the glenosphere and its’ associated fixation to the glenoid. While much has been written about glenoid bone grafting for primary osteoarthritis in the setting of total shoulder arthroplasty, this is the first meta-analysis looking specifically at the role it plays in the revision setting for conversion to reverse shoulder arthroplasty. The authors acknowledge a low number of autograft patients may skew the failure rates in this group, however in the setting of a revision the most common form of autograft, humeral head, is not available. Alternatively, this meta- analysis points towards the potential benefit of allograft, particularly femoral head, for this patient population.
Better Outcomes? Rotator Cuff Repair versus Reverse Shoulder Arthroplasty for Massive Rotator Cuff Tears in Elderly Population
-
Presenting author: Laila Khoury
-
Additional authors: Vani Sabesan, Kiran Chatha, Joel Grunhut, Andres Guerrero, Gregory Gilot
Introduction: Despite advances in surgical technology with rotator cuff repairs, there is a high re-tear rate for large and massive rotator cuff tears, up to 90%. Due to their complexity and poor outcomes, large or massive RCT present a substantial challenge to orthopedic surgeons. An alternate treatment option more recently offered to elderly patients is reverse shoulder arthroplasty (RSA) for massive RCT. The purpose of this study was to compare outcomes, opioid usage, and pain scores for patients treated with RCR versus RSA for massive RCT.
Methods: A retrospective review of 400 patients was performed to identify 32 patients with massive RCT treated with RSA and RCR at a single institution from 2017-2019. All patients were treated for large or massive rotator cuff tears by two fellowship trained shoulder surgeons. Preoperative and postoperative outcome scores including opioid usage, American Shoulder and Elbow Surgeons (ASES) scores, Penn (PSS) scores, Constant scores (CS), and Subjective Shoulder Value (SSV) were collected. Demographic variables and outcomes scores at preoperative assessment and postoperatively at 6 weeks, 3 months, and 6-12 months were compared using t-tests and multivariable regression modeling.
Results: In the cohort there were 22 males and 10 females with average age of 62 for the RCR and 67.3 for the RSA (p≥ 0.05) and BMI of 28.9 and 29.3 for each group respectively. At baseline there were no differences between groups for ASES pain or function scores (p=0.27 and p=0.74), PSS pain or function scores (p=0.84 and p=0.93), CS (p=0.14) and SSV (p=0.90). At 6 weeks, the average PSS function, ASES function and CS scores for RSA group were significantly higher compared to the RCR group (p=0.01, p=0.02, p=0.03). All patient reported outcomes at 3 months and 6 months postoperatively were not significantly different between groups.
Conclusion: Our results demonstrated that both RCR and RSA showed significant improvements in all pain and functional scores with significant difference seen only in initial recovery at 6 weeks. RSA is comparable to RCR and shows earlier improvements and faster functional return postoperatively which is not surprising given the delays in rehab after massive RCR. Further studies are needed examining long term function and reoperation rates in these patients
The Role of Preoperative Magnetic Resonance Imaging (MRI) in Surgical Decision Making for Total versus Medial Unicompartmental Knee Arthroplasty
-
Presenting Author: Maddison Morgan
-
Additional Authors: Dr. Shane Davis, Dr. Christopher Lee
Introduction: Unicompartmental knee arthroplasty (UKA) is currently considered favorable over total knee arthroplasty (TKA) due to quicker recovery and high postoperative function; however, UKA failure rates remain high and there is a lack of universal guidelines for operative planning. The purpose of this study was to investigate the role of preoperative MRI in surgical decision making for medial (UKA) vs. total knee arthroplasty (TKA).
Methods: A total of 54 knees of 51 consecutive patients who underwent knee replacement surgery were analyzed retrospectively. Patients who were deemed candidates for UKA based on stress view radiographs and physical exam underwent MRI scans to assess candidacy. Exclusion criteria on MRI included lateral meniscus tears, loose bodies, grade 3-4 chondromalacia, anterior cruciate ligament (ACL) tears, sclerosis and osteoarthritis in more than one compartment of the knee.
Results: 40% of patients who were candidates for medial UKA based on stress view radiographs and physical exam alone were deemed only TKA candidates based on exclusion criteria found in the preoperative MRI. Lateral meniscus and anterior cruciate ligament (ACL) tears were the two most common exclusion criteria found.
Conclusions: Preoperative MRIs, in conjunction with stress view radiographs and physical exam, should become part of the surgical decision making for UKA vs. TKA. While MRIs pose an additional cost, the current high failure rate of UKA and the high cost of conversion to TKA make it a more beneficial solution. As the indications for UKA continue to grow, superior imaging, including MRIs, are needed for surgical planning.
Psychological Burnout and Age of Sport Specialization: A Profile for Current NCAA Big 12 Student-Athletes
-
Presenting author: Nick Giusti
-
Additional authors: Seth Carder, Jordan Baker, Lisa Vopat, Bryan Vopat, Jeff Randall
Background: Adolescent sport specialization has increased significantly in recent years despite a growing body of evidence showing negative consequences such as increased rates of burnout and injury. The purpose of this study was to survey current NCAA student-athletes to compare levels of burnout to gender, year of NCAA eligibility, and age of beginning sport specialization.
Methods: Student-athletes at two NCAA Division I institutions were surveyed asking about sport specialization history along with the Athlete Burnout Questionnaire. Results from the Athlete Burnout Questionnaire were compared to gender, year of NCAA eligibility, and age of beginning sport specialization.
Results: 267 athletes filled out the survey to completion including 95 males and 172 females. 156 were in their first or second year of NCAA eligibility, and 111 were in their third, fourth, or fifth year. 121 reported specializing before the age of 15, and 140 specialized at age 16 or older. Females reported significantly higher levels of exhaustion than males (Difference of means (M) = 0.43, 95% confidence interval (CI) = [0.20, 0.66], p <0.01), but not significantly higher feelings of reduced sense of accomplishment (M = 0.17, 95% CI = [-0.03, 0.37], p =0.09), or sport devaluation (M = 0.14, 95% CI = [- 0.08, 0.36], p =0.14). Athletes in their third, fourth, or fifth year of eligibility reported significantly higher levels of sport devaluation (M = 0.27, 95% CI = [0.05, 0.48], p <0.05), but not significantly higher feelings of reduced sense of accomplishment (M = 0.16, 95% CI = [-0.03, 0.35], p =0.11) or exhaustion (M = -0.07, 95% CI = [-0.29, 0.15], p =0.54) than athletes in their first or second year. Athletes who specialized before 15 did not report significantly higher levels of burnout than athletes who specialized at age 16 or later in sense of reduced accomplishment ((M) = 0.14, 95% confidence interval (CI) = [-0.04, 0.33], p =0.14), exhaustion (M = 0.09, 95% CI = [-0.14, 0.32], p =0.44), or sport devaluation (M = 0.09, 95% CI = [-0.13, 0.31], p =0.43).
Conclusion: Current NCAA female athletes are more likely to experience the burnout symptoms of exhaustion than males. NCAA athletes later in their careers are more likely to experience burnout in terms of sport devaluation. Finally, beginning sport specialization before 15 years old did not have a significant change in burnout symptoms compared to specializing 16 or older.
Major and Minor Complications in Patients with Generalized Anxiety Disorder Undergoing Single-Level Anterior Cervical Discectomy and Fusion
-
Presenting author: Zan Naseer
-
Additional authors: Matthew McIntyre, Cristian Brotea, David Asprinio
Introduction: Anxiety has been reported in up to 1 in 5 orthopaedic patients, with greater anxiety scores reported in the spine surgery patient population. Higher anxiety scores may ultimately lead to worse patient reported functional and pain scores following surgery. The purpose of this study was to compare patient demographics and rates of inpatient perioperative complications following elective single-level anterior cervical discectomy and fusion (ACDF) in patients with an established diagnosis of generalized anxiety disorder (GAD) versus patients without GAD.
Methods: The National Inpatient Sample from 2009 through 2015 was used to analyze patient characteristics (age, race, sex, number of preexisting Elixhauser comorbidities, hospital length of stay) and perioperative complications of patients with GAD following elective single-level ACDF. The International Classification of Diseases, ninth and tenth revision, Clinical Modification (ICD-9-CM, ICD-10-CM) procedure codes were used to identify all patients undergoing a single-level ACDF. Exclusion criteria consisted of age younger than 18 years old, admission through the emergency department, cervical trauma, cervical abscess/infection, and cervical discitis. Minor perioperative complications consisted of dysphagia, dysphonia, length of stay ≥ 5 days (90th percentile), acute blood loss anemia, seroma or hematoma, postoperative wound infection, and deep venous thrombosis. Major perioperative complications consisted of mortality, acute kidney injury, congestive heart failure, myocardial infarction, pneumonia, pulmonary embolism, stroke, and paralysis. Chi-squared tests were used for binary variables and T-tests for continuous variables. Univariate analysis was done to assess for statistical significance between groups for patient demographics and both major and minor perioperative complications. Further analysis was done using a multivariate regression controlling for patient age, sex, and race as covariates (significance, p < 0.01).
Results: Patients with GAD (n=36,096), as compared to patients without depression (n=350,540), who underwent ACDF were significantly more likely to be younger (54.3 ± 0.7 vs. 56.1 ± 0.02, p< 0.001), more likely to be female (63.7% vs 53%), have a greater LOS (3.0 ± 0.01 vs 2.7 ± 0.01, p<0.001), and have a greater number or preexisting medical comorbidities (6.2 ± 0.01 vs. 4.0 ± 0.004, p<0.001). Patients with GAD were more likely to have any major (3.6% vs. 3.0%, p<0.001) or minor (11.0% vs. 8.4%, p< 0.001) perioperative complication. Multivariate regression analysis revealed that GAD was independently associated with a higher likelihood of acute kidney injury (odds ratio, 1.3; 95% CI, 1.2-1.5), CHF (odds ratio, 1.5; 95% CI, 1.4-1.7), MI (odds ratio, 1.5; 95% CI, 1.1-1.9), pneumonia (odds ratio, 1.6; 95% CI, 1.4-1.9), dysphagia (odds ratio, 1.5; 95% CI, 1.4-1.6), length of stay > 5 days (odds ratio, 1.36; 95% CI, 1.32-1.4), blood loss anemia (odds ratio, 1.4; 95% CI, 1.3-1.5), and seroma/hematoma (odds ratio, 1.2; 95% CI, 1.0-1.3).
Conclusions: Generalized anxiety disorder is independently associated with several minor and major perioperative complications following elective single-level ACDF. Assessing pre- and postoperative mental health may play an integral in overall patient outcomes following elective cervical spine surgery. Future studies exploring the risk factors and management strategies for anxiety in spine patients will provide insight into the biopsychosocial dynamics responsible for patient outcomes. Orthopaedic spine surgeons should consider a comprehensive psychiatric screen as an integral component of their preoperative workup.
The Influence of Pharmacological Osteoporosis Treatment on Refractures Following Kyphoplasty
-
Presenting author: Imran Noor Alam
-
Additional authors: Chris Hanson, Mustasim Rumi
Introduction: The aim of this study was to examine the relationship between pharmacological osteoporosis treatment on the refracture rate in patients who have had a thoracic or lumbar level kyphoplasty for a diagnosis of osteoporotic compression fracture.
Methods: A single center observational cohort study with 192 patients who had kyphoplasty from 2015 until 2019 was conducted. All patients who had at least one kyphoplasty from the center were included in the study. The patients were divided into two main groups. Group I (pharmacological osteoporosis treatment) and Group II (no pharmacological osteoporosis treatment). Each group had 96 patients. In this study, refracture was defined as having at least one future osteoporotic compression fracture requiring a kyphoplasty after the initial. Patients who were successfully treated in a brace were exempt from the study. Patients that had a subsequent fracture following the initial kyphoplasty procedure were placed into the “Post Kyphoplasty Refracture” (PKR) category, whereas those that didn’t have a fracture subsequent to the initial kyphoplasty were categorized as “No Post Kyphoplasty Refracture” (NPKR). The refracture rate was determined for each group. 44 patients self-reported the intent to start osteoporosis treatment with their Primary Care Provider (PCP) and were placed in Group I based on the assumption that they were an Intended to Treat Group (ITT). A Chi Square Independence Test was used to analyze the data.
Results: There were 121 females and 71 males with an average age of 77 years. There was a significant reduction in the refracture rate between Group I and Group II (p=0.036). Group I PKR showed a 20.8% refracture rate (20/96) versus a 34.4% refracture rate in Group II PKR (33/96). In Group I NPKR 58% (44/76) patients claimed to start pharmacological osteoporosis treatment with their PCP. These patients were part of the ITT population. In Group I, the ITT group (44/76) were the only patients who were lost to follow up. No patients in Group II were lost to follow up. The Chi Square Independence score was 4.4045.
Conclusions: There was a significant reduction in refractures following kyphoplasty in patients who had pharmacological osteoporosis treatment. The Chi Square Independence Test suggested a strong dependent relationship pharmacological osteoporosis treatment and the refracture rate following kyphoplasty.
How Should PROMs Be Used? The Development of Quality Measures for Using Patient Reported Outcome Measures in Hand Surgery
-
Presenting author: Lauren Shapiro
-
Additional authors: Edward Akelman, David Ruch, Marc Richard, Amy Ladd, Phil Blazar, Sanjeev Kakar, Jeffrey Yao, Alex HS Harris, David Ring, Christopher Got
Introduction: As the burden of surgical care and associated outreach trips to low- and middle-income (LMIC) countries increase, it is important to collect post-operative data to assess and improve the quality, safety, and efficacy of the care provided. In this pilot study, we aim to evaluate the feasibility of SMS- based mobile phone follow-up to obtain patient-reported outcome measures (PROMs) after hand surgery on a surgical outreach trip to Vietnam.
Methods: Patients undergoing surgery on a week-long outreach trip to Hospital 175 in Ho Chi Minh City, Vietnam who owned a mobile phone were included in this study. All eight eligible patients elected to participate and were sent an SMS-based, HIPAA-compliant text message with a link to a contextualized QuickDASH on the following post-operative time points: one day, one week, two weeks, four weeks, and twelve weeks. Patient characteristics, instrument completion rates, and instrument scores were reported.
Results: The eight patients had a mean age of 45.4 years and lived a mean distance of 72.7 km from the hospital. Seven (87.5%), seven (87.5%) , eight (100%), six (75%), and eight (100%) patients completed follow up questionnaires at one day, one week, two weeks, four weeks, and twelve weeks post- operatively, respectively. The mean QuickDASH scores were 54.9 (day 1), 59.1 (week 1), 53.0 (week 2), 45.5 (week 4), 33.6 (week 12). The mean change in QuickDASH score from day 1 to week 12 was -21.0.
Conclusion: This pilot study demonstrates that collection of PROMs after hand surgery outreach trips to LMIC via SMS-based messaging is feasible up to twelve weeks post-operatively. As the number of outreach trips and the resources invested in such trips increase, it is important to ensure the care provided is safe and improves the health of patients. This technology can be scaled and contextualized based on location to ensure patient care on outreach trips is safe and effective.
Treatment of Severe Ankle and Hindfoot Deformity: Technique Using Femoral Head Allograft for Tibiotalocalcaneal Fusion Using a Cup and Cone Reamer
-
Presenting author: Victor Hoang
-
Additional authors: Shivali Gupta, Taylor Anthony, Victor
Introduction: Malalignment of the ankle and hindfoot is a common pathology in patients with end-stage ankle arthritis.1 Limb shortening due to structural bone loss in TTC arthrodesis is also a concern that can negatively impact the patient’s gait and weight-bearing. To aid in preventing the risk of limb shortening, the use of a femoral head allograft and intramedullary nail in TTC arthrodesis has been shown to successfully preserve limb length in patients with structural bone deficits.
Case Presentation: 64-year-old with a severe fixed ankle valgus deformity underwent an ankle arthrodesis through a lateral approach with fibular osteotomy. 1-year post op, patient was found to have an incomplete deformity correction, nonunion with potentially a neuropathic joint. Indications for Femoral Head Allograft for Tibiotalocalcaneal Fusion include large talar body defects, severe fixed deformity of ankle and hindfoot
Surgical Technique: Distal tibia and remaining talus or calcaneus are prepared with an acetabular reamer, this creates a concave surface for secure placement of the convex interposition femoral head allograft and increases the amount of bone-to-bone contact between the allograft and the residual host bone. This provides a stable construct for alignment and placement of the IM nail to TTC fusion
Conclusion: We present surgical technique guide and video for the treatment of severe fixed ankle valgus deformity utilizing a femoral head allograft for tibiotalocalcaneal fusion using a cup and cone reamer.
Determinants of Physical Therapy Utilization Following Shoulder Surgery: A Retrospective Review
-
Presenting author: Brett Stephens
-
Additional authors: Vani Sabesan, Mauricio Drummond, Mirelle Dawoud, Levonti Ohanisian, Ahmed Al-Mansoori, Matthew Wilneff, Joel Grunhut, Christian Martinez
Introduction: Postoperative physical therapy (PT) is cornerstone for patients to achieve optimal range of motion and better overall patient-centered outcomes following orthopedic shoulder surgery. Access to postoperative PT can be limited by insurance type (private vs. Medicare) and cost. The goal of this project was to describe the trend of physical therapy utilization among patients with different insurance types that undergo shoulder surgery.
Methods: This was a retrospective analysis of 80 patients that underwent shoulder surgery along with physical therapy sessions before and after surgery. The patients were placed into two groups, based on insurance type: privately insured (PI) (42) and Medicare with or without supplemental insurance (MSI) (n=38). Data collection included demographics, comorbidities, diagnosis, copay, number of sessions covered, and number of sessions used before and after surgery. Statistical analysis included Chi-square, independent t-test and multinomial logistic regression based on copay.
Results: The average age of the cohort was 61.8 years with 27 males and 53 females with an average BMI of 28. There were no significant differences between groups at baseline other than age, where the MSI group was older (70 vs 55) (p<0.01). Overall, the average number of sessions covered was 65 with an average copay of $15. The average deductible for those that had one was $431.00 When comparing between groups, the average copay for the PI group was $25 compared to $6.50 in the MSI group (p<0.05). The average number of sessions covered was higher for the MSI group at 80 sessions compared to 55 in the PI group (p<0.05). There was no significant difference between the two groups in the number of utilized PT sessions after surgery. However, we found higher utilization of PT for patients with copays (22.1) compared to 15.7 for no co pay patients (p = 0.046).
Conclusions: Even though the number of sessions allotted for the Medicare group was greater and the average copay per session was lower than that for the private insurance group, there was no change in average number of sessions attended between these patients. It appears that a financial investment into rehabilitation may increase compliance and utilization for patients during postoperative rehabilitation after shoulder surgery.
Sex Related Outcomes Following Anterior Cruciate Ligament Reconstruction (ACLR): A Systematic Review and Meta-Analysis
-
Presenting author: Anthony Mok
-
Additional authors: Drew Fancher, Mary Mulcahey, Scott Mullen, John P. Schroeppel, Kim Templeton, Bryan Vopat, Matthew Vopat
Introduction: There is a paucity of information on the influence of patient sex on outcomes following ACL reconstructions. Previous studies have demonstrated that females have worse outcomes with regards to instrumented laxity, revision rate, Lysholm score, Tegner activity score, and are less likely to return to sport. However, other measures have been shown to be similar between male and female patients. The purpose of this study was to perform a systematic review and meta-analysis comparing outcomes after ACL reconstruction with regards to sex.
Methods: A systematic review and meta-analysis were conducted using PubMed, PubMed Central, Embase, Cochrane Library, and OVID (inception – April 2020) according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) guidelines. Outcomes including functional tests, re-rupture rates, re-operative rates, post-operative range of motion, post-operative stability, return-to-sport rates, and International Knee Documentation Committee (IKDC) scores were recorded and analyzed.
Results: Studies that reported post-operative IKDC scores, re-rupture rates, and revisions rates were included in the meta-analysis. Males had statistically significant higher IKDC post-operative scores (MD = 3.02; 95% CI = [1.19, 4.84]; I2 = 66%). There was no significant difference between males and females with regards to revisions (OR = 0.85; 95% CI = [0.45, 1.60]; I2=94%). Males were significantly more likely to suffer a graft re-rupture than their female counterparts (OR=1.35; 95% CI = [1.22, 1.50], I2 = 0%). Males also reported a 17% higher return-to-sport rate than females (59.82% compared to 42.89%); however, no formal statistical analysis was able to be done due to the variability in reporting techniques between papers.
Conclusion: To our knowledge, this is the most recent and comprehensive study focused on the role of a patient’s sex on ACLR outcomes. Males and females showed similar outcomes with regards to rate of revision surgery. However, males were found to have higher post-operative IKDC scores and higher re-rupture rates. Males also showed almost a 17% higher incidence of returning to sport. More studies are needed that focus directly on the effect of sex, combined with other co-variables such as age, graft used, or level of sport, to increase the breadth of knowledge on sex specific outcomes following ACL reconstructions.
Ambulatory Hip and Knee Replacement Outcomes During COVID Outbreak in Washington State
-
Presenting author: Sahir Jabbour
-
Additional authors: Christian Song, Craig McAllister, Vinod Dasa, Aric Christal
Introduction: The first case of COVID-19 in the U.S. was diagnosed on January 19, 2020 in Washington State and antibody tracing data suggests that the virus was circulating in Washington prior to this. Elective joint replacements were halted on March 19, 2020 with a goal of preserving resources and protecting surgical patients. This study evaluates patient-reported outcomes of a group of patients in Washington State who underwent elective joint replacement during the initial surge of COVID-19 and prior to the shutdown to determine the safety of elective joint replacements in the setting of COVID-19.
Methods: This is an observational study of 303 patients who underwent hip and knee arthroplasty in Washington State during COVID-19 surge between January and March 2020. Surgeries were done by surgeons experienced in outpatient techniques using a standardized protocol. Patients registered on a dedicated outpatient online platform (The SwiftPath Program, LLC) that allowed them to report their outcomes. Patients responded to clinical questionnaires (HOOS, KOOS, PROMIS) at baseline and routine postop intervals out to 6 weeks. A follow-up “COVID survey” was also used.
Results: Of the 303 patients, 220 (72.6%) registered and had partially completed the data collection. 204 (67.3%) completed HOOS and KOOS data. Of these, 119 (58.3%) were knee replacements and 85 (41.7%) were hip replacements. Average age of patients was 67.7 years (range 30 – 91). Both groups had improved KOOS and HOOS scores by six weeks. Of the 134 patients who responded to the COVID survey, no patient reported viral symptoms or developed COVID-19. Patients indicated limited physical therapy access, but recovery was not impacted. The average surgery satisfaction during pandemic score was 9.25/10.
Conclusion: This data suggests that with the help of a comprehensive patient engagement and online education platform, outpatient joint replacement surgery can be done safely with no change in quality, even during a COVID outbreak. Remotely monitoring and engaging patients can help providers monitor not only surgery specific outcomes, but more importantly any virus-related illness or transmission and participate in mitigation efforts.
The Effectiveness of Bedside Low Pressure Irrigation on Pistol Caliber Gun Shot Wounds Bacterial Contamination
-
Presenting author: Alexander J. Colen
-
Additional authors: Katherine Lindeman, Robert Ablove
Introduction: Controversy exists regarding the benefit of low-pressure irrigation of pistol caliber gunshot wounds. Our study set to examine the effect of low-pressure irrigation on bacteria quantity in a simulated gunshot wound.
Methods: Twenty lamb shanks were shot with a nine- millimeter pistol at a distance of three meters. To replicate a clinical setting, denim fabric was placed in front of the impact zone. The denim fabric was treated with a standardized number of targeted bacteria (Serratia marcescens) for post incubation colony identification. This bacterium was chosen for its easily identifiable color on growth media. Two control samples were fired upon without bacterial inoculation. Specimens were cultured immediately after impact and post irrigation with both 250cc and 500cc total normal saline. Irrigation was performed with a 60cc syringe at a rate of 20cc per second. The syringe tip was placed just outside of the entrance wound to allow back flow. Cultures for all specimens were examined after 72 hours by a microbiologist and rated on quantity of growth
Results: Of the 20 specimens that underwent firing and culture procedures, 19 provided viable data for analysis. Before irrigation, 0 (0%) plates showed no growth, 2 (10.5%) showed rare growth, 8 (42.1%) showed few growth, 6 (31.6%) showed moderate growth, and 3 (15.8%) showed many growth. After 500cc irrigation, the numbers in each category remained similar, with 2 (10.5%), 1 (5.3%), 11 (57.9%), 2 (10.5%), and 3 (15.8%) plates falling within their respective categories. A Fisher exact test confirmed that there was not a statistically significant difference in the proportion of plates within each category across all time points (p=0.59). In addition to maintaining similar proportions in each growth category across all irrigation time points, the levels of growth across each specimen showed high variability. There was no clear pattern for change in bacterial growth levels after 250cc or 500cc irrigation, with 5/19 specimens showing a sustained decrease in growth, 7/19 showing no change at either t point, 4/19 showing a transient increase in bacterial growth after 250cc irrigation that returned to baseline levels after the second 250cc irrigation, 1/19 that showed transient decrease in bacterial growth after 250cc irrigation that increased to baseline levels after the second irrigation, and 2/19 that showed sustained increases in bacterial growth. There was no significant correlation between number of irrigations and level of bacterial growth when controlling for specimen (rho = -0.15, p = 0.25).
Conclusion: Our data demonstrates no statistically significant decrease in bacterial quantity with the stated method of low-pressure irrigation for the management of pistol caliber gunshot wounds and brings into question the use of such method in the clinical setting.
Health Literacy in English vs. Spanish-Speaking Orthopaedic Chronic Pain Patients in a Closed Urban Setting
-
Presenting author: Gabriela Batista
-
Additional authors: Eva Kitlen, Natasha Richmond, Lindsey Ruda, Ariel Chen Silverman, Ira Kirschenbaum
Introduction: Health literacy is an essential element of doctor-patient communication. Inadequate literacy was also a risk factor for hospital admission among elderly Medicare patients. Additionally, patients with low levels of literacy have been shown to hold a deep sense of shame, which is often exacerbated when hospital staff express frustration when interacting with such patients. We developed and administered a novel survey that investigates the following main questions:
-
How well do patients comprehend their medical conditions?
-
What is the nature of the patient’s social connectivity to others as it relates to their health?
-
How do patients perceive both their doctor’s and their own ability to influence their health outcomes?
Methods: Chronic Pain Patients (CPPs) presenting for treatment (either general or specialized) at BronxCare’s orthopaedic clinic were randomly selected and asked to complete a 5-minute survey prior to their appointments. The survey assessed English speaking and comprehension abilities, current pain level and chief complaint, persistence of condition, comprehension of condition, whether the patient had discussed the condition with others, whether the patient was accompanied to appointments, confidence in the physician, and confidence in self. The inclusion criterion for analysis was self-reported pain for greater than 3 months in orthopaedic patients over the age of 18.
Results: 44% of patients chose to complete the survey in Spanish and 56% did so in English. Over 60% of patients reported their English speaking and comprehension abilities to be either good, very good, or excellent. CPPs reported an average pain score of 6.25/10 for conditions mostly related to the hip, leg, or knee. 42% of all CPPs could both name and describe their condition (n=24). Most CPPs came unaccompanied to their appointments (n=36, 65%), but over 85% reported previously discussing their conditions with members of their community (n=47). Of all CPPs, 75% reported confidence in their physician (n=42) and 59% reported self-confidence in improving their health outcomes (n=33).
Regressors Influencing Condition Comprehension: Condition comprehension was significantly positively correlated with both English Speaking and English Comprehension abilities (p<0.02). There were no other factors significantly correlated with condition comprehension.
English vs. Spanish-Speaking Comparisons: Survey responses for English- and Spanish-speaking cohorts were further compared for significant differences. Non-English-comprehending and speaking patients reported significantly lower confidence in their physicians to improve their health outcomes (X2=6.705, p=0.009). The two cohorts were comparable for all other responses.
Conclusions: The present study aimed to examine health literacy in a closed, urban community with a high proportion of Spanish-speaking patients. Despite the extensive interpretation services available at our hospital, patients with poor English capabilities still showed significant decreases in their condition comprehension and overall confidence in their physician. Language differences can interrupt the flow of health information from practitioner to patient, leaving the patient less informed regarding their health. The Spanish-speaking cohort also showed significantly lower levels of confidence in their physicians. The results beg further investigation into a detailed analysis of this issue.
Characterizing Comorbidities in Total Joint Arthroplasty Patients in a Safety-Net Hospital Using the Age-Adjusted Charlson Comorbidity Index
-
Primary author: Noshin Nuzhat
-
Additional authors: Melanie Anaya, Gabriela de Queiroz Campos, Ariel Chen Silverman, Ronald Huang, Morteza Meftah, Ira H. Kirschenbaum
Introduction: Total knee and hip arthroplasty is often performed for severe cases of osteoarthritis. It is generally performed on older patients, usually over 55 years of age, and is more common in obese patients [1,2]. It is well documented that joint arthroplasty population has a high number of comorbidities at the time of surgery, which can greatly affect surgical outcomes. The presence of multiple comorbid diseases has been shown to increase patient’s length of stay and lead to greater utilization of resources after a total knee arthroplasty [3]. It may also delay diagnosis, alter treatment, lead to complications, influence survival, and confound analysis of outcomes [4]. The goal of the present study is to analyze the distribution of comorbid diseases in patients who have undergone total joint arthroplasty at BronxCare Health System, which serves the poorest congressional district in the United States. We hypothesize that patients in this large, closed urban setting have a high incidence of comorbidities, calculated as both total number of conditions using the hospital’s internal comorbidity formula and scoring system, and using the Age-Adjusted Charlson Comorbidity Index (ACCI), thus requiring a shift in the bundled payment structure to account for the actual resource use as a result of the pre-existing comorbidities.
Methods: A retrospective analysis was conducted reviewing consecutive total joint arthroplasty patients at BronxCare Hospital System receiving surgery between 2008 and 2018 (N=1836). All procedures were performed by two fellowship-trained joint replacement surgeons. The total number of conditions per person was determined using the department’s own formula which takes into account additional comorbidities and risk factors common in our particular patient population proven to increase risk of complications such as obesity, anemia or smoking status, but does not weight the comorbidities by severity. Additionally, the relevant comorbidities were used to calculate the Age-Adjusted Charlson Comorbidity Index (ACCI), which is includes fewer comorbidities, but weights them based on severity. From this, we determined the score distribution of both the hospital score and of the ACCI of the population. The most frequent conditions present were also identified. Descriptive statistical analysis was performed to find central tendency and variance.
Results: Within the patient population, 5% had no comorbidities, 36.7% had between 1 and 4, 41.6% had between 5 and 9, and 16.8% had over 10 comorbid conditions (mean: 6; sd: 3.66; mode: 4) [Graph 1]. Regarding AACI scores, 5.5% of the patient population scored 0, 48% scored between 1 and 4, 43% scored between 5 and 9, and 4% scored above 10 (mean: 4.4; sd: 2.6; mode: 4) [Graph 2]. Out of the total patient population, 26% presented with one or more psychiatric issues. The most frequently occurring comorbid conditions according to the hospital criteria in this population were hypertension (N=1228), obesity (N=755), diabetes (N=583), anemia (N=533), and valve disorder (N=522).
Conclusion/Discussion: Using the described methodology, our analysis uncovered the presence of a high incidence of comorbidities in the BronxCare Orthopedics total joint replacement patient population. We had previously observed this but had not statistically confirmed it to date. Total joint arthroplasty is a common procedure performed worldwide and it is well known that comorbidities can influence outcomes. Additionally, it has been shown that safety net hospitals that serve patients of lower socioeconomic status, like BronxCare, have a patient population with increased comorbidities [5]. It is possible that the greater occurrences of comorbidities in total joint arthroplasty patients is in part due to the trend that this procedure is more commonly required in older and obese osteoarthritis patients. Both age and obesity are risk factors for other comorbidities such as hypertension and diabetes, which can impact surgical complications and outcomes and often require more extensive care.
Thus, regardless of the reason for increased rate of comorbidities, it is critical that joint replacement centers properly assess the pooled severity of comorbid conditions in their patient population for two main reasons. First, awareness of increased comorbidities dictates the care delivery process required to achieve quality outcomes. Spotlighting certain especially risk-associated comorbidities that were previously unknown also allows for the enactment of special protocols. Second, this information is useful to assist in calculating the total cost of procedures used for value-based healthcare payments.
As total joint arthroplasty becomes more common, gaining a better understanding of the severity of pooled comorbidities within a hospital’s respective patient population can lead to a more accurate assessment in developing efficacious payment systems adopted for the procedure [6]. It has been studied and declared that bundled payments for total joint payments are promising for keeping costs down and quality up, but require additional attention and risk adjustment of complexities for patients with high comorbidity burdens [7]. In our opinion it is critical that the Center for Medicare and Medicaid Services (CMS) and commercial payors include these risk adjustments for pooled comorbidities so that hospitals with medically complex patients, such as BronxCare and other safety net hospitals, are not penalized or disadvantaged [8].
Therefore, rather than stratifying individuals for individual payment, pooled comorbidity information can be used to better inform bundled payments for joint replacements based on severity of comorbidities of the population served by the center. Our suggestion is that joint replacement centers, especially hospitals similar to BronxCare across the nation, go through the exercise described and carried out here in order to understand the severity of the pooled comorbidities in their patients. Not only is it important for these surgical centers to be more aware of the health problems present in their patients, but they should also use this information to better assess total cost of procedures.
Stemless Anatomic Total Shoulder Arthroplasty with an Inlay Glenoid: Analysis of 90-Day and 2-Year Complications
-
Presenting author: Andrew D Posner
-
Additional authors: Matthew Anderson, Ian D. Hutchinson, Michael Kuna, Khusboo Desai, Joseph Zimmerman
Introduction: Big data studies of anatomic total shoulder arthroplasty (TSA) with a stemmed humeral implant and onlay glenoid have demonstrated concerning rates of serious postoperative adverse events: cumulatively up to 4.8% at 90 days. These events include death, pulmonary embolism, myocardial infarction, urinary or respiratory tract infection, and stroke. In addition, the rates of deep vein thromboses (DVT) range from 0.09% – 13%. Stemless TSA with an inlay glenoid improves glenoid stability and is relatively less invasive compared to conventional TSA, which may decrease complications. The aim of our study was to assess 90-day and 2-year complications of stemless inlay glenoid TSA.
Methods: A retrospective review of patients undergoing stemless anatomic TSA with an inlay glenoid was performed. Demographics and Charlson Comorbidity Index were used to determine preoperative patient physical status. Outcomes included hospital length of stay (LOS), adverse events at 30 days, 90 days, and 2 years postoperatively, and rates of readmission and revision.
Results: 46 shoulder arthroplasties in 45 patients, performed by a single surgeon, were identified. The mean age was 64.7 years (43 – 90). 30 patients (67%) were male. Mean Charlson Comorbidity Index was 3.04 (0 – 7). Mean follow up was 19.4 months (4.8 – 33.7). Mean LOS was 0.35 days (0 – 3), with 32 patients (70%) discharged the day of surgery. Rates of readmission and adverse events at 30 and 90 days postoperatively were 1/46 (2%). One patient developed a DVT on postoperative day 18 in their operative extremity. No early component failures or reoperations occurred. 16 of the 46 shoulders were available for 2 year follow up. For that cohort, mean follow up was 29.7 months (24.4 – 33.7), and there were no adverse events, periprosthetic fractures, signs of component loosening, hardware failures, or revisions.
Conclusions: In our patient cohort, stemless anatomic TSA with an inlay glenoid component appears to be safe and appropriate as an ambulatory procedure. Rates of early complications and DVTs are very low when compared to rates reported for conventional TSA. We will continue to follow this cohort, with future studies exploring patient reported outcomes, long term complications, and rates of reoperation.
Implementation of an Injury Prevention Program in NCAA Division I Athletics Reduces Injury-Related Healthcare Costs
-
Presenting author: Robert Parisien
-
Additional authors: Ali Farooqi, Marisa Pontillo, Brian Sennett
Introduction: Sports injuries impose a high economic burden on society. At the collegiate level, the estimated cost per year has been reported to be in the billions in the United States. Injury prevention programs are often assessed but only the magnitude of reduction of injuries, and there is little evidence on the associated reduction in costs if and when these programs are effective. The purpose of this study is to investigate the change in health care costs at a Division I university from sports injuries after the implementation of an injury prevention system.
Methods: Data was obtained from 3 academics years prior and 2 years after the implementation of an injury surveillance and prevention system (Sparta Science). This system utilizes a commercially available force plate system with dedicated software to assess kinematic variables gathered from vertical jumps; this information is used to flag athletes who are at higher risk of sustaining an injury, and guides strength and conditioning programs based on each athlete’s output. Twelve teams were designated as users of the Sparta Science System while sixteen teams were designated as non-users. Number of injuries and associated healthcare costs (surgery, clinic visits, imaging, and physical therapy) were compared between users and non-users.
Results: Total average annual injuries did not significantly change between users and non-users following implementation of the program (P = 0.50). However, users demonstrated a 23% reduction in clinic visits as compared to a 14% increase for non-users (P = 0.049). Users demonstrated a 13% reduction in associated healthcare encounters as compared to a 13% increase for non-users (P = 0.032). Overall healthcare costs changed significantly for both groups (P < 0.01), with an observed 19% decrease (2,456,154 to 1,978,799) for users and an 8% increase (1,177,542 to 1,270,846) for non-users. Costs related to associated healthcare encounters also decreased by 20% for users as compared to an increase of 39% for non-users (P = 0.027).
Conclusion: An injury prevention program utilizing force plate technology reduced healthcare costs associated with surgeries, clinic visits, and image requests. A decrease was also observed in the number of clinic visits and combined healthcare encounters, including surgeries, clinic visits, and image requests.
Post-operative advantages of use of tranexamic acid combined with local anesthesia at graft site in single bundle arthroscopic anterior cruciate ligament reconstruction
-
Presenting author: Saad Alghunaymi
-
Additional author: Mujeeb Ashraf, Omar Quraita AlAnazi
Introduction: The use of tranexamic acid ( TXA) is gaining popularity in Orthopaedic surgery.
We conducted at prospective randomized controlled trial in anterior cruciate ligament (ACL) reconstruction with combined use of TXA and local anesthetic ( LA) .
Methods: A cohort of 65 patients military personnel randomly selected through informed consent who had traumatic rupture of ACL requiring reconstruction. Exclusion criterion was concomitant ligament injury, meniscal injury requiring repair and clotting disorders. They were divided into a) TXA + LA b ) non TXA & LA groups. All procedures were “Day Surgery” performed by the same surgeon, anatomic placement of quadruple single bundle hamstring graft using the accessory antero-medial portal technique. 1 gram of TXA (regardless of weigh of the patient) was given intravenously by the anesthetist 15-30 minutes before inflation of the tourniquets and another dose of 1 gm was repeated 15-30 minutes before deflation of the tourniquet. A mixture of Lidocaine 1% and bupivacaine 0.25% was injected along the hamstrings. No post-operative deep vein thrombosis (DVT) prophylaxis was used in either groups.
Both the groups had same rehabilitation program selected by the senior author executed by experienced physical therapists. The same team reviewed the patients before discharge in “day surgical unit” using Visual Analog Score (VAS) for pain and a Set Criterion for analgesia requirement. Follow up was 10-12 days, at 6 weeks and at 3 months using similar protocols and clinical examination techniques. The patients were assessed for 1) Signs of deep vein thrombosis (DVT) “Well’s criterion” 2) Effusion by “Patellar stroke test”. 3) Bruises by “Harm Score” and 4) Range of motion (degrees) at all the visits.
Results: Pearson’s chi-squared, independent sample t-test and multivariable logistic regression model were used. Study found our technique is associated with reduced immediate post-operative effusion and pain leading to less use of narcotics and non-steroidal anti-inflammatory analgesia. It also reduced post-operative bruising and not associated with deep vein thrombosis. There was improved range of motion in tranexamic acid group.
Conclusions : This study showed that use of TXA +LA is associated with decrease use of post-operative analgesia, decrease haemarthrosis, less bruising , relatively improved early range of motion and no DVT.
Clinical Outcomes of Primary versus Revision Surgery using Arthroscopic Anatomic Glenoid Reconstruction for Anterior Shoulder Instability
-
Presenting author: Ryland Murphy
-
Additional authors: Ivan Wong, Sara Sparavalo, Jie Ma
Introduction: Revision surgeries after prior shoulder stabilization are known to have worse outcomes as compared to their primary counterparts. To date, no studies have looked at the utility of arthroscopic anatomic glenoid reconstruction (AAGR) as a revision surgery. The purpose of this study was to assess the clinical outcomes of primary versus revision AAGR for anterior shoulder instability with bone loss.
Methods: We performed a retrospective review on consecutive patients with prospectively collected data who underwent AAGR from 2012 to 2018. Patients who received AAGR for anterior shoulder instability with bone loss and had a minimum follow-up of two years were included. Exclusion criteria included patients with rotator cuff pathology, multidirectional instability and glenoid fractures. There were 68 patients (48 primary and 20 revision) who met inclusion/exclusion criteria. Our primary outcome was measured using the Western Ontario Shoulder Instability Index (WOSI) and Disabilities of Arm, Shoulder, Hand (DASH) scores. Secondary outcomes included post-operative complications and post-operative recurrent instability.
Results: The primary group showed a significant improvement in most-recent post-operative WOSI from 62.7 to 20.7 (P<0.001, α=0.05) and in DASH from 26.89 to 6.7 (p<0.001, α=0.05). The revision group also showed a significant improvement in WOSI from 71.5 to 34.6 (p<0.001, α=0.05) and in DASH from 39.5 to 17.0 (p<0.05, α=0.05). When comparing between groups, the revision group had worse WOSI scores (34.6) at most recent follow-up compared to the primary group (20.7); p<0.05. The most-recent DASH scores also showed the revision group (17.0) having worse outcomes than the primary group (6.7); p<0.05. Important to note that the minimal clinically important difference (MCID) was met for WOSI (MCID=10.4) but not DASH (MCID=10.83). There were no post-operative reports of instability in either group. For complications, one hardware failure (suture anchor) was seen in the primary group, and two hardware removals were seen in the revision group.
Conclusion: While patient reported scores indicated worse outcomes in the revision group, the significant clinical improvement in DASH and WOSI, along with the lack of recurrent instability provides evidence that AAGR is a suitable option for revision patients.
An Alternative 1-stage Exchange Arthroplasty Technique: for the Chronic Infected Total Hip
-
Presenting author: Keith Kotecki
-
Additional authors: Victor Hoang, Daniel LeCavalier, Michael S Bradford
Introduction: There are various algorithms for the treatment of prosthetic joint infections (PJI). Currently, a 2-stage hip exchange is considered the “gold standard” of care for treatment of chronic hip PJIs. However, there has been recent debate whether a 1- or 2-stage exchange offers the correct treatment. In a retrospective cohort study, the outcome of patients with chronic hip PJIs treated with our 1-stage exchange arthroplasty was analyzed.
Methods: Between January 2015 and January 2020, 8 patients underwent a 1-stage exchange hip arthroplasty by a single surgeon at a single institution for a chronically infected total hip arthroplasty (THA). Original diagnosis of PJI was made in accordance with the Modified Musculoskeletal Infection Society (MSIS) Criteria. The femoral stem was cemented with antibiotic-impregnated cement, the polyethylene acetabular liner was cemented directly onto the acetabular bone with antibiotic-impregnated cement. Of the 8 patients, 3 were female and 5 were male with a mean age of 70.5 years (SD 11.2, range 53-87).
Results: Six patients (75%) had infection eradication with retention of a stable implant and no additional surgery at a mean follow-up of 35.7 months (range 17-50). One patient (12.5%) underwent closed reduction for a dislocated THA at 1 month; however, this patient remained infection free at the most recent follow-up of 41 months. One patient (12.5%) who was the oldest patient (87 years) died 18 days post-operatively. Overall, all living patients (87.5%) retained their 1-stage exchange THA. One patient (12.5%, CI 95% 0.3-52.7) required additional surgery in the form of a closed reduction and 0 patients (0.0%, CI 95% 0.0-36.9) required additional open surgery.
Conclusion: Single-stage exchange arthroplasty with an antibiotic-impregnated cemented femoral stem and antibiotic- impregnated cemented polyethylene acetabular liner is a useful option for the treatment of chronic hip PJIs. Our study provides evidence that infection eradication and function preservation are possible using our 1-stage exchange arthroplasty technique in a chronically infected THA.
Calculating Glenoid Bone Loss Based on Glenoid Height Using Ipsilateral 3-Dimensional Computed Tomography
-
Presenting author: Johnny Rayes
-
Additional authors: Ivan Wong, Sara Sparavalo, Jie Ma, Jian Xu
Introduction: Anterior shoulder instability is a common problem in the young active population. It accounts for nearly 75% of all shoulder instability cases and the incidences in the general population of the United States and Canada are 8 per 100,000 person-years and 23.1 per 100,000 person-years, respectively. Glenoid reconstruction procedures continue to be the preferred treatment, especially in the presence of significant glenoid bone loss. Thus, one of the most important factors in surgical decision-making between a soft tissue stabilization or a glenoid bony reconstruction procedure is the amount of glenoid bone loss, and three-dimensional (3D) computed tomography (CT) reconstruction has become the gold standard imaging technique for glenoid measurement. Currently there is no consensus on the best technique for assessing glenoid size and amount of bone loss. The purpose of this study is to investigate the relationship between glenoid width and other morphologic parameters using three-dimensional (3D) computed tomography (CT) images of native shoulders to create a tool for assessing glenoid bone loss.
Methods: 102 glenoid images were obtained for patients who underwent contralateral shoulder glenoid reconstruction for anterior shoulder instability between 2012 and 2020. Demographic data was obtained including age, gender and BMI. The subjects were excluded if they had a prior history of ipsilateral shoulder instability, shoulder fractures, or bone tumors. The following glenoid parameters were measured: width (W), height (H), ratio (W/H), anteroposterior (AP) depth, superior-inferior (SI) depth and version. The shape of the glenoid was also classified into pear, inverted comma or oval. Data was analyzed based on gender and age. Simple logistic regression, Kruskal Wallis Rank tests and Fisher Exact tests were performed.
Results: There were 71 male and 25 females with a mean age of 39.74 ± 17.88 years. Pear morphotype accounted for most glenoid shapes (46%). The glenoid width was strongly correlated with the height (coefficient = 0.78) and a regression model equation was obtained: W (mm) = 3.4 + 0.68*H (mm). There was also strong correlation with gender (P<0.0001), age (P=0.0384), BMI (P<0.0001), glenoid shape (P=0.0036), height (P=0.0019), AP and SI depths (P<0.0001). Male gender was associated with higher measurement values for all parameters. Older age was significantly correlated with higher glenoid width values in both male and females group. (P=0.0015 and P=0.0104, respectively).
Conclusion: The native glenoid width can be easily estimated using solely the glenoid height. This is particularly important for surgical decision making when facing anterior or posterior glenoid defects in patients with shoulder instability.
Level of evidence: Level III, cross-sectional radiological study
MPFL Graft Tensioning to Treat Patellar Instability Related to Patella Alta: Dynamic Simulation
-
Presenting author: Travis Jones
-
Additional authors: Kerwyn Jones, John Elias
Introduction: Medial patellofemoral ligament (MPFL) reconstruction is a popular treatment for lateral patellar instability. For knees with patella alta, however, tibial tuberosity distalization is the most common approach due to concerns about graft tensioning. A MPFL graft is tensioned intra-operatively to prevent lateral subluxation without over-constraining the patella by allowing some translation. The purpose of this study is to analyze the effects of MPFL reconstruction on lateral tracking and cartilage pressure for knees with patella alta using dynamic simulation of knee function.
Methods: Knee function was simulated with 8 multibody dynamic simulation models constructed from 3.0 T MRI scans of subjects being treated for recurrent patellar instability validated from previous studies. Four models displayed patella alta; the remaining 4 models were made to reflect patella alta by lengthening the springs. Motion was simulated in a pre-operative condition and for three MPFL graft tensioning techniques (1.0, 0.5, and 0 patellar quadrants of lateral translation). The maximum bisect offset index during flexion was used as a measure of patellar instability and the maximum pressures applied to patellar cartilage (lateral, medial) as measures of the risk of overloading cartilage. Statistics were used to compare the parameters with significance set at p < 0.05.
Results: MPFL reconstruction with 0.5 and 0 quadrants of allowed lateral translation significantly decreased the maximum bisect offset index compared to the pre-operative condition, but not for 1.0 quadrants. MPFL reconstruction did not significantly influence the maximum pressure applied. The maximum post-operative bisect offset index was significantly correlated with the pre-operative bisect offset index for 1.0 and 0.5 quadrants of lateral translation allowed.
Conclusion: For knees with patella alta, the influence of MPFL reconstruction on patellar tracking varied with the allowed patellar translation during graft tensioning. None of the graft tensioning conditions significantly decreased the maximum lateral pressure or increased the medial cartilage pressure. The graft tensioning process for MPFL reconstruction typically allows some lateral patellar translation to avoid overconstraining the knee. For knees with patella alta, reducing the allowed lateral translation seems to limit maltracking without overconstraining the knee.
What is Driving Increased Numbers of Applications in the Orthopaedic Surgery Match and What are Applicant Opinions of the Process – An Anonymous Survey of 4th Year Applicants
-
Presenting author: Keegan T. Conry
-
Additional authors: Nicholas L. Kolodychuck, Michael T. Makowski, Steven B. Lippitt, Joseph N. Gabra, Gregory A. Vrabec
Introduction: The orthopaedic surgery residency Match is among the most competitive of any specialty. The Match rate has remained stable at approximately 77% despite increased numbers of applications submitted per applicant and received per program. No steps have been taken to address this issue at a system-wide level. This article aims to: 1) examine reasons for increased numbers of applications to orthopaedic surgery residency programs and 2) assess applicant perceptions of the Match process.
Methods: An IRB approved, anonymous, voluntary survey was sent to fourth year medical students who applied for an orthopaedic surgery residency position at our institution during the 2019-20 application cycle. Data was analyzed for associations and correlations between applicant characteristics and perceptions of the Match process.
Results: A total of 154/535 (28.8%) applicant survey responses were received. The median number of applications submitted was 95 per applicant. Applicants with higher self-rated strength of application submitted significantly fewer applications (p=0.0035.) Applicant USMLE Step 1 and 2 scores were significantly correlated with applicant self-rated strength (p<0.001.) No other objective measures of application strength were significantly associated with the number of applications submitted. The factor selected as most important in selecting programs was “geographic location,” which was chosen by 37.7% (58/154) of applicants. Applicants reported having a specific interest in a median of only 10 programs prior to submitting applications. Approximately 78.6% of applicants reported feeling “pressured” to apply to a greater number of programs than they desired. There was no association between the number of applications submitted and endorsing a feeling of pressure (p=0.726.) Additionally, 87.7% of applicants felt that the Match process requires reform. An application limit is supported by 76.0% (117/154) of applicants.
Conclusions: Applicants currently apply to more programs than they have interest in secondary to perceived pressure to submit more applications. There is overwhelming support amongst medical students for reform of the Match process, with most survey respondents favoring a universal application limit.
Onlay versus Inlay Prosthesis for Reverse Shoulder Arthroplasty: Retrospective Comparison of Radiographic and Clinical Outcomes
-
Presenting author: Teja Polisetty
-
Additional authors: Aaron Baessler, Jonathan Levy, Brian Badman
INTRODUCTION: Recent innovations in reverse shoulder arthroplasty (RSA) have presented two distinct humeral stem designs: an onlay system that rests above the anatomic neck and an inlay component that rests within the metaphysis. The purpose of this study is to compare clinical and radiographic outcomes between inlay and onlay-designed stems in lateral center of rotation RSA systems.
METHODS: A retrospective cohort study was performed on primary RSA patients treated for glenohumeral osteoarthritis with or without a rotator cuff tear and with a minimum 2-year follow-up. Patients were categorized based on treatment with an onlay or inlay humeral design and matched 1:1 by indication and age. Patient-reported outcome measures (PROMs), including the Simple Shoulder Test, American Shoulder and Elbow Surgeons, and Visual Analog Score for pain, as well as active motion were recorded. An Inlay-Onlay index assessed the degree of inset or offset in reference to the anatomic neck. Radiographic analysis focused on scapular notching, bone resorption, and acromion stress fractures.
Results A total of 92 patients participated in the 1:1 matched analysis, with similar age, gender, indication, follow-up length, and preoperative PROMs. There were no differences in all postoperative PROMs between groups. Greater tuberosity and calcar resorption occurred in 34 (74%) and 18 (39%) patients with an onlay-designed prosthesis, compared to 13 (28%) and 1 (2%) in the inlay group, respectively (p<0.0001). Both groups had low rates of scapular notching (p=1.0), while acromial fractures occurred in 6 patients with an onlay stem and in 4 patients with the inlay stem (p=0.73).
Conclusion: There were no differences in clinical outcomes and scapular notching following RSA with an onlay- or inlay-designed humeral stem prosthesis. Our study reports higher rates of both medial calcar and greater tuberosity resorption for onlay-style implants.
Comparison of CMCJ Resection Arthroplasty and Ligament Reconstruction with Tendon or Biosynthetic Collagen Interposition For the Management of Basal Thumb Arthritis
-
Presenting author: Agustin Herber
-
Additional authors: Jose J. Monsivais, MD, FACS
Introduction: The first carpometacarpal joint (CMCJ) of the thumb is a common site of osteoarthritis in the hand. Advanced progression can cause pain, progressive weakness, and deterioration of function . Surgical treatment can provide functional improvement and pain relief when conservative measures fail. Ligament Reconstruction with Tendon Interposition (LRTI) is an effective treatment for CMCJ arthritis, however, the use of an acellular dermal allograft (ADCA) as interposition material has not been extensively studied. This study compares the clinical outcomes of patients that underwent a modified CMCJ resection arthroplasty with LRTI with either the Flexor Carpi Radialis (FCR) tendon or (ADCA).
Methods: A retrospective review was conducted for 54 patients (60 extremities) between 23-87 years old with an Eaton-Little Stage II,III, IV trapeziometacarpal (TMC) or CMC joint arthritis. Each patient underwent a modified CMCJ Resection Arthroplasty with LRTI using either an ADCA or the FCR tendon. Preoperative and postoperative assessments were performed utilizing the Disability of the Arm, Shoulder, and Hand (DASH); Brief Pain Index (BPI), Wong Baker (WB) Scale, and numeric pain scale.
Results: Comparisons showed significant clinical and statistical differences between preoperative and postoperative measurements of the DASH, BPI, WB, and numerical pain scale regardless of interpositional type. However, there was no evidence of a statistically significant effect among the study outcome variables with regard to type of interposition used. (p-value>.05)
Conclusion: Our results suggest that the ADCA is a highly-effective alternative interpositional material for patients undergoing LRTI for CMCJ arthritis when compared to the use of the FCR tendon.
Complete Capsule Closure Provides Clinically Significant Outcome Improvement and Higher Survivorship After Hip Arthroscopy at Minimum 5-year Follow-up
-
Presenting author: Laura M. Krivicich
-
Additional authors: Edward Beck, Benedict Nwachukwu, Jorge Chahla, Kyleen Jan, Ian Clapp, Anirudh Gowd, Shane J Nho
Introduction: Previous studies have demonstrated the benefits of complete capsular repair during hip arthroscopy for femoroacetabular impingement syndrome (FAIS). However, the long-term effect of complete versus partial capsular closure of T-capsulotomies on achieving meaningful clinical outcomes are unknown.
Purpose: To compare the rates of reaching threshold hip-specific outcome scores for achieving the minimal clinically important difference (MCID) and Patient Acceptable Symptomatic State (PASS) between patients who had partial vs complete T-capsulotomy repair, and to identify the failure rates in each group 5-years after undergoing hip arthroscopy for FAIS.
Methods: Data from consecutive patients undergoing hip arthroscopy for FAIS by a single fellowship trained surgeon from 01/2011 to 03/2013 were collected and analyzed. Baseline data, hip-specific outcomes, and clinical failure rates were recorded at 5-years minimum postoperatively. Patient receiving partial T-capsulotomy repair matched 1:3 by age, BMI, and sex to patients with complete T- capsulotomy repair. Threshold scores for achieving MCID and PASS were calculated and compared between the two groups. Additionally, revisions and conversion to total hip arthroplasty (THA) were compared between the groups.
Results: A total of 379 patients were available for analysis (39 partial and 340 complete repairs), with 100 patients included in the matching (25 partial and 75 complete repair group). Analysis demonstrated that the complete repair group had significantly higher functional score and lower pain score averages as compared to the partial repair group (p<0.05 for all). A total of 65(95.6%) complete repair patients achieved MCID on at least one outcome measure vs. 18(78.3%) patients with partial repair (p=0.04). A total of 69(92%) complete repair patients achieved PASS on at least one outcome measure vs 18(72%) of patients with partial repair (p=0.017). Of the 39 partial repair patients, 35.9%(n=14) underwent revision or THA conversion; compared to 2.9%(n=10) in the overall cohort
Conclusion: At minimum five year follow-up, patients with complete capsular closure after hip arthroscopy for FAIS demonstrate superior long-term achieve higher rates of meaningful clinical success when compared to patients with partial capsular closure. Furthermore, patients with partial capsular repair undergo revision or conversion to THA at high rates.
Opioid Use and Complication Rates after Unicompartmental Knee Arthroplasty: A PearlDiver Study of Medicare Advantage Patients
-
Presenting author: Jack M. Ayres
-
Additional authors: Brandon L. Morris, Armin Tarakemeh, Scott Mullen, J. Paul Schroeppel, Bryan G. Vopat
Introduction: Unicompartmental knee arthroplasty (UKA) represents a surgical treatment option for patients who present with unicompartmental knee osteoarthritis (OA). Implant utilization, postoperative complication rates, opioid usage and implant survivability of UKA is not well-reported within the Medicare population. The purpose of this study is to analyze UKA practice patterns in Medicare Advantage patients and analyze differences in outcomes between UKA and TKA.
Methods: The PearlDiver Application was used to analyze Medicare Advantage patients in the Humana Claims dataset who underwent UKA and compare them to patients who underwent TKA. Patients who underwent UKA and TKA were identified by respective CPT codes. Complication rates were determined by ICD-9 and ICD-10 codes. Opioid use was analyzed by comparing the total number of days patients were prescribed opioids postoperatively. Statistical analysis included qualitative analysis and logistic regression. Implant survivability was defined as conversion to TKA.
Results: 24.27 million patients between 2007 and 2017 were reviewed in the Humana Claims dataset, 7,808 UKA and 150,680 TKA patients were identified. 4.59% of UKA patients underwent conversion to TKA with average time between surgical procedures at 817 days. Overall 8-year UKA implant survival was 87.7% (95% CI [0.861,0.894]). Revision surgery was more common in the UKA group (3.88%) than the TKA group (2.60%) (p<0.01, RR = 1.49, 95% CI = [1.33, 1.67]). A statistically significant difference in opioid use was observed, with the mean prescribing days of opioid use at 186.1 days after TKA and 144.7 days after UKA (p < 0.01, Δ = 41.1, 95% CI = [30.41, 52.39]). Complications occurred at a higher rate in most categories in the TKA group compared to the UKA group. This includes complications such as DVT (p=0.022) and cardiac arrest (p=0.008), as well as wound dehiscence (p <0.001).
Conclusion: Unicompartmental knee arthroplasty represents an increasingly utilized treatment for osteoarthritis in the Medicare population. Unicompartmental knee arthroplasty in Medicare patients may be comparatively advantageous to total knee arthroplasty due to reduced opioid use and complication rates after surgery.
Total Joint Arthroplasty Outcomes in the Outpatient Ambulatory Surgery Center Setting
-
Presenting author: Jeff Almand
-
Additional authors: Ben Stronach, Doug Parsell, Kerk Mehrle, Louis Francis McIntyre
Introduction: There has been a rapid transition to outpatient total joint arthroplasty (TJA) in the ambulatory surgery center (ASC) setting with only early reports on outcomes and complications. This study presents patient reported outcomes (PRO) and complication rates of outpatient TJA in the ASC.
Methods: All patients undergoing outpatient TJA (hip, total and partial knee arthroplasty) from 2016-2019 were enrolled. A validated selection tool identified patients amenable for outpatient TJA. A rapid recovery pathway was utilized with same day to home discharge with standardized post-operative therapy. PRO (HOOS, KOOS and VR-12) and complications were collected at routine follow up (2 weeks, 6 weeks, 3 and 6 months, then annually).
Results: There were 3664 procedures performed (1578 partial knee, 1179 total knee, 907 total hip arthroplasties). 2036 were involved in a bundled payment contract with a private insurer. Average length of follow-up was six months (2 weeks to one year). 3,444 (94%) were same day discharge and 220 (6%) required overnight stay. There was statistically significant improvement in hip scores (HOOS 31.2 to 82.2, VR-12 MCS 48.7 to 54.5, VR-12 PCS 28.6 to 45.0, p<0.001) from baseline to post-operative 6 month follow up with similar findings in the knee (KOOS 37.3 to 73.1, VR-12 MCS 51.0 to 54.1 and VR-12 PCS 30.4 to 42.4, p<0.001). There were 18 (0.6%) readmissions and 43 (1.4%) emergency department visits. There were 109 (2.9%) complications including 11 (0.36%) manipulations for arthrofibrosis, 12 (0.4%) venous thromboemboli, 18 (0.6%) other medical, 18 (0.6%) wound issues, 9 (0.3%) infection, 14 (0.45%) superficial infection, and 27 (0.9%) pain control issues.
Conclusion: Outpatient TJA in the ASC is safe and effective with PROs and complication rates that compare favorably to inpatient procedures. The migration of TJA to the outpatient should be encouraged in appropriately selected patients.
Return to Sport and Weightlifting Analysis Following Distal Biceps Tendon Repair
-
Presenting author: Anirudh Gowd
-
Additional author: Joseph Liu, Bhargavi Maheshwer, Grant H. Garcia, Edward C Beck, Mark Cohen, Gregory Nicholson, Brian J. Cole, Nikhil N. Verma
Background: Rupture of the distal biceps tendon is an increasingly frequent injury sustained predominantly by middle aged males. Despite the prevalence of sport in this age group, little is known regarding return to sport outcomes following surgery.
Purpose: To evaluate and quantify return to sport and lifting following repair of the distal biceps tendon.
Methods: Patients undergoing distal biceps tendon repair (DBR) between January 2015 and January 2017 were contacted electronically and via telephone to administer a previously validated and standard return to sport survey. Patients self-reported pre-injury and current level of sport and activity as well as pre-injury and current level of select weightlifts.
Results: A total of 77/124 were available for follow-up (62.1%). Of these patients, 61 endorsed preoperative sport, and were included for analysis. Average follow-up was 38.7 ± 6.7 months. The mean age at surgery was 47.5 ± 8.8 years, and mean BMI was 30.3 ± 5.1. The dominant side was affected in 25 of 61 cases. Of the 61 included patients, 57 (93.4%) were able to return to sport at any level. Forty of the patients (65.6%) were able to return to sport at same/higher intensity.
Mean time to return to sport was 6.0 ± 2.8 months. Days from injury to surgery (OR: 0.999, 95% CI: 0.998 – 0.999), suture anchor fixation in comparison to suture button (OR: 0.602, 95% CI: 0.427 – 0.850), and dominant side surgery (OR: 0.749, 95% CI: 0.582 – 0.963) were associated with a decreased likelihood to return to sport at same/higher level of duty. Single-sided incision in comparison to double (OR: 5.209, 95% CI: 1.239 – 20.903) and dominant side surgery (OR: 6.370, 95% CI: 1.639 – 24.762) were associated with increased duration to return to sport.
Conclusion: Distal biceps tendon rupture is a devastating injury, although, patients can expect high levels of return to sport following DBR. It is important to counsel patient expectations with the results of this study as there is a small but appreciable decrease in strength when compared to pre-injury levels.
Twitter Use Amongst Orthopedic Surgery Journals: Does a Tweet Increase Citations?
-
Presenting author: Arjun Verma
-
Additional authors: Osman Kazan, PhD, Mohammed Asad Khalid, Jie Chen
Introduction: Twitter is a rapidly growing means of social-media distribution for research, and the relationship between Twitter use and research impact is not established. The purpose of this study is to investigate the impact of Twitter on research citation rate across major orthopedic publications.
Methods: Articles published in ten major orthopedic journals between January 2018 and December 2018 were analyzed using the Altmetric Bookmarklet. Multiple linear regression analyses and paired t-tests were used to determine (1) the relationship between Twitter use of different sources and number of citations, (2) differences in citations and Altmetric Attention Score (AAS) for tweeted versus non-tweeted articles, and (3) the correlation between journal impact factor and average number of monthly tweets.
Results: A total of 2916 articles were included for analysis at an average of 26 months after publication. The mean AAS was 9.7 (SD, 45.1, range; 0-1125) and mean citation rate was 6.4 (SD, 8.5; range, 0-166). Impact factor was strongly positively correlated with average monthly tweets (r2= 0.77). Articles with more tweets had significantly higher citations for all journals analyzed (p<0.05). Tweets sent by the author/department had the greatest impact on future citations (multiplier =1.1, p<0.01). Tweets by news outlets had a smaller positive effect on citations (multiplier=0.3, p<0.01). Tweets by journal or other sources did not have a significant impact on citations. There was significant variance amongst the individual journals impact on citations. Tweets sent by Arthroscopy (multiplier=2, p<0.01) and JPO (multiplier= 6.1, p<0.01) had high impacts compared to other journals.
Conclusion: Articles with a higher number of tweets have a higher number of citations 26 months after publication across the 10 journals studied. Non-tweeted articles received much lower citations (mean 2.56) compared to tweeted article (mean 8.51). This result was independent of their date of publishing and statistically significant (p<0.01). Journals with higher impact factors were also found to have a higher average number of tweets. The citation rate across all journals was most impacted by tweets by department/author, and less by tweets by news outlets, journal, or other sources. However, there was a variation amongst journals in their twitter impact on citations.
The Effect of Recovery Period on Injury Patterns and Trends among Athletes in the National Football League
-
Presenting author: Akhil Sharma
-
Additional author: Amanda N. Fletcher, Jay K. Shah, Craig C. Akoh, Selene G. Parekh
Introduction: While there are many isolated studies on NFL injuries, limited data exists in contributing to a comprehensive understanding of these injury patterns and trends. This study aimed to determine the relationship of recovery period length on overall injury patterns (rates and incidence) for athletes in the National Football League.
Methods: Official NFL gamebooks were queried from 2011 to 2015, and each in-game injury was analyzed for all regular season games. Data included athlete name, position, season, week, date, weekday, teams, and injured body part. ANOVA testing determined statistical significance of injury rates across weekdays, season weeks, and positions.
Results: A total of 27,712 injuries were analyzed. On average, 21.4 (8.6; 20.9-21.9) injuries were sustained per game on Sunday, 18.2 (6.9; 16.7-19.7) on Monday, and 21.7 (6.9; 20.2-23.3) on Thursday. The difference between Sunday and Thursday games was negligible (p=0.9264), while Monday games had fewer injuries than Sundays (p=0.0028) and Thursdays (p=0.0214). There was no difference in number of injuries each team sustained on Thursday compared to the week prior to (10.8 versus 10.8; p= 0.4971) or week after (10.8 versus 10.7; p=0.7315) its Thursday game. Among positions, defensive linemen (p=0.0036), linebackers (p=0.0297), skilled running positions (p=0.0099), and wide receivers (p=0.0259) sustained fewer injuries on Mondays compared to Sundays, but no statistical difference existed between Thursdays and Sundays.
Conclusion: Our analysis indicates that shortened recovery before Thursday games does not have significant effect on injury rates compared to Sunday games, while the additional rest day before Monday games correlates to fewer injuries. Additionally, there was no residual effect of reduced rest period affecting players’ injury risk the following week. A general trend of greater injury rates occurs as the season progresses; the incidence of injury during the final week of the season is nearly double that of the first. Interestingly, although injury rates did not differ among positions between Thursdays and Sundays, defensive positions and offensive ball-carrier positions saw reduced injuries on Mondays.
Outcomes of Obstructive Sleep Apnea Patients Undergoing Rotator Cuff Repair
-
Presenting author: Andres Barandiaran
-
Additional authors: Jonathan Bravman, Adam Seidl, Rachel Frank, Eric McCarty
Introduction: Obstructive sleep apnea (OSA) prevalence in the general adult population is estimated to be 6-17%, and as high as 49% in older adults. These patients are at 45-59% greater risk of postoperative complications, such as hypoxemia, acute hypercapnia, as well as hyperalgesia, due to higher levels of inflammatory markers compared to patients without OSA. While older adults are at higher risk of OSA, they are also at a higher risk of having a rotator cuff tear (RCT). Previous research has shown 30% of adults >60 years and 62% of adults >80 years have a RCT. Given the prevalence of OSA and RCT in older adults, OSA may negatively affect parameters of mental, physical health, and shoulder function in patients recovering from rotator cuff repair (RCR). The purpose of this study was to compare patient reported outcomes (PROs) between OSA patients and controls that underwent RCR.
Methods: A retrospective review of patients who underwent RCR by 5 fellowship-trained orthopedic surgeons between 2014 and 2019 was performed. Patient medical history was screened for a diagnosis of OSA or deemed at high risk by STOP BANG questionnaire. All patients were asked to complete PROs pre- operatively, at 3, and 6 months post-operatively. A mixed-model ANOVA was performed with age and BMI as covariates due to higher age and BMI increasing OSA risk as well as being associated with worse outcomes following RCR.
Results: Data from 91 (44 female) control and 89 (24 female) OSA patients were available for analysis. As expected, as OSA risk increases with male sex, higher BMI, and age; mean BMI (25.1 ± 4.0 kg/m2 vs. 30.4 ± 5.1 kg/m2), age (57.7 ± 11.8 years vs. 61.7 ± 8.7 years), were significantly higher in the OSA group (p<0.05). In addition, there were also significantly less females in the OSA group compared to control (p<0.05). There was no significant effect of OSA for VAS, VR-12 mental scores, and SANE (p>0.05). However, OSA patients had a significantly lower ASES score compared to control (66.79 ± 21.03 vs. 60.95 ± 21.70, respectively, p<0.05) when adjusted for age and BMI, but no interaction effect with time (p>0.05). In contrast, VR-12 physical scores showed a significant interaction effect of time and OSA condition, when adjusted for age and BMI. More specifically, control patients at both 3 months (41.0 ± 1.0 vs. 37.1 ± 1.0, p<0.05) and 6 months (49.2 ± 1.2 vs. 42.3 ± 1.3, p<0.05) reported better physical health post-RCR compared to OSA patients. Lastly, the difference in 6-month VR-12 physical scores between groups met minimal clinical important difference (MCID) criteria.
Conclusion: The findings of our study suggest PROs related to shoulder pain and mental health among OSA patients that underwent RCR are not significantly different from healthy patients. However, our results show despite controlling for age and BMI, patients with OSA report significantly worse physical health post- operatively and shoulder function compared to healthy patients.
The Fate of Patients Undergoing ACI/MACI Biopsy
-
Presenting author: Avi Robinson
-
Additional author: Hannah Bradsell, Andres Barandiaran, Brian Cole, Armando Vidal, Rachel Frank
Introduction: Focal chondral defects of the knee can be successfully treated with Matrix-Induced Autologous Chondrocyte Implantation (MACI), a surgical technique that requires two separate surgeries, including one surgery (biopsy) to assess the defect and harvest healthy articular cartilage, and a second surgery to perform the cartilage transplantation. In some cases, patients do not progress to the second surgery. The number of patients not undergoing MACI transplant following biopsy remains unclear. The purpose of this study was to determine the clinical outcomes of patients undergoing MACI biopsy, including conversion rate to MACI transplantation and clinical outcomes following both initial biopsy and definitive treatment.
Methods: A retrospective review of all patients who underwent MACI (or ACI) biopsy by two board-certified, fellowship-trained orthopaedic surgeons between January 2013 and January 2018 was performed. All patients were invited for a clinical follow-up evaluation at a minimum of 2-years following surgery. Preoperative data, intraoperative data, and postoperative outcomes were assessed. Conversion rate from biopsy to transplantation was calculated, and reasons for not undergoing transplantation were analyzed. Descriptive statistical analysis was performed.
Results: A total of 46 (63% female) patients with a mean age of 30.0 ± 10.5 years and mean body mass index of 25.3 ± 5.1 kg/m2 underwent MACI/ACI biopsy during the study period. Of these 46 patients, 16 underwent cartilage restoration surgery, for an overall transplantation rate of 32.7%. Of the 16 patients undergoing transplantation, 11 underwent one or more concomitant procedures including realignment osteotomy (N=6), platelet rich plasma augmentation (N=1), meniscus repair/meniscectomy (N=3), ligament reconstruction (N=1), and hardware removal (N=3). Of these 16 patients, 62.5% underwent MACI/ACI transplant and 37.5% underwent osteochondral allograft (OCA) transplantation at an average 7.3 ± 7.7 months following biopsy. The reoperation rate following transplantation was 25% (N= 2 following MACI/ACI and N=2 following OCA) at an average 11.7 ± 3.4 months after transplantation surgery. There were no complications reported for all patients.
Discussion: Patients undergoing chondral biopsy for future MACI/ACI transplantation progress to future cartilage restoration surgery 32.7% of the time, suggesting arthroscopy with debridement/chondroplasty of pathology in the knee compartment at the time of biopsy may be a sufficient option to improve function and reduce pain in patients with knee focal cartilage defects.
Physician Burnout: Understanding the Risk Factors, Warning Signs and Prevention Strategies. How Stigma can lead to Tragedy
- Presenting author: Eric Muehlbauer, MJ, CAE
Introduction: The commonly accepted definition of burnout is a state of emotional, mental and physical exhaustion caused by excessive and prolonged stress. It is a chronic process of energy expenditure without appropriate periods of recovery. H. Freudberger, ,1974
Methods: A study published about 5 years ago was conducted by Mayo Clinic and Stanford University. (Burnout and Satisfaction With Work-Life Balance Among US Physicians Relative to the General US Population - Tait D. Shanafelt, MD; Sonja Boone, MD; Litjen Tan, PhD; Lotte N. Dyrbye, MD, MHPE.) 27 276 physicians received an invitation to participate and 7288 (26.7%) completed the survey. In 2011, 45% of U.S. physicians had at least one symptom of professional burnout, according to a study from the Department of Medicine Program on Physician Well-Being at Mayo Clinic. Per the recent Mayo/Stanford study that number rose to 54% in 2014. This number might increase going forward.
There are many reason for this. First, projections from the Department of Health and Human Services suggest that by 2020, the U.S. will face a shortage of 50,000 physicians. The age wave is upon and amore people are utilizing medical services and demanding results that ensure their quality of life. So, the demands on physician time and attention is only going to increase. As burnout symptoms increase the quality of service declines. “The rising tide of burnout, coupled with its effects on quality of care and access, make burnout a major threat to the health care delivery system,” - Tait Shanafelt. “We tell physicians to get more sleep, eat more granola, do yoga, and take better care of yourself. These efforts are well intentioned,” says Shanafelt. but “the message to physicians, however, is that you are the problem, and you need to toughen up.” This is an unfortunate message to deliver to a field that is already under tremendous stress. Shanafelt argues that “We need to stop blaming individuals and treat physician burnout as a system issue” Quality care is at issue. “If it affects half our physicians, it is indirectly affecting half our patients.”
Results: 8 Burnout warning signs: 1) Yelling; 2) Using inappropriate or abusive language; 3) violating Physical boundary; 4) Making threatening gestures; 5) vocalizing insulting on others or shaming or using abusive language; 6) using intimidation; 7) slamming or throwing items; 8) being physically aggressive. 9 Passive Aggressive Warning signs: 1) Hostile avoidance; 3) Inappropriate jokes – with racial, sexual, gender-based, or religious slurs, or jokes about physical appearance; 4) Intense sarcasm; 5) Implicit threats; 6) Impatience and irritability; 7) Condescending or character defiling comments about others; 8) soft speech; 9) Slowed response or lack of availability for professional communications about patient care.
Conclusions: The support network that physicians have is often limited due to the amount of time spent working. There are perceived internal and external stigmas to having any mental health issues. Due to these stigmas no one wants to admit they have a problem. There could also simply be a lack of self-awareness that they are burned out (be unaware of the symptoms) and/or could simply not accept that they are burned out. There is often a lack of connectedness to one’s job, spouse, friends and a sense of alienation. Again, due to the long work hours there could be lack of a support network. They might fear assaults to their medical license, hospital privileges or insurance so they refuse to see anyone because there is a lack of a safe environment to get treatment
Emergency Department Visits and Admissions after Total Joint Replacement in a Closed Urban Setting
-
Presenting author: Julia Fisher
-
Additional author: Ira Kirschenbaum
Introduction: Each year, nearly 1 million hip and knee replacements are performed in the United States. The American Academy of Orthopedic Surgeons demonstrates the low complication and high improvement rates after joint replacement surgery, but a close following of patients post-surgery is necessary to take into account possible complications or negative outcomes that may not initially be associated with the joint replacements. Further, the Comprehensive Care for Joint Replacement (CJR) model of payment bundling calls for precise inspection of emergency department (ED) visits and hospital admissions of patients within the 90 days following joint replacement surgery to determine if any visits or admissions could have been prevented. The goal of this study was to determine how often joint replacement patients at Bronxcare Health System (BCHS), a community hospital serving primarily the South and Central Bronx, visited the ED or were admitted to the hospital within 30 days of surgery and within the CJR defined period of 90 days post-surgery. Knowledge of these rates is necessary to achieve joint replacement care delivery of the highest quality and efficiency, and to prevent unnecessary hospital visits and admissions, and adverse outcomes.
Methods: Patients who underwent joint replacement surgeries between 2016 and 2019 at BCHS were examined for ED visits and hospital admissions within 30 and 90 days of their surgeries. All visits and admissions that fit the CJR model criteria, including non-orthopedic visits and admissions, were considered. Both emergency hospital stays and elective surgical procedures were included in the admissions category. Patients who did not go to the ED or were not admitted to the hospital within 90 days of their surgeries AND did not have an orthopedic outpatient visit at a date later than 90 days from their surgeries were excluded from the study to ensure that ED visits and admissions at other hospitals were accounted for.
Results: Of 445 patients, 152 (34%) either visited the ED or were admitted to the hospital within 90 days of joint replacement surgery. 99 patients (22%) visited the ED and 70 (16%) were admitted to the hospital within 90 days of surgery. Of those same 445 patients, 83 patients (19%) either visited the ED or were admitted to the hospital within 30 days of joint replacement surgery. 58 (13%) visited the ED and 28 (6%) were admitted to the hospital within 30 days of surgery.
Conclusion: ED visits and hospital admissions are frequent following hip and knee replacement surgeries. Further analysis of the reasons for those visits and admissions, and how rates differ among those with various comorbidities and of different social factors, is necessary to determine which of those visits and admissions were ultimately preventable, and how to reduce the number of visits and admissions following joint replacement surgery in the future.
Reverse Total Shoulder Arthroplasty for Patients with Minimal Pre-Operative Pain: A Matched Cohort Analysis
-
Presenting author: Gagan Grewal
-
Additional authors: Teja Polisetty, Ryan Colley, Andrew Malarkey, Jonathan Levy
Introduction: Profound improvements in function have been described for patients following reverse shoulder arthroplasty (RSA). Previous studies have demonstrated young age, high pre-operative function, and neurologic dysfunction to be predictors of poor functional improvement. However, there is no study to date that has focused on patients electing to have RSA for function more than pain. The purpose of this study is to compare the outcomes of RSA for patients with minimal pre-operative pain with those that have higher baseline pain.
Methods: A retrospective matched-cohort study was performed on RSA patients treated by a single surgeon with a minimum 2-years follow-up. Patients with at least moderate baseline pain (“Function+Pain”), pre-defined by existing literature as a Visual Analog Scale (VAS) pain score > 3, were matched 3:1 based on gender, indication, and age to those with a minimal pain with VAS score ≤ 3 (“Function”). Patient reported outcome measures (PROMs), active range of motion, and overall satisfaction were compared. The percent of maximal improvement in outcomes and the proportion of patients exceeding the established threshold that predicts an excellent satisfaction were also compared.
Results: A total of 260 patients (195 Function+Pain, 65 Function) were selected for matched analysis with a similar gender distribution, mean age of 73.1 years, and mean follow-up of 50 months. Patients in both groups showed no differences in most recent post-operative function, overall improvement in functional scores, and active motion (p>0.05). However, pain scores improved only for patients with at least moderate baseline pain (p<0.0001). Patient satisfaction was significantly different (p=0.035), as 10.8% of patients who elected to have RSA for function were unsatisfied. The Function cohort also had worse percent of maximal SST (p=0.034) and ASES (p<0.0001) improvement, and a lower proportion of these patients exceeded the threshold in percent of maximal improvement that predicts an “excellent” outcome (p<0.0001).
Conclusion: RSA patients with minimal pre-operative pain achieve significant improvements in function and motion similar to those who choose to have RSA for both pain and function, but are less satisfied and are less likely to achieve an “excellent” outcome. Patients electing to proceed with RSA with minimal pain should be counseled accordingly.
High Complication Rates for Morbidly Obese Patients After Total Hip Arthroplasty in a Predominantly African American and Hispanic Population
-
Presenting author: Benjamin J Levens
-
Additional author: Eli Kamara
Introduction: High body mass index (BMI) is associated with an increased risk of post-operative complications. Patients with high BMI are more likely to have osteoarthritis necessitating total joint replacement. The purpose of this study is to investigate how morbid obesity (BMI >40) effects post- operative complications after Total Hip Arthroplasty (THA) in a racially and ethnically diverse population.
Methods: A retrospective chart review of patients who received primary THA at a high volume, academic center between 2016 and 2019. Demographics, medical complications and surgical complications were collected by chart review. The primary outcome is return to operating room (RTOR) for any reason, secondary outcomes are RTOR for infection or revision. BMI of 40 was defined as the cut off between cohorts. Patient characteristic variables and comorbidities were compared between cohorts. Cox Proportional Hazards Model was used to compare Time to Outcome Hazard Ratios.
Results: 1351 THA cases (1128 patients) were included in the study (BMI <40: 1202, BMI >40: 149). The average BMI was 29.6 and 43.6 for BMI<40 and BMI>40 cohorts, respectively. Overall, 44% were African American, 34% Hispanic, and 22% Caucasian. The BMI>40 cohort was comprised of a higher percentage of African Americans (55 vs. 43%, p<0.01). BMI>40 group had a higher risk for prolonged hospital stay with 66% of the cohort staying 3 or more days post-operatively (p<0.01). The Hazard Ratio for RTOR for any reason was three-fold higher in the BMI >40 cohort (3.10, p<0.01) with over four-fold increased risk of 2 stage revision for Periprosthetic Joint Infection (PJI) (4.65, p=0.01. The Adjusted Hazard Ratio remained significant for RTOR for any reason (2.23, p=0.02) and 2 stage revision for PJI (3.47, p=0.04).
Conclusion: THA in morbidly obese patients in a majority African American/Hispanic population resulted in significantly higher likelihood of RTOR and 2 stage revision compared to BMI <40. The results of this study align with the preexisting research that high BMI is associated with poor outcomes following THA, while focusing on a minority population. Further research is needed on the benefit of arthroplasty in morbidly obese patients and to determine if the risk associated with high BMI necessitates an absolute cut off.
Increased 90 Day Mortality and Morbidity in Recovering Elective Arthroplasty Patients During the 2019 Coronavirus Pandemic in New York City
-
Presenting author: Megan M. Mizera
-
Additional author: Zeynep Seref-Ferlengez, Sun Jin Kim, Zachary Sharfman, Anna Tarasova, Evan Mostafa, Eli Kamara
Introduction: On March 16th, 2020, amidst the evolving SARS-CoV-2 (COVID-19) pandemic, there were executive orders from the local government to stop all elective surgeries in New York City (NYC). In this study we report the 90-day mortality and complications in patients who underwent primary arthroplasty in close proximity to the COVID-19 pandemic at a single academic medical center located in Bronx, New York.
Methods: We performed a retrospective cohort study including primary arthroplasty patients that underwent surgery between December 1st 2019 and March 16th 2020 at a single arthroplasty department in Bronx, New York. This cohort was compared to patients during the same operative season in 2019. Procedures eligible for inclusion were primary total hip and knee arthroplasty. Cohorts were compared using Wilcoxon Sum Rank test and categorical variables were compared using chi-squared or Fisher Exact tests.
Results: The sample size for the 2020 and 2019 cohort included 359 and 410, respectively.
For baseline characteristics, patient preoperative health and length of stay there was no significant difference between the two cohorts except the prevalence of diabetes. The 2020 cohort had statistically significant higher rates of Pneumonia (2.8% vs 0.7%, p=0.03), readmission rate (9.5% vs. 5.4%, p=0.03), pulmonary embolism (1.7% vs 0.2%, p=0.04) and 90-day mortality (1.1% vs 0%, p=0.03). The 2020 cohort also had increased rates for deep vein thrombosis (1.1% vs 0.7%, P=0.71), cardiac complications (1.9% vs 0.5%, p=0.06) and no change in ER visits (14.5% vs 11.7%, p=0.28). There were 7 confirmed SARS-CoV-2 patients in the 2020 cohort and one mortality among the group.
Conclusion: This study demonstrates patients who underwent primary arthroplasty procedures at our institution in proximity to the COVID-19 pandemic experienced a statistically significant increase in mortality, pneumonia, pulmonary embolism and readmission rate when compared to historic controls. As elective procedures resume in the setting of the ongoing pandemic, providers and patients should be aware of these increased risks when resuming elective procedures.
Pericapsular Nerve Group Block in Total Hip Arthroplasty Reduces Peri-operative Complications
-
Presenting author: Michael Nammour
-
Additional authors: Michael Warren, Bhumit Desai, Colin Carroll, Nicholas Newcomb, Matthew Patterson, Leslie Thomas, George Chimento
Introduction: Patient controlled epidural analgesia (PCEA) provides excellent post-operative analgesia following posterior approach total hip arthroplasty (THA). The Pericapsular Nerve Group block (PENG), coupled with a spinal anesthetic is an alternative method of providing pain control without the associated side effects of PCEA. The purpose of this study is to determine if the PENG block can provide satisfactory pain control without the side effects associated with PCEA.
Methods: 100 consecutive patients who received a single shot PENG block and spinal anesthesia were retrospectively compared to the previous 100 patients who had PCEA, which was continued until 0630 post-op day 1. Primary outcome measures were Visual Analgesia Scores (VAS) and opioid requirements measured in Morphine milliequivalents (Meq). Secondary outcomes were incidence of urinary tract infection (UTI), urinary retention, falls, and length of stay (LOS). Statistical analysis involved student’s t test and multivariate linear regression with α = 0.05.
Results: The groups were similar demographically. Pain was well controlled in both groups, however the PCEA group demonstrated decreased Meq and VAS in the PACU (p < .001, p < .001) and at 12 hours (p <.001, p < .001), while the epidural was in place. VAS scores in the PENG group progressively decreased from 5.07 in PACU, 4.84 at 12 hours, and 4.07 at 24 hours post-op. VAS scores in the PCEA group were 2.55 in PACU, 2.06 at 12 hours, and 3.80 at 24 hours. There was no difference in Meq and VAS at 24 hours, once the epidural had been discontinued (p = .056, p = .357), and in LOS (p = .359). There was no difference in incidence of urinary retention (p = 1.0). The PENG group demonstrated less UTIs at two weeks post-operative (p < .001) and less inpatient falls at 24-hours post-operative (p = .044).
Conclusion: As expected, there was less pain in the PCEA group while the epidural was in place, however, the pain was well controlled in the PENG group and there was no difference once the epidural was discontinued. With less UTIs and falls, the PENG block coupled with spinal anesthetic may be a preferable option in patients undergoing posterior approach THA.
Medial Patellofemoral Ligament Reconstruction With and Without Mersilene Tape Augmentation
-
Presenting author: Taylor Hobson
-
Additional authors: Noah Quinlan, Alexander Mortensen, Kelly Tomasevich, Temitope Adeyemi, Stephen Aoki
Introduction: Reconstruction of the medial patellofemoral ligament (MPFL) has become the mainstay of treatment for pediatric patients with recurrent patellar instability. This study compares outcomes following MPFL reconstruction with and without mersilene tape augmentation in the pediatric population.
Methods: A case-controlled retrospective review was performed. All patients under the age of 18 with recurrent patellar instability treated operatively at a single institution by a single surgeon from January 2013 through March 2017 were identified by current procedural terminology (CPT) codes. Inclusion criteria were: 1) Primary MPFL reconstruction, 2) Minimum of 3 years follow-up, 3) No previous patellar instability surgery. Patients were contacted via telephone to complete a questionnaire, which included the International Knee Documentation Committee (IKDC) form and questions pertaining to knee pain and function, satisfaction with surgery, and need for additional surgery on the ipsilateral knee.
Results: Forty-seven of 87 eligible patients completed questionnaires. Six patients had bilateral surgeries, leading to a total of 53 MPFL reconstructions, 28 with and 25 without mersilene augmentation. Both groups were similar in demographic makeup. At an average of 5.09 ± 1.15 years follow-up, mean IKDC scores were 79.4 and 75.6 in the mersilene augmentation and no mersilene augmentation groups, respectively. Significantly fewer patients experienced further injury to their ipsilateral knee in the augmentation group compared to the non-augmentation group (7.1 vs 32.0%, p=0.034). Although not statistically significant, 3.6% (1/28) of patients in the augmentation group experienced recurrent subjective instability and/or dislocation following initial surgery, compared to 20% (5/25) in the non- augmentation group (p=0.089). Overall patient-reported outcomes were similar between the two groups.
Conclusions: There were no significant differences in patient-reported outcomes after MPFL reconstruction with or without mersilene tape augmentation. Mersilene tape augmentation was associated with a lower rate of subsequent ipsilateral knee injury and, though not statistically significant, there was a lower risk of recurrent patellar instability following MPFL reconstruction.
The Effectiveness of Injection with Orthosis for the Treatment of Trigger Finger
-
Presenting author: Daniel Lara
-
Additional authors: Cynthia Ivy, Jin Wang, Kevin Renfree
Introduction: Trigger digit is one of the most common diagnoses treated by hand surgeons and therapists. The evidence based clinical practice guidelines for the therapy management of trigger digit remain variable. Meanwhile surgical algorithms typically include only injection and surgical techniques with orthotic intervention rarely included. Because of the prevalence and variable treatments of trigger digit, the authors sought to answer two questions: “What is the success rate of treating trigger digit with corticosteroid injection plus orthosis use?”, and “What are the factors that are associated with a successful outcome when combining corticosteroid injection and orthosis use for trigger digit?”
Methods: The charts of 161 patients over the age of 18 with 313 trigger digits were reviewed for descriptive information. The patients were telephoned and asked questions from a predetermined script including the QuickDASH to determine current trigger digit status and functional outcomes. Success was measured by lack of recurrence and stage of stenosing tenosynovitis (SST). Effectiveness of the treatment was determined by current SST score through analysis of digits of patients.
Results: Higher success rate is associated with non-insulin dependent diabetes, past treatment on other digits, and lower stage of trigger digit before treatment. Lower success rate is associated with insulin dependence, male sex, and use of oral anti-inflammatory medicines. Effectiveness of injection with finger based orthosis, hand based orthosis and overall use of injection and orthosis were all determined successful with statistical significance at α=.05.
Conclusions: Corticosteroid injection followed by immediate fitting of a custom orthosis or commercial proximal interphalangeal joint stabilizing orthosis worn for 6 weeks is an effective treatment for trigger digit. Associated factors with success of resolving trigger digit include non-insulin dependent diabetes, female sex, having past treatment on other digits, and a lower STT score on the first visit. . Use of oral anti-inflammatories predicts a lower success. These findings will inform therapists and surgeons in determining initial treatment interventions for trigger digit at varying stages of disease.
MPFL Reconstruction in the Pediatric Population: Does Skeletal Maturity Affect Outcomes?
-
Presenting author: Noah Quinlan
-
Additional authors: Taylor Hobson, Alexander Mortensen, Kelly Tomasevich, Temitope Adeyemi, Stephen Aoki
Introduction: Patellar instability requiring medial patellofemoral ligament (MPFL) reconstruction in the pediatric population poses a challenge in that the isometric point of femoral fixation is in close proximity to the distal physis. This study evaluates short to midterm outcomes following MPFL reconstruction in skeletally immature versus mature pediatric patients.
Methods: Patients aged <18 who underwent primary MPFL reconstruction for recurrent patellar instability by a single surgeon from 2013 to 2019 who were >1 year from surgery were contacted to complete questionnaires. Questions pertained to subsequent injury or surgery, pain, and function, including IKDC score. Further data included chart and imaging review. Patients were placed into skeletally mature or immature cohorts based on radiographic appearance of the distal femoral physis. Statistical analysis included chi-square, fisher’s exact, and Mann-Whitney U tests. Significance was determined by p-value <0.05.
Results: There were 103 primary MPFL reconstructions in 94 patients: 70 skeletally mature and 24 immature. The skeletally immature group was younger (13.1 v 15.5 years) and had a higher incidence of trochlear dysplasia (88 v 63%, p=0.04). No other baseline differences were identified. Skeletally immature patients sustained more subsequent dislocations (15 v 3%, p=0.03) and ipsilateral knee injuries (35 v 16%, p=0.04). No significant difference was observed in IKDC score, perceived percent of normal for that knee, frequency of instability events, sport participation, or VAS pain scores at rest, with ADLs, or with sport. Fewer patients in the skeletally immature group were satisfied (79 v 97%, p<0.05) and would undergo the surgery again (68 v 100%, p<0.05).
Conclusions: Among pediatric patients undergoing MPFL reconstruction, skeletally immature patients are more likely to have a subsequent ipsilateral dislocation or injury and are less likely to be satisfied with their results compared with skeletally mature patients.
Systematic review and meta-analysis of anterior cervical discectomy and fusion with plate and screw construct versus anchored cage
-
Presenting author: John Coury
-
Additional authors: Robert Bullock, Eric Huish
Introduction: Anterior cervical discectomy and fusion (ACDF) is commonly performed for degenerative conditions of the cervical spine including myelopathy, radiculopathy, cervical disc prolapse as well as for traumatic injuries. ACDF may be performed with an interbody spacer consisting of an implant or bone alone but commonly an anterior plate and screws are added to improve construct stability. More recently an anchored interbody cage with integrated screws has been used to negate the need for an anterior plate resulting in less insult to prevertebral soft tissues and plate related complications.
Methods: The PubMed database was searched for human cadaveric studies reporting segmental range of motion following single- or two-level ACDF with anchored cage or anterior locking plate were included in the study. After full text review, data was collected from included studies for mean range of motion in flexion/extension, lateral bending, and rotation along with standard deviations and sample sizes. Fixation type, number of screws used, level and number of levels instrumented, and age of cadaveric specimens were also recorded.
Results: Eight studies met inclusion criteria, four of which performed direct comparison of the two fixation methods. Meta-analysis of the four comparative studies showed no significant differences between groups. Multivariate meta-regression of all eight included studies evaluating flexion/extension demonstrated that each additional screw significantly decreased flexion/extension range of motion by 1.351 degrees. Multivariate analysis of lateral bending demonstrated no significant difference between cohorts. Finally, multivariate analysis of rotation demonstrated a significant increase in rotation of 3.071 degrees at each level for 2-level constructs as compared to single level constructs and increased rotation of 0.177 degree for each additional year of age of the cadaveric specimen.
Conclusions: The present study demonstrates no significant difference in time zero range of motion between ACDF with an anchored cage or an anterior locking plate construct. Flexion/extension range of motion was significantly decreased by increasing the number of screws in the construct. As a surgeon modifiable factor this may be important to achieving a more stable construct for fusion.
Optimizing The Use of Liposomal Bupivacaine in Shoulder Arthroplasty
-
Presenting author: Christian Martinez
-
Additional authors: Vani Sabesan, Kiran Chatha, Ravi Teja Rudraraju, Shawn Hall, Andres Guerrero, Shimron Brown, Gregory Gilot
Introduction: Shoulder arthroplasty (SA) is the fastest growing joint replacement surgery in the United States, and it has been estimated that postoperative pain management is not adequately controlled in up to 80% of patients. Liposomal bupivacaine has been an addition to this multimodal pain management that has shown promise in reducing pain, narcotic consumption, and hospital length of stay in SA but there has been some controversy regarding its efficacy in the literature. This may be due to lack of standardization across studies in the utilization of LB. The purpose of this study was to compare different titrated formulations of LB to assess the optimal dilution for pain control and decreased opioid consumption.
Methods: A prospective RCT was conducted with patients undergoing primary shoulder arthroplasty randomized into 40mL, 60mL or 80mL dilution of 20mg of LB with saline. Patient reported pain scores, dependence rates (3months continuous opioid usage) and opioid consumption were recorded at 24, 48, and 72 hours, and 7 days. Opioids consumed were converted to total morphine equivalents (TMEs) and ANOVA was performed to compare between groups.
Results: A total of 90 patients were assigned to the three dilution groups, 5 were lost to follow-up. Our results showed significant differences in pain scores between the groups at 24 and 72 hours. The 80mL dilution group reported significantly lower pain scores at both time points (2.7 and 2.2 respectively) when compared to the 60mL and 40mL groups (p<0.016). There were significant differences in average morphine equivalents consumed over the first 24 hours of the postoperative course with the 80mL dilution consuming significantly less TMEs, averaging at 1.7 pills (p<0.05) compared to average 3.48 pills for 40ml and 60ml groups. The average morphine equivalent consumed over the postoperative period was 9.6 for the 40mL group, 7.98 for the 60mL group and 2.3 for 80mL group during the 7-day period following surgery (p>0.05).
Conclusion: Our results demonstrated that the 80mL dilution group achieved significantly better pain control and consumed less opioids postoperatively after SA. If orthopedic surgeons consider using liposomal bupivacaine to optimize postoperative pain control after shoulder surgery, then optimal dilution recommended would be 80 ml based on our results.
Location of the Digital Neurovascular Bundles in Relation to a Mid-axial Incision Line: A Cadaveric Study
-
Presenting author: Brenden Cutter
-
Additional authors: Daniel Lara, Eric Huish, Marc A Trzeciak
Introduction: The digital mid-axial incision is commonly used in hand surgery. A major risk of this approach is transection of the palmar digital neurovascular (NV) structures; however, Green’s Operative Hand Surgery states that when the incision is correctly placed, the proper digital nerves should lie protected in the volar skin flap. The purpose of this study was to evaluate the location of the proper palmar digital neurovascular (NV) bundle of the fingers and thumb in relation to a mid-axial incision.
Methods: A standardized mid-axial incision along both radial and ulnar sides of each digit was made on five fresh frozen cadaver hands. The NV bundle was then exposed. The distance from the margin of the incision to the NV bundle was measured at the proximal interphalangeal joint (PIP) and the distal interphalangeal joint (DIP) creases on both sides of each digit. The same protocol was performed at the interphalangeal joint (IP) of each thumb.
Results: A total of 80 measurements were taken. There was no difference between values at the PIP and DIP levels. On the radial side of the fingers, distances were larger than those taken on the ulnar side. However, on the thumb the ulnar sided distance was larger than the radial sided measurements.
Conclusion: The digital nerves of the fingers and thumb are safe during a mid-axial approach with an increased safe zone on the radial side of the fingers and ulnar side of the thumb. Our study confirmed that the neurovascular bundle, specifically the proper palmar digital nerve, is safe during a mid-axial incision of the fingers and thumb. All of our measured values were greater than the cited 2mm with the median distance in the fingers found to be 3.96mm, and there was only one recorded value less than 3mm (2.97mm). Knowing these anatomic relationships will aid surgeons in safely approaching the digits while minimizing the risk of injury to the NV bundle.
Location of the Flexor Carpi Radialis Myotendinous Junction: A Cadaveric Study
-
Presenting author: Kunal L Panwar
-
Additional authors: Daniel Lara, Marc A Trzeciak, Eric Huish
Introduction: The flexor carpi radialis (FCR) tendon is frequently selected for use as an interposition graft, for tendon transfers, and as a landmark for volar forearm approaches. Original surgical techniques of FCR harvest recommend incision placement 10cm proximal to wrist crease. To date no anatomic study has been conducted to precisely define the location of the FCR myotendinous junction.
Methods: 5 fresh frozen cadavers were dissected, exposing the full length of the FCR. The radial styloid (RS) was selected as a distal anatomic landmark, the medial epicondyle (ME) was chosen as a proximal landmark. As the FCR myotendinous junction is chevron shaped, we marked both the proximal myotendinous junction (PMT) and distal myotendinous junction (DMT), with the DMT indicating the beginning of purely tendinous FCR. Four measurements were taken for each arm.
Results: Pearson correlation coefficient comparing tendinous length of the FCR to the overall forearm length was 0.896 indicating a strong positive correlation (p=0.040). The mean ratio of tendinous FCR length to forearm length was 0.42 ± 0.05, ranging from 0.38 to 0.50. This correlated to a distance 11.7 ± 2.3cm proximal from the radial styloid.
Conclusion: Since the original description of ligament reconstruction and tendon interposition (LRTI) for CMC arthritis by Eaton and Littler in 1973, various techniques have been described for FCR harvest. Some of these techniques require at least four separate incisions, with the proximal most extent of the FCR tendon estimated to be 10cm from the proximal wrist crease. This, however, fails to consider patients of different sizes and forearm lengths. Our results demonstrate that the tendinous portion of the FCR is located 11.7 ± 2.3cm proximal from the radial styloid. This correlates to 42% of the distance from radial styloid to medial epicondyle. As such, conventional descriptions of incision placement 10cm from proximal wrist crease would be sufficient for most indications, but for patients with very short or very long forearms, adjustments should be made.
Identifying the Location of the Flexor Digitorum Superficialis Tendon Insertion
-
Presenting author: Rex Saito
-
Additional authors: Daniel Lara, Eric Huish, Marc A Trzeciak
Introduction: The insertion point of the Flexor Digitorum Superficialis tendon and its involvement in single finger amputation injuries are important factors when guiding treatment. Flexor zone 2 injuries with involvement of the FDS tendon is considered a relative contraindication when considering replantation. We evaluated the average distance from the proximal interphalangeal crease to the distal insertion point of the FDS tendon.
Methods: Three upper extremities with a total of 12 digits were dissected for measurement. 0.7 Kirschner wires were used to mark the proximal interphalangeal crease on each digit. Dissection down to the FDP tendon insertion point was performed and measurements from the Kirschner wire to the distal aspect of the FDP tendon was then recorded using a digital caliper.
Results: The Shapiro-Wilk test showed that the data was normally distributed (p=0.202). ANOVA showed no difference in length to insertion based on the digit measured (p=0.174). The mean distance from the proximal interphalangeal crease to the distal aspect of the FDS insertion was 9.05 mm (±2.34 mm). The minimum and maximum measurements were 5.60 mm and 13.39 mm.
Conclusions: Hand traumas are time sensitive injuries and require specialized care. It is important for all providers, especially emergency room physicians, to quickly identify hand injuries that need higher level of care. A further understanding of appropriate management for traumatic hand injuries can be beneficial for the patient’s wellbeing and will decrease the financial burden on the health care system. The measurement found in this study can be used as a quick and reliable tool when assessing distal single fingertip amputation injuries. This finding may help guide physicians in treatment options in regards to replantation versus revision amputation.
Onlay Patellofemoral Arthroplasty in Patients with Isolated Patellofemoral Arthritis - A Systematic Review
-
Presenting author: Jordan Carolina Villa
-
Additional authors: Howard Nelson-Williams, Albit Paoli, Rhamee Badr, Katharine Harper
Introduction: Patellofemoral arthroplasty (PFA) remains a controversial surgical treatment for isolated patellofemoral osteoarthritis (OA) due to variable post-operative outcomes and high failure rates. Prosthesis design is one of the major factors perceived to influence this variability. There are two major types of PFA, inlay type and onlay type. Second-generation (2G) onlay prostheses have recently been associated with improved post-operative PFA outcomes but there is a paucity of current outcomes reported in the literature. This systematic review was performed to assess the current overall survivorship and functional outcomes of 2G onlay PFA.
Methods: A literature search was performed using PubMed, Cochrane Library, EMBASE and Google Scholar to identify eligible studies. Keywords used during the literature search included: “(patellofemoral OR patell* OR femoropatell* OR femoro-patell*) AND (arthroplasty OR replacement OR resurfacing)”. Inclusion criteria included studies using 2G onlay prostheses in PFAs performed for patients with isolated patellofemoral OA. Exclusion criteria included short follow up < 2 years. Twenty-three (23) studies that reported patient reported outcome measures (PROMs) and postoperative survival were included. These studies were then analyzed for type of prosthesis, gender, age, average follow-up, survival, Oxford Knee Score (OKS), and non-operative and operative complications. Pooled statistical analysis was performed for survivorship and functional scores using Excel 2016 and Stata 13.
Results: The mean follow-up of all the studies analyzed was 8.04 years. The mean age of the patients was 59.84, with females making up 76% of the patients. Operative complications rates were reported ranging from 6% to 37% with the most common complications being AO progression, persistent pain and aseptic loosening. The overall revision rate was low, with 27 revisions and 186 conversions to total knee arthroplasty (TKA) reported in 2199 PFAs. The resulting 5-, 10-, 15- and 20-year PFA survivorship was reported to be 91.71, 84.10, 77.12 and 70.73 % respectively. Functional outcomes were reported in 10 of the 23 studies (43.5%) with an average postoperative weighted mean OKS was 32.8 (range 22.3-40)
Discussion / Conclusion: There continues to be debates about which PFA implant design yields improved outcomes. Current literature reports better results with onlay implants, due to the ability to dictate rotation without taking into account the natural trochlear position. First generation onlay implants were found to result in problems with patellar tracking, instability and impingement. Therefore, implant modifications including a broader trochlear surface and an angle that better promotes patellar tracking are now what define a 2nd generation onlay prosthesis.
Our systematic review has demonstrated that safe and acceptable results of functional outcomes and PFA survivorship can result from 2G onlay PFAs at both short and mid-term follow-up for patients with isolated patellofemoral OA. This makes it an acceptable alternative to total knee arthroplasty or conservative measures in appropriately selected patients. However, more extensive studies regarding functional outcomes need to be performed. In addition, future studies should be evaluated for long-term cost saving measures of performing a PFA vs. long-term conservative management in those patients who are too young to receive a TKA. Finally, cost benefits should be evaluated in those who may never progress to a need for a TKA.
A Three-Dimensional Magnetic Resonance Imaging Based Morphologic Study of Post-Arthroscopy Hip Instability
-
Presenting author: Joseph Featherall
-
Additional authors: Dillon O’Neill, Alexander Mortensen, Kelly Tomasevich, Stephen Aoki
Introduction: With the growing prevalence of hip preservation surgery, iatrogenic hip instability is increasingly common. There is currently a limited understanding of the structural and imaging abnormalities of iatrogenic hip instability. The authors hypothesized an increased intracapsular volume and altered capsular morphology on magnetic resonance arthrogram (MRA) would be demonstrated in the post-arthroscopy hip instability population.
Methods: 43 patients with pre- and post-index hip arthroscopy MRAs were identified. These MRAs were compared with regards to total intracapsular volume calculated by automated 3-dimensional pixel intensity region segmentation, 2-dimensional anterior proximal intracapsular area in the femoral neck gunsight plane, and maximal anterior fluid pocket depth using Horos image processing software. Paired t- test, Wilcoxon signed rank test, and the McNemar test were used for identifying statistical significance.
Results: Mean intracapsular volume was significantly greater in post-index surgery MRAs (21.71 cm3 vs. 17.14 cm3; p<0.001). Proximal anterosuperior (12-3 o’clock) intracapsular area was also significantly greater post-index surgery (2.85 cm2 vs. 1.43 cm2; p<0.001). Capsule deficiency grade distributions (p<0.001), anterior capsule retraction distance (4.83 mm vs. 0.34 mm; p<0.001), and maximum anterior fluid depth (8.34 mm vs. 4.90 mm; p<0.001) were also significantly increased post-index surgery.
Conclusion: Iatrogenic hip instability is associated with MRA findings that include increases in: total intracapsular volume, intracapsular anterosuperior proximal cross sectional area, maximum proximal anterosuperior fluid depth, and capsule retraction distance. Further investigations are necessary to understand how closely these capsular features correlate with hip biomechanics, severity of symptoms, and surgical outcomes.
Evaluation of Rotator Cuff Repair with Concomitant Biceps Treatment: A Retrospective Review of Patient Outcomes
-
Presenting author: Zachary Herman
-
Additional authors: Meghan Bishop, Daniel Nemirov, Matthew Beucherie, Michael Ciccotti, Kevin B. Freedman, Brandon J. Erickson, Sommer Hammoud
Objectives: The purpose of this study is to retrospectively investigate the clinical outcomes of patients who underwent primary rotator cuff repair with concomitant biceps treatment and compare these patients to a matched cohort of patients who underwent isolated primary rotator cuff repair. We also sought to compare the clinical outcomes of tenodesis vs tenotomy when biceps treatment was performed.
Methods: A retrospective chart review of 173 patients who underwent RCR at a single large multicenter group in 2016 was performed. Information regarding demographics, presence of concomitant biceps pathology, pre- and postoperative ASES scores, rates of cuff failure, and all complications were compiled.
Results: There were 84 patients who underwent biceps pathology treatment [tenotomy (n=26) or tenodesis (n=58)] and 89 who underwent RCR alone. There was no significant difference in terms of average age (p = 0.201), gender (p = 0.329), or side of surgery (p = 0.100). Preoperatively, the group with biceps pathology had lower average ASES scores compared to the group without biceps pathology (40.4 vs 49.0; p = 0.009). Postoperatively, there was no significant difference in average ASES scores between the two groups (77.7 in biceps treatment group vs. 81.9 in group without biceps pathology; p = 0.476). There was no significant difference in terms of rates of cuff failure after 2 years (3.61 % in biceps treatment group vs 5.75% in group without biceps treatment; p = 0.721) or rates of all complications (4.76% in biceps treatment group vs 11.2% in group without biceps treatment; p = 0.200). Preoperative ASES (33.7 in tenotomy group vs 43.2 in tenodesis group; p = 0.0642) and postoperative ASES (73.7 in tenotomy group vs 79.7 in tenodesis group; p = 0.422), scores were not significantly different. There was no significant difference in terms of rates of cuff failure after 2 years (3.85% in tenotomy vs 3.51% in tenodesis; p = 1.000) or all complications (3.85 % in tenotomy vs 5.17% in tenodesis; p = 01.000).
Conclusions: Our results support the conclusion that correcting biceps pathology when performing RCR is safe, resulting in similar rates of cuff failure and all complications when compared to isolated RCR alone. Furthermore, when comparing tenotomy vs tenodesis, our results support the conclusion that neither method is superior in terms of altering cuff failure, complication rates, or ASES scores when performed with an RCR.
Real World Survey Burden of Common Patient-Reported Outcome Measures Utilized in Shoulder Surgery
-
Presenting author: Andrew Potyk
-
Additional authors: Darby Houck, Ian Verbeck, Eric McCarty, Rachel Frank, Michelle Wolcott, Adam Seidl, Jonathan Bravman
Introduction: Patient-reported outcome measures (PROMS) are important for tracking outcomes following shoulder surgery. However, PROMS can be limited by time constraints and patient compliance. The purpose of this study was to evaluate the time to complete commonly administered PROMS as well as determine how it affects survey completion rates following shoulder surgery.
Methods: Utilizing our institutions prospective outcomes registry, we identified patients who underwent shoulder surgery, including rotator cuff repair (RCR), and (anatomic and reverse) total shoulder arthroplasty (TSA). Patients were invited to complete a survey consisting of 6 PROMS pre- and postoperatively at 3, 6, 12, and 24 months. A series of univariate multiple logistic regression analyses were performed to determine all possible predictors of completion rate at each time interval.
Results: An overall total of 742 patients (male, 58.9%; mean age, 60.9±10.8 years) who underwent shoulder surgery were enrolled (RCR, n=467; TSA, 275). The overall average completion time was 9.9±14.6 minutes. Six variables significantly increased the likelihood of completion at each follow-up interval: (1) Doubling the time per question of the most recent survey taken (6-month, OR: 2.0); (2) The most recent survey being taken through email (3-month, OR: 2.4; 12-month, OR: 9.5); (3) Each additional access attempt (averaged over all previous surveys) (6-month, OR: 1.9; 24-month, OR: 2.1); (4) Obtaining the minimally clinically important difference (MCID) in the most recent survey taken (6-month, OR: 3.7); (5) Undergoing RCR (vs. TSA) (pre-op, OR: 2.3; 24-month, OR: 3.1); and (6) Being over the age of 66 (vs. 58 to 66) years (24-month, OR: 2.4). Two variables significantly decreased the likelihood of completion at each follow-up interval: (1) Each additional (reminder) email sent decreases (pre-op, OR: 0.85; 3-month, OR: 0.40; 6-month, OR: 0.58); 12-month, OR: 0.86); and (2) Receiving care at the hospital clinic (vs. the satellite clinic) (pre-op, OR: 0.464).
Conclusions: The results of this study are noteworthy as they may suggest that patients who intend to complete the survey- potentially as a result of doing well after surgery- are going to complete it. Although socio-demographic and treatment factors also significantly influenced completion rate, the reality may be that these surveys are only burdensome to individuals who perceive surveys as a burden.
Pigmented Villonodular Synovitis of the Hip in Patients Undergoing Total Hip Arthroplasty: A Retrospective Case-Controlled Analysis
-
Presenting author: Andrew D Ardeljan
-
Additional authors: Teja Polisetty, Joseph Palmer, Justin Toma, Gagan Grewal, Martin W Roche
Introduction: Pigmented villonodular synovitis (PVNS) affects larger joints such as the hip and knee. Little is known regarding implications of PVNS in total hip arthroplasty (THA). The aim of the study was to determine if patients with PVNS of the hip undergoing primary THA experience greater: 1) in-hospital lengths of stay (LOS); 2) complications; 3) readmission rates; and 4) costs.
Methods: Patients undergoing primary THA for PVNS of the hip were identified using a nationwide registry. PVNS patients were matched to controls in a 1:5 ratio by demographics and comorbidities. This yielded 7,440 patients with (n=1,240) and without (n=6,200) PVNS of the hip undergoing primary THA. Endpoints included LOS, complications, readmission, and costs. Multivariate logistic regression was used to determine odds ratios (OR) of developing complications. Welch’s t-tests were used to test for significance in LOS and cost. A p-value less than 0.001 was considered statistically significant.
Results: PVNS patients had longer LOS (3.8 days vs 3.5 days, p=0.0006). PVNS patients had greater odds of (OR: 1.60, p<0.0001) medical and (OR: 1.81, p<0.0001) implant-related complications. Furthermore, PVNS patients were found to have higher odds (OR: 1.84, p<0.0001) of 90-day readmissions. PVNS patients also incurred higher day of surgery ($13,119 vs. $11,983, p<0.0001), and 90-day costs ($17,169 vs. $15,097, p<0.0001).
Conclusion: The findings of the study suggest PVNS of the hip is associated with worse outcomes and higher costs following primary THA. The study is useful as orthopaedic surgeons can use the study to educate patients of the complications which may occur following their hip surgery.
Intraoperative Testing of Hip Capsular Repair Demonstrates Restoration of Axial Distraction Resistance
-
Presenting author: Dillon O’Neill
-
Additional authors: Alexander Mortensen, Joseph Featherall, Suzanna Ohlsen, Kelly Tomasevich, Stephen K. Aoki
Introduction: It has previously been shown in cadaveric models that failure resistance of capsular repair is dependent on the robustness of the repair construct. However, in vivo data on the efficacy of capsular repair techniques are limited. The authors hypothesized that a figure-of-eight capsular repair would restore hip resistance to axial distraction to pre-capsulotomy levels.
Methods: 32 consecutive patients undergoing primary hip arthroscopy for femoroacetabular impingement syndrome with a single surgeon were prospectively enrolled. Prior to surgery, traction was applied to the operative lower extremity using an integrated spring traction system at predetermined traction intervals for the intact state, followed by fluoroscopic imaging of hip distraction distance. A standard interportal capsulotomy was then created and surgery progressed as usual. Traction force-distraction distance testing was then repeated prior to capsular repair and then again after repair. Distraction force and joint distraction displacement were then analyzed for these 3 capsule states.
Results: The mean difference in distraction distance for all traction forces between 37.5-100lbs was 3.32mm between the intact and capsulotomy states and 3.32mm between the capsular repair and capsulotomy states. The capsular repair state was associated with a small but statistically significant increase in distraction distances at 37.5 lbs-f (5.55mm vs. 4.99mm; p =0.006), 50lbs-f (6.14mm vs. 5.37mm; p < 0.001) and 62.5lbs-f (6.66mm vs. 6.34mm; p =0.045) relative to the intact state.
Conclusion: This study provides in vivo biomechanical evidence demonstrating that capsulotomy results in significantly lower resistance to axial distraction across the hip joint relative to the native state. Furthermore, the data suggest that capsular closure using a reproducible figure-of-eight suture repair reconstitutes the majority of capsular resistance to axial distraction intra-operatively. Future research should evaluate the in vivo effects of other published capsular repair techniques and assess the biomechanical durability of in vivo capsular repairs over time.
The Effect of Age and Activity Level on SLAP Repair Outcomes
-
Presenting author: Andy Kuo
-
Additional authors: Shane Davis, Christopher S. Lee
Introduction: The purpose of this retrospective study is to compare the outcomes of SLAP repairs between three patient populations above and below the age of 40: heavy laborers, overhead athletes, and people who participate in neither activity.
Methods: 141 patients with SLAP lesions underwent arthroscopic SLAP repairs by a single sports medicine fellowship trained orthopedic surgeon. Patients were classified into three populations: overhead athletes (n=58, 41.1%), heavy laborers (n=29, 20.6%), or neither (n=54, 38.3%). UCLA, ASES, and a self-reported recovery satisfaction score ranging from 0 to 100 were obtained post-operatively (average 36.4 months) for all patients and comparisons were made between the populations.
Results: Without considering age, the overhead athlete population had higher scores in all three outcomes when compared to the “neither” population. The average UCLA, ASES, and recovery satisfaction scores were 30.2 vs. 27.6 (p=0.02), 90.9 vs. 84.0 (p=0.009), and 92.0 vs. 85.2 (p=0.03), respectively. Comparing the populations under 40 years, the heavy laborer population scored significantly higher on ASES than the overhead athlete (96.7 vs. 89.0; p=0.004) and neither populations (96.7 vs. 86.8; p=0.04). Comparing the populations over 40 years, the overhead athlete population scored significantly higher on both ACES (92.3 vs. 83.1; p=0.006) and UCLA (30.6 vs. 27.5; p=0.03) than the neither population. No significant differences were noted in any of the other comparisons.
Conclusions: Without considering age, overhead athletes demonstrated higher satisfaction and function following SLAP repairs than persons who do not participate in overhead athletics or heavy labor. Even though there were significant differences noted when considering age, these differences were only seen in one or two outcome scores, but never all three. This contrasts the significant difference found when we did not consider age, where all three outcome scores were found to be statistically significant between the relevant populations. This weaker correlation when considering age suggests that the myriad of factors associated with age plays a significant role when comparing these three populations. This finding suggests further study is necessary to identify the responsible factors prior to recommending SLAP repairs for overhead athletes, heavy laborers, and persons who participate in neither activity.
Factors Affecting Pelvis Position During THA in the Lateral Decubitus Position
-
Presenting author: Daniel Sherwood
-
Additional authors: Eli Kamara, Zeynep Ferlengez, Yonatan Schwartz
Purpose: Acetabulum component positioning is critical to successful total hip arthroplasty (THA). Anatomic landmarks, alignment guides, and intraoperative X-rays are tools used in performing this crucial step. Previous studies demonstrate wide variability of pelvis positioning in the lateral decubitus position (LDP), questioning the reliability of external alignment guides. The aim of this study is to determine factors that impart increased risk of pelvis malpositioning and whether this affects acetabulum component placement.
Methods: We retrospectively reviewed X-rays of 204 patients who underwent posterior THA in the LDP by three surgeons from 2017-2018. Pelvic tilt and rotation as described by Otero et. al. were measured on intra-operative and post-operative X-rays. Demographic and clinical data including height, weight, BMI, lumbar spine arthritis, history of spinal surgery/fusion, lower back pain, and positioner type were recorded. Patients with intra-operative radiographs without a visible sacrococcygeal joint were excluded. 30-50° of abduction was defined as proper cup positioning (PCP). Proper pelvic positioning (PPP) was defined as vertical tilt and axial rotation of +/- 15°.
Results: The average pelvic tilt and rotation were 4.76° and 6.39° backwards, respectively. PPP was obtained in 138/204 cases (68%). PPP occurred in 77/103 patients (75%) with the Capello or Wixon hip positioner, compared to 61/101 (60%) with the De Mayo positioner (p<0.02). Patient height, weight, BMI, and L-spine pathology was not associated with PPP. PPP had no affect on proper cup position; of the patients with PPP, cup position was proper in 123/138 (89%), compared to 15/138 (11%). Pelvic position was within +/- 20° of tilt and rotation in 86% of cases.
Conclusion: Pelvis orientation in the LDP is highly variable. Certain hip positioners are associated with increased rates of pelvis malpositioning. Surgeons should be aware of these differences when using alignment guides and intraoperative X-rays during THA.
Freestyle skiing is associated with similar proximal femur and lumbar spine adaptations and lower body mass index as compared to skiers in non-freestyle events
-
Presenting author: Ilona Schwarz
-
Additional authors: Darby Houck, Jonathan Bravman, Viral Shah, Austin Jolly, Rachel Frank, Eric McCarty
Introduction: Freestyle skiers must optimize aerial performance while maintaining the strength and coordination to propel themselves in the air and adapt to uneven surfaces. The purpose of this study is to investigate the differences in areal bone mineral density (aBMD) and body composition in freestyle skiers and non-freestyle skiing controls.
Hypothesis: We hypothesized that the transfer and distribution of high-impact, short duration, directionally variable forces experienced by the freestyle athletes would result in increased aBMD and decreased body fat.
Level of Evidence: Level 3, Retrospective Cohort Study
Methods: 18 freestyle skiers (14M 4F, [27.56 ± 5.22 years]) and 15 controls (7M 8F, [26.93 ± 3.54 years]) were measured with dual energy X-ray absorptiometry (DXA) to determine total body composition, hip and lumbar spine aBMD and bone mineral composition (BMC). Height and weight were measured with an in-office stadiometer and scale. Questionnaires were used to gather physical activity and medical history. Between-group variations were analyzed with an analysis of variance (ANOVA) and stratified by sex.
Results: Percent fat, hip and lumbar spine aBMD, BMC, and area were all similar between freeski and nonfreeski athletes (p<0.05 for all). BMI was significantly lower in male freeski athletes (23.97kg/m2, 95% CI [22.75-25.18]) when compared to other skiers (26.64kg/m2, 95% CI [24.43- 28.86]) (p=0.03). Male freestyle skiers also had less body fat (controls 26.64%, 95% CI [24.43- 28.86], freeski 23.97%, 95% CI [22.75-25.18]) (p=0.09).
Conclusions: Freestyle skiers maintain a high aBMD despite a low BMI. This study shows that BMD can be maintained independent of body mass with movement patterns emphasizing torsion and loading.
Clinical Relevance: Skiers endure a variety of intense physical forces yet remain understudied despite high orthopedic injury rates. This study serves as a pilot to broaden the current sports health literature and better understand the relationship between winter sports and musculoskeletal health.
Quantifying Survival and Mortality Among Geriatric Orthopaedic Trauma Patients: A Retrospective Chart Review
-
Presenting author: Frederick Mun
-
Additional authors: Kathy Ringenbach, Blake Baer, Sandeep Pradhan, Kayla Jardine, Vernon Chinchilli, Michael Andreae, Henry Boateng
Introduction: An increasingly active and growing elderly population has led to more geriatric orthopaedic trauma patients. There is limited literature quantifying survival and mortality in this patient population. The purpose of this study was to evaluate the independent risk factors related to survival and mortality in geriatric orthopaedic trauma patients admitted to the ICU as a Level 1 or 2 trauma activation.
Methods: A retrospective chart analysis was done on 174 patients over the age of 60, from January 1, 2008 to January 1, 2018, who were involved in a multi-trauma with orthopaedic injuries. Variables evaluated include: sex, age, Injury Severity Score (ISS), Trauma and Injury Severity Score (TRISS), Abbreviated Injury Scale (AIS), length of stay in the ICU, use of vasopressors, use of ventilator, head injury, Multiple organ dysfunction syndrome (MODS), number and type of orthopaedic injury, number of orthopaedic surgeries, <30 day mortality, and >30 day mortality. A Kaplan-Meier estimator and Cox proportional hazards model were used to identify risk factors for mortality and predictors of survival.
Results: The average mortality was 47.7% (n=83). The relative risk for mortality within 30 days increased with age (RR: 1.09, 95% CI: 1.03-1.16), ISS (RR: 7.24, 95% CI: 2.16-24.2), high-energy trauma (RR: 3.42, 95% CI: 1.13-10.3), length of ICU stay (RR: 0.71, 95% CI: 0.56 -0.91), MODS (RR: 22.4, 95% CI: 5.23-96.2), psychiatric disorder (RR: 3.22, 95% CI: 1.03-10.0), and anticoagulant use (RR: 20.5, 95% CI: 5.22-80.7). Patients with an ISS ≤30 were significantly more likely to survive than patients with an ISS >30. Greater age (HR=1.04, 95% CI: 1.01-1.07), ISS (HR=2.31, 95% CI: 1.31-4.07 ), length of ICU stay (HR= 0.76, 95% CI: 0.65-0.89), MODS (HR=5.13, 95% CI: 2.74-9.59), anticoagulant use (HR=2.74, 95% CI: 1.55-4.87), and ventilator use (HR=1.29, 95% CI: 1.11-1.50) were significantly associated with lower survival rates. There were no statistically significant associations between survival and number of orthopaedic surgeries and orthopaedic injuries.
Conclusions: A high ISS (>30) at admission is strongly predictive of a lower probability of survival. Furthermore, lower age, ISS, length ICU stay, MODS, anticoagulant use, and ventilator use, are significantly predictive of survival. These indications help us to better understand the factors predictive of death among geriatric orthopaedic trauma patients, and to improve the way we can diagnose and care for them.
Manipulation Under Anesthesia following Two-Team Simultaneous Primary Total Knee Arthroplasty
-
Presenting author: Nicholas L Kolodychuk
-
Additional authors: Samuel Hammonds, Daniel Enright, Gregory Vrabec
Introduction: Bilateral total knee arthroplasty can be performed under a single anesthesia event (simultaneous) by one surgeon or two surgeon teams or under different anesthesia events (staged).
Post-TKA knee stiffness is common and can be treated with manipulation under anesthesia (MUA) with incidence reported between 0.5%-10%.1 Various risk factors for MUA have been identified including younger age, female sex, high BMI, smoking, and others.2-4 Rates of MUA for one-team simultaneous and staged have been investigated. There is a lack of literature regarding MUA following two-team simultaneous bilateral TKA. Our aim was to investigate incidence of MUA and associated risk factors following two-team simultaneous bilateral TKA.
Methods: Following IRB approval a retrospective review of a single healthcare system from 2010 to 2014 was performed. Patients who underwent primary TKA were included. Demographic, operative, and manipulation under anesthesia data was collected. Chi-square and student t tests were used for categorical and continuous variables with p<0.05 indicating significance. Multivariate logistic regression was used to examine risk factors for manipulation under anesthesia.
Results: Review identified 1697 patients who underwent primary TKAs. Two-team simultaneous bilateral TKAs were performed in 233 patients (466 knees). The remainder of patients underwent unilateral TKA. Rate of MUA was similar between unilateral (7.1%) and two-team bilateral TKA (6.0%). Multivariate analysis found age <65 (Odds ratio [OR] 1.93) and BMI <30 (OR 1.64) were associated with MUA. Two-team bilateral TKA, diabetes, and sex were not associated with MUA in our population.
Conclusions: Rates of MUA have previously been shown to be higher in staged bilateral TKA than in unilateral TKA or one-team simultaneous bilateral TKA. Our study demonstrates similar rates of MUA in two-team simultaneous bilateral TKA as unilateral TKA. The risk factors for MUA are similar between two-team bilateral TKA and unilateral TKA in our population. Two-team simultaneous bilateral TKA can be performed without increased risk of MUA.
Optimal Treatment For Glenoid Bone Loss: Augmented Versus Standard Reverse Shoulder Arthroplasty?
-
Presenting author: Siddharth Kundal
-
Additional authors: Vani Sabesan, Diego Lima, Christian Martinez
Introduction: Since the early 1970s, standard reverse shoulder arthroplasty (RSA) has seen an increasing range of clinical application in the treatment of shoulder pathologies. Introduced in 2011, augmented glenoid implants have shown encouraging results as a treatment for managing glenoid bone loss. With greater innovative options for RSA, surgeons must decide the best procedure for optimal clinical outcome. With a lack of follow up studies comparing the use of augmented RSA (aRSA) to standard RSA (sRSA), the decision is not always clear. This study will compare the postoperative outcomes between augmented and standard RSA.
Methods: Using a database of 26 patients treated with RSA, we grouped 15 patients into the sRSA group and 12 patients into the aRSA group. Demographic variables, glenoid version and postoperative outcomes were collected and functional range of motion was collected at last follow up (minimum 3mo FU). Outcomes and ROM for each group were compared and statistical analysis were performed with with t-tests.
Results: There was a total of 12 males and 11 females with an average of 71 years old included in the study. All patients had a B2 or B3 type glenoid and the sRSA group had an average glenoid version of –9.5°compared to an average –24.4° for aRSA group (p = 0.0033). There was no significant difference in ASA scores between the aRSA and sRSA groups. There were significant differences in gender distribution and BMI between groups (p<0.05). There was no significant difference between the average range of motion for abduction, flexion, and external rotation (p≥0.05) but a trend toward increased forward elevation for sRSA.
Conclusions: The decision between augmented glenoid baseplate versus standard RSA for severe glenoid bone loss is still unanswered for surgeons. Standard reverse shoulder arthroplasty may have better postoperative outcomes concerning range of motion however further research is needed to help guide surgeons with the optimal treatment for these increased complexity cases of glenohumeral arthritis.
Arthroscopic Repair of Femoral-Sided PCL Avulsions Using a Transosseous Drilling Technique - a Retrospective Review
-
Presenting author: Zachary Bloom
-
Additional authors: Timothy Mulry, Marc Lubitz, Brian Busconi
Background: Femoral-sided ligamentous avulsions of the PCL are an uncommon, but significant, insult to the ligamentous stability of the knee. Primary repair of these lesions is not well investigated in the orthopedic literature. The purpose of this study is to assess the subjective, objective and radiographic outcomes following primary transosseous PCL repair of femoral-sided “peel-off” lesions.
Methods: This retrospective case series included patients who underwent primary repair of femoral-sided “peel- off” PCL ruptures at a single institution from 2017 to 2019. Patients underwent a preoperative and post- operative MRI to diagnose injury and ligamentous healing as a part of routine standard of care. Demographic information, radiographic evidence of PCL healing, range of motion, ligamentous examination of the knee, SF12, VAS and IKDC scores were analyzed.
Results: 11 patients were reviewed. 10 patients had multi-ligamentous knee injuries and 1 had an isolated PCL rupture. At 6 months and 12 months, all patients had improved ROM. Post-operatively, all patients had Grade I posterior drawer examination, and had otherwise stable ligamentous exam. MRI of all patients confirmed ligamentous healing of the PCL repair at 6 months. There was 1 complication: arthrofibrosis requiring a manipulation under anesthesia and arthroscopic lysis of adhesions 3 months following index procedure. IKDC, VAS, SF12 all showed improvement in subjective pain scores and function post- operatively.
Conclusion: Arthroscopically assisted primary PCL repair for femoral-sided avulsion injuries using a transosseous drilling technique yields satisfactory knee function, radiographic evidence of healing and excellent subjective scores at 6-months and 1-year following repair.
Before or After? An Assessment of 1-Year Complications in Spinal Fusion and Total Hip Arthroplasty
-
Presenting author: Nequesha Mohamed
-
Additional authors: Ethan Remily, Wayne Wilkie, Scott Douglas, Sahir Pervaiz, Oliver Sax, Johannes Plate, Ronald Delanois
Introduction: The success of total hip arthroplasty (THA) is well documented, as is the success of lumbar spinal fusion, but recently, questions have been raised regarding treating patients with concurrent hip and spine pathologies. Often termed “hip spine syndrome”, denoting degenerative disease in both the lumbar spine and hip, treatment procedures are clear, but the order in which to perform them has been the subject of debate. However, direct comparisons of pre-THA fusion and post-THA fusion are lacking. This study matches pre-THA and post-THA fusion patients to assess postoperative complications for one year.
Methods: A retrospective review was performed utilizing the PearlDiver Supercomputer identifying all THA patients between 2010 and 2018, gathering 716,084 patients. Patients who underwent spinal fusions prior to THA were propensity score matched 1:1 to patients that underwent THA prior to undergoing lumber fusion, yielding 4,510 patients in each cohort. Categorical variables were tested with chi-square analyses, while Continuous variables were analyzed with t-test.
Results: Pre-THA and post-THA fusion patients were similar in age (p=0.246), male sex (p=0.999), CCI (p=0.999). and morbid obesity (p=0.999). However, pre-THA fusion patients had a shorter length of stay (p=0.015). With regard to one-year revision rates, both groups were similar (p=0.426). Pre-THA patients experienced significantly fewer hematomas at one year (p=0.008), but conversely experienced significantly more dislocations (p<0.001), pneumoniae (p=0.005) and joint infections (p=0.020). All other complication differences were nonsignificant.
Conclusions: The timing of THA and spinal fusion in patients requiring both procedures has become a hot topic. This study suggests performing spinal fusion after THA to reduce hip dislocation, as well as reducing joint infection rates. Reduced dislocations may be due to more accurate acetabular placement prior to spinal procedures. Determining the ideal interim time between THA and spinal fusion is the next step to optimizing these procedures for these patients.
Far Cortical Locking Versus Standard Locking Screw Fixation in Simulated Femoral Fractures: A Biomechanical Meta-Analysis
-
Presenting author: Robert Bullock
-
Additional authors: John Coury, Eric Huish
Introduction: Comminuted distal femur fractures remain difficult to treat due to the high incidence of non-union after locking plate fixation. A contributing factor to non-union with standard locking (SL) plate fixation includes construct rigidity, particularly on the side adjacent to the plate. Far cortical locking (FCL) is a concept of fixation with the goals of reducing stiffness and producing symmetric micromotion to improve callus formation without compromising load to failure. This is done through insertion of locking screws in which the screw threads only engage the far cortex and plate, allowing toggle between the near cortex and screw shaft. This can be performed by using partially threaded far cortical locking screws that only engage the far cortex, or by technique with over-drilling the near cortex producing a cortical slot. The goal of our study was to review the current biomechanical data evaluating the effects of partially-threaded FCL versus standard fully-threaded SL fixation.
Methods: A Pubmed database search was screened by two independent reviewers to identify any available biomechanical studies that directly compared FCL and SL plate fixation for simulated femoral fractures in cadaveric specimens or surrogate bone models. Primary outcomes included construct stiffness, load to failure, axial motion at the near cortex, axial motion at the far cortex, and the difference between near and far cortical axial motion to demonstrate motion symmetry.
Results: FCL screws decreased construct stiffness by 1.069 kN/mm as compared to SL screws. FCL demonstrated greater axial motion than SL in the near cortex by 0.425 mm and in the far cortex by 0.456 mm. FCL resulted in symmetric axial motion with no significant difference between far and near cortex compression with the far cortex displacing 0.347 mm or more than near. SL resulted in asymmetric axial motion favoring the far cortex by 0.270 mm. The load to failure was not significantly different between FCL and SL, with FCL load to failure 0.367 kN higher than SL.
Conclusions: In our review of the current biomechanical data, we found that FCL screw fixation in femoral fractures achieves the goals of reducing construct stiffness and promoting more symmetric axial motion while maintaining construct strength with no difference in load to failure. These results support the overall biomechanical goals of far cortical locking and should encourage continued investigation into its effects on clinical and radiographic outcomes.
Orthopaedic Fellowship Information for an AOA applicant
-
Presenting author: Shayne R Kelly
-
Additional authors: Daniel Lara, Joseph Smathers, Marc A Trzeciak
Background: The orthopaedic fellowship match process as we know it today was established by the American Academy of Orthopaedic Surgeons (AAOS) and the American Orthopaedic Association in 2008. Approximately 90% of graduating orthopaedic residents apply for fellowships and before 2008 the absence of a match made interviewing difficult and the process frustrating for applicants and program administrators alike. Before 2008, there was no standardized fellowship match process. While data for ACGME programs have been reported, it is lacking for an American Osteopathic Association (AOA) applicant. The purpose of our study was look at factors including financial impact, time spent interviewing, and how to determine their rank lists for AOA applicants.
Methods: An anonymous survey was created with 12 questions in multiple choice format. American Osteopathic Academy of Orthopedics (AOAO) was sent the link, and they sent it to the recent fellowship matches. Deadline was set for 2 months with periodic reminders. All responses were used in the study. Statistical analysis was done using the SPSS Version 23 (IBM, Aramonk, NY).
Results: There were 90 surveys completed. 4 chose not to do fellowships. 97.7% of applicants matched. The average total amount spent was $5327.56. The average number of applications sent was 25.26, and the average number of interviews completed was 8.4. Sports had the most applicants with 24. 44.2% matched into their 1st choice. Faculty and staff was the number 1 reason for choosing a program for 32.1% of applicants.
Conclusions: Our data confirmed that DO orthopedic applicants were applying to more fellowship programs and generating less interviews than their MD orthopedic applicant counterparts. Applicants preferred programs based on their faculty just like their MD counterparts. This study provides good initial insight for a DO orthopedic fellowship applicant. Future research is needed going forward with all programs now undergoing a single accreditation. This dichotomy may change for the DO orthopedic applicant with the advent of the single accreditation system.
Bilateral Simultaneous Anterior Cruciate Ligament Ruptures in a Female Skier with Systemic Lupus Erythematosus
-
Presenting author: Jacob Dunn
-
Additional authors: Daniel Lara, Michael Holmboe, Jonathan M Pettegrew
Introduction: Anterior cruciate ligament (ACL) rupture is one of the most common knee injuries seen by orthopedic surgeons, with 100,000 cases documented in the United States annually. The incidence of patients presenting with bilateral ACL ruptures has been reported to be between 2-4% in the literature. Here we present a unique case of a 30-year-old female skier with a past medical history of systemic lupus erythematosus (SLE), who suffered simultaneous bilateral ACL ruptures while skiing.
Methods: The patient is a 30-year-old female with a significant past medical history for SLE, who presented with bilateral knee pain, after twisting their knees while skiing. Bilateral Knee MRIs were obtained, revealing bilateral ACL tears. After discussing with the patient about the benefits and risks of simultaneous surgeries versus staged repair, the patient decided to proceed with simultaneous bilateral ACL reconstruction utilizing bilateral bone-patellar tendon-bone (BTB) autografts.
Results: The patient started physical therapy following surgery. At 2 weeks post-operative both knees were stable, had a ROM of 0-120 bilaterally, and quadriceps strength of 3/5 bilaterally. At six months following surgery the patient was able to return to their normal activities, had a ROM of 0-140, and had quadriceps strength of 4/5 bilaterally.
Conclusion: Simultaneous bilateral ACL ruptures are rare injuries with only a few cases being reported in the literature. Currently there are no defined guidelines for optimal management of these patients. Both staged and simultaneous ACL reconstructions are considered appropriate for the management of bilateral ACL injuries. Studies that have examined outcomes of bilateral ACL reconstruction, have shown that in addition to having comparable clinical outcomes as staged reconstruction, simultaneous reconstruction is both more time and cost effective, leading to less total rehabilitation time before returning to sports.
Case Study: The Effect of Medicaid Expansion on Payments to Orthopedic Surgeons from Industry
-
Presenting author: Michael V. DiCaro
-
Additional authors: Andrew Muse, Joel Mintz, Joseph Richards, Jacob Sorenson, Walid Raslan
Introduction: Previous studies suggest that Medicaid reimbursements are 20% lower than similar claims submitted to Medicare. Lower reimbursement rates may shift physicians’ perspectives on industry payments. While other fields such as neurosurgery saw an increase in industry payments after 2013, the effect of Medicaid expansion on industry payments in orthopedic surgery is incompletely understood. Here, we examine if Medicaid expansion was associated with an increase in industry payments to orthopedic surgeons by comparing states that expanded Medicaid to epidemiologically matched states that did not.
Methods: Industry payments are reported to the Open Payment Database (OPD) as General, Research or Ownership payments. The OPD was queried for general payments to orthopedic surgeons between 2013-2018 in North Dakota (N.D), South Dakota (S.D), Kentucky and Alabama. N.D. expanded Medicaid access in 2013, whereas Kentucky did so in 2014. These two states were matched to S.D and Alabama, respectively, which did expand Medicaid. States were matched based on their total population, GDP per capita, and proportion in poverty. Due to the nonparametric nature of the OPD data test (Shapiro-Wilk test P<.001), Mann-Whitney-Wilcoxon U test was used to compare differences in total pay relative to 2013 for the years 2015-2018.
Results: Industry payments to orthopedic surgeons increased in all four states regardless of Medicaid expansion. Orthopedists in N.D received higher payments in 2013-2014 before declining in 2015-2018. S.D. reported significantly higher payments from 2016-2018 (p=.042, .030, .006 respectively) than N.D. Kentucky reported higher payments from 2013-2018 than those from Alabama, although not statistically significant. Although physicians from Kentucky saw higher industry payments, the gap in payments narrowed after 2014 where recipients from Alabama experienced a greater relative increase in payments.
Conclusions: The effects of Medicare expansion on industry payments to orthopedic surgeons contrasted each other in our 4-state analysis. We plan to expand our analysis to include data from all 50 states and undertake multivariate modeling to explore our findings.
Impact of HIV Status on Surgical Outcomes after Primary Total Hip Arthroplasty
-
Presenting author: Ridhi Sachdev
-
Additional author: Anna Tarasova
Introduction: Medical optimization of HIV-positive patients (HPP) has allowed for significant improvements in overall health and life expectancy. An increasing number of HPP are undergoing elective procedures, including total hip arthroplasty (THA). Few studies have evaluated the impact of HIV status on THA. We explored the impact of HIV-status on post-operative complications after THA.
Methods: A retrospective chart review of patients who received primary THA at a high volume, academic center between 2016 and 2019. The primary outcome is return to operating room for any reason (ROR) and secondary outcome was infection at the surgical site. We compared the baseline demographics and outcome variables of cohort of HPP with non-HIV patients undergoing primary THA. Additional variables collected included patient demographics and medical comorbidities. Student’s t-test and chi square were used to compare demographic and surgical outcomes between HPP and non-HIV cohorts. Cox Proportional Hazards Model was used to compare Time to Outcome Hazard Ratios (HR) used to assess the impact of HIV status on return to OR, all cause revision and rate of infection and presented as HR, 95% Confidence Interval (CI) for each outcome.
Results: 1370 undergoing primary THA were identified, of which 70 were HPP. The mean (SD) age was 60.8 (12.0) and 738 (54%) female. At an average of 12.4 month follow-up, overall 48 (3.6%) returned to OR, 32(2.4%) required all cause revision, and 22 (1.6%) were found to have PJI. When comparing HPP and non-HIV patients, return to operating room was higher in the HPP group, but this was not statistically significant (HPP:5.7%, Non-HIV:5.7%, (HR: 1.67 CI95%:0.6-4.64),p=0.3). No significant differences were noted with regards to rate of infection (HPP:2.8%, Non-HIV:1.5%, (HR: 1.86 95% CI: 0.43-7.94),p=0.4). On multivariable logistic regression, controlling for age, gender, ASA status, and CCI score, HPP were at no increased risk of return to OR (adjusted odds ratio [aOR], 0.82; 95% CI:0.14-4.63), all cause revision (aOR, 0.73; 95% CI, 0.09-5.73), and rate of infection (aOR, 0.56; 95% CI, 0.02-18.3).
Conclusion: Our study found that HIV-positive patients undergoing THA can achieve surgical outcome on par with a non-HIV cohort, with regards to return to OR, rate of revision, and rate of surgical infection.
Prolonged LOS After Primary TKA in an Urban, High-Volume Joints Center Serving Socioeconomically Disadvantaged Minority Populations
-
Presenting author: Yoav Zvi
-
Additional author: Zeynep Seref-Ferlengez, Sun Jin Kim
Introduction: Identifying risk factors for increased Length of Stay (LOS) after primary Total Knee Arthroplasty (TKA) has the potential to improve healthcare outcomes and spending. This study aimed to identify patient characteristics associated with prolonged LOS after primary TKA in an urban, high-volume joints center serving a predominantly Hispanic and Black population. Methods: A retrospective cohort study of patients who underwent primary TKA in a single, high volume, academic center. Demographic data, ASA status, smoking status, co-morbidities, insurance type, socioeconomic status and discharge disposition were collected. Patients were categorized into two groups based on LOS (Normal LOS: 1-2 days, Prolonged LOS: >2 days).
Patient characteristics were compared between LOS groups using Wilcoxon Sum-Rank, Chi- squared and Fisher’s exact tests. Logistic regression analyses were to determine independent risk factors for prolonged LOS.
Results: A total of 3,093 patients were identified with a mean age of 64.7±9.7 years (76.8% female). The cohort included 47.9% Hispanic and 38.3% African American patients. Factors associated with prolonged LOS included increased ASA or CCI, smoking, several comorbidities (p<0.05). Non-home discharge, low socioeconomic status (SES) and insurance type (Medicare or Medicaid) were also associated with prolonged length of stay (p<0.05). Logistic regression analysis performed using those factors that were significantly associated with prolonged LOS found that compared to Hispanic patients, Black patients were 1.22 times more likely to have prolonged LOS, while White patients were 1.53 times more likely to have prolonged LOS (95% CI; p<0.05). Low SES and Non-Home Discharge (4.64 OR) are also the risk factors.
Conclusion: This study highlights several risk factors for prolonged LOS after primary TKA in an urban, socioeconomically disadvantaged, predominantly minority patient population. Overall health status, chronic disease, insurance type (Medicare or Medicaid), low SES, and non-home discharge were associated with prolonged LOS in this population.
Non-narcotic Total Joint Arthroplasty using an Alternative to Opioids (ALTO) Multimodal Pain Protocol: a Comparison of 90-day Outcomes
-
Presenting author: Iciar M Davila Castrodad
-
Additional authors: Thomas A Novack, Michael Pompliano, Jennifer Kurowicki, Ryan A Finkel, John J Callghan, Craig Wright, Anthony Festa, Anthony Scillia, Vincent K McInerney
Introduction: Despite complications, acute postoperative pain management strategies have utilized opioid consumption. At our institution, there has been a system-wide push to reduce opioid prescriptions, as seen in the development of an Alternative to Opioids program within our Emergency Department. Therefore, the purpose of this study was to evaluate outcomes in patients who received an opioid-free protocol after primary lower extremity TJA. We analyzed (1) in-hospital opiate consumption, (2) length of stay, (3) 90-day ED visits, (4) 90-day readmissions, and (5) 90-day complications.
Methods: We retrospectively identified 303 cases of primary TJA for osteoarthritis between January 2017 and February 2019. Patients who received narcotic medications postoperatively were combined into a narcotic group while those who remained opiate-free were combined into a non-narcotic group. Complications were stratified by non-orthopaedic (including all medical concerns), and orthopaedic. Continuous and categorical variables were assessed using Independent samples t-test, Two-way analysis of variance, chi-squared tests, and Fisher exact tests, respectively. A p-value of 0.05 was set as the threshold for statistical significance.
Results: A total of 53 patients (17.5%) received postoperative opiate medication in-house, while 250 patients (83%) were opiate-free. Among THA and TKA patients, there were no significant differences in mean LOS between the narcotic and non-narcotic groups (2.11 vs 2.14 days; p=0.947; 2.17 vs 2.15 days; p=0.947). Among THA and TKA patients, there were no significant differences in 90-day ED visits between the narcotic and non- narcotic groups (11.4 vs 8.0%; p=0.537; 11.1 vs 8.4%; p=0.702). Among THA and TKA patients, there were no significant differences in 90-day readmissions visits between the narcotic and non-narcotic groups (11.4 vs 5.4%; p=0.213; 0.0 vs 5.3%; p=0.315). There were no differences in the rate of orthopaedic complications between the narcotic and non-narcotic groups. There was a significance in the rate of non-orthopaedic complications (5.7 vs 0.8%; p=0.040).
Conclusions: An opioid-free, multimodal pain management pathway is a safe and effective option in patients undergoing TJA, and does not increase length of stay, 90-day complication rates, return ED visits, or hospital readmission rates. Future research will need to further investigate this ongoing issue, possibly in the form of randomized trials, to fully understand how to implement an opioid-free model in total joint arthroplasty.
Tissue-Engineered Augmentation of A Rotator Cuff Tendon Using A Novel Bio-Inductive Biocomposite Scaffold: A Preliminary Study In Sheep
-
Presenting author: Gregory M. Kanski
-
Additional authors: William R Walsh Ph1, Andrew J Carter PhD, Vedran Lovric PhD, James Crowley BVSc, Dan Wills BVSc, Tian Wang PhD, Robert Stanton MD, Steven Arnoczky DVM, Robert Arciero MD
Introduction: Surgical repair of torn rotator cuff tendons has been associated with a high degree of re-tears. Recent studies have shown that augmenting the repair through the induction of new host tissue can prevent gapping or re-tears by increasing the thickness of the tendon. This study investigated the ability of a novel, bio-inductive, biocomposite (high porosity collagen with PLLA microfilaments) scaffold to support the rapid proliferation, maturation, and remodeling of new host tissue in an animal model of rotator cuff tendon repair. The bio-inductive scaffold was hypothesized to rapidly increase the thickness of the repaired tendon through the addition of functional host tissue.
Methods: The porosity of the bio-inductive, biocomposite (collagen-PLLA) scaffold (BioBrace, Biorez Inc.) was measured using mercury porosimetry. Arthroscopic surgical technique of an augmented rotator cuff repair was evaluated using human cadaveric shoulders. Following Institutional Animal Care and Use Committee approval, a mid-portion detachment of the infraspinatus tendon (IST) was created and repaired in 18 sheep using a double row suture bridge, and augmented using the biocomposite scaffold, mimicking human cadaveric technique. Nine animals were humanely euthanized at either 6 or 12 weeks for radiography, micro-computed tomography, MRI, histology, or biomechanical testing.
Results: Mercury Porosimetry: The biocomposite scaffold had an average porosity of 80%, median pore diameter of 19.4 micron, and pore volume of 4.2 cm3/gram*. Surgical Technique:* The implant could be introduced into the joint arthroscopically and incorporated using a double row suture bridge (Figure 1A). Imaging (T2 MRI): The mean thickness in the IST (Figure 1B arrow) of non-operated animals was 3.5 mm while the mean thickness of the repaired ISTs was 10.0 mm at six weeks and 9.8 mm at twelve weeks (Figure 1C/D). Histology: At six weeks the bio-inductive scaffold was infiltrated by host fibroblasts and fibrovascular tissue. Dense, regularly oriented connective tissue was also observed on the superior and inferior surfaces of the scaffold which added to the overall thickness of the healing tendon (Figure 2A). By 12 weeks there was maturation and remodeling of the fibrovascular connective tissue within the scaffold as well as on its inferior and superior surfaces (Figure 2B). Scattered foreign body giant cells (arrows) were observed at both 6 and 12 weeks and were associated with the PLLA fibers (Figure 2C). Mechanical testing: The ultimate tensile strength (UTS) of the repaired IST construct significantly increased between 0 (1163 + 303N) and 6 weeks (1740 + 338N) (p=0.01), and 6 (1740 + 338N) and 12 weeks (2463 +484N) (p=0.01) (Figure 2D). There was no significant difference in UTS between repaired (2463 + 484N) and contralateral control tendons (2707 + 605N) at 12 weeks (p=0.35) (Figure 2D).
Discussion: The collagen-PLLA biocomposite scaffold increased the thickness of a repaired rotator cuff tendon through the rapid induction of host- generated dense, regularly-oriented connective tissue. The new host tissue demonstrated functional remodeling over time resulting in a repair that was as strong as the unoperated control by 12 weeks.
SIGNIFICANCE/CLINICAL RELEVANCE: Healing of rotator cuff repairs has been a challenging clinical problem. In addition, functional outcomes are improved with integrity of the rotator cuff after repair. This study shows that a biocomposite scaffold induced a proliferative healing response that improved the thickness of the repair tissue, and was as strong as controls. This has strong potential as an adjunct for rotator cuff repair.
Impact of Resident Involvement on Complication Rates in Revision Total Knee Arthroplasty
-
Presenting author: Kelly Chandler
-
Additional authors: Roshan Jacob, Mackenzie Sowers, Nick Andrews, Ashish Shah
Introduction: The number of revision total knee arthroplasty (TKA) procedures continues to rise, a direct consequence of the increase in primary TKA. The number of arthroplasty-trained orthopaedic surgeons has failed to increase at a corresponding rate, and the increased burden will ultimately fall on non-specialized orthopaedists. Resident involvement in primary TKA does not increase postoperative complications, but revision TKA is more complex and the impact of resident involvement has not been well studied.
Methods: Using the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database, this study identified 1,834 revision TKA procedures between the years 2008-2012. Of these procedures, 863 included residents. Demographic information, postoperative complications, comorbidities, operative times, and length of stay (LOS) were stratified by resident and non-resident involvement and analyzed.
Results: Resident involvement was not associated with a significant increase in complications, despite a significant increase operative times (147.50 minutes with resident involvement vs. 124.55 minutes without a resident, p<0.001). Resident involvement did produce increased length of stay by 0.34 days, but this did not reach significance (p=0.061).
Conclusion: Resident involvement in revision total knee arthroplasty was associated with a significant increase in operative time; however, there were no significant increases in postoperative complication rates within 30 days. These findings support continued resident involvement in revision total knee arthroplasty cases and postoperative management.
Operative Room Time Comparison between General and Spinal Anesthesia in Total Hip Arthroplasty: An Institutional Review
-
Presenting author: Mackenzie Sowers
-
Additional authors: Roshan Jacob, Kelly Chandler, Nick Andrews, Ashish Shah
Introduction: A relatively high expense with any procedure is total operative time. Two components of this time are the time spent anesthetizing the patient and time spent removing the patient from the operating room (OR) after surgery. This time can be affected by using spinal aesthesia (SA) or general anesthesia (GA).
Currently there is conflicting information about the cost burden of these two techniques in total hip arthroplasty (THA) procedures. This study compares the total time it takes for a patient to be anesthetized and the time until the patient is out of the room, for both spinal anesthesia and general anesthesia, in patients undergoing a primary THA.
Material and Methods: A retrospective chart review was performed at a single institution between the years of 2016-2018. Primary THAs without additional complications performed by one surgeon were selected. The anesthesia note from the procedure was reviewed to calculate total time spent anesthetizing the patient and time spent removing the patient from the OR after surgery. Anesthesia records for 40 patients were used; 20 patients who received SA and 20 that received GA.
Results: The time for a patient to be anesthetized was 48.1 minutes in the GA group and 58.6 minutes in the SA group (p=0.0013). The time spent moving the patient from the operating after surgery was 6.8 minutes in the GA group and 4.4 minutes in the SA group (p=0.0015). When combining these times, the total time of anesthesiologist involvement pre and postoperatively was 54.9 minutes in the GA group and 63.1 minutes in the SA group (p=0.0154)
Conclusion: There was a significant difference in the total time of anesthesiologist involvement in general anesthesia versus spinal anesthesia groups. The total time of anesthesiologist involvement was significantly lower for patients receiving general anesthesia. This and the complications of both GA and SA should be taken into consideration when anesthetizing patients undergoing THA.

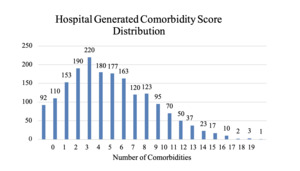
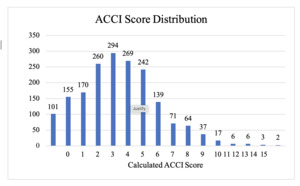
__t2_mri_imaging_of_ists_(arrows)_on_non-o.png)
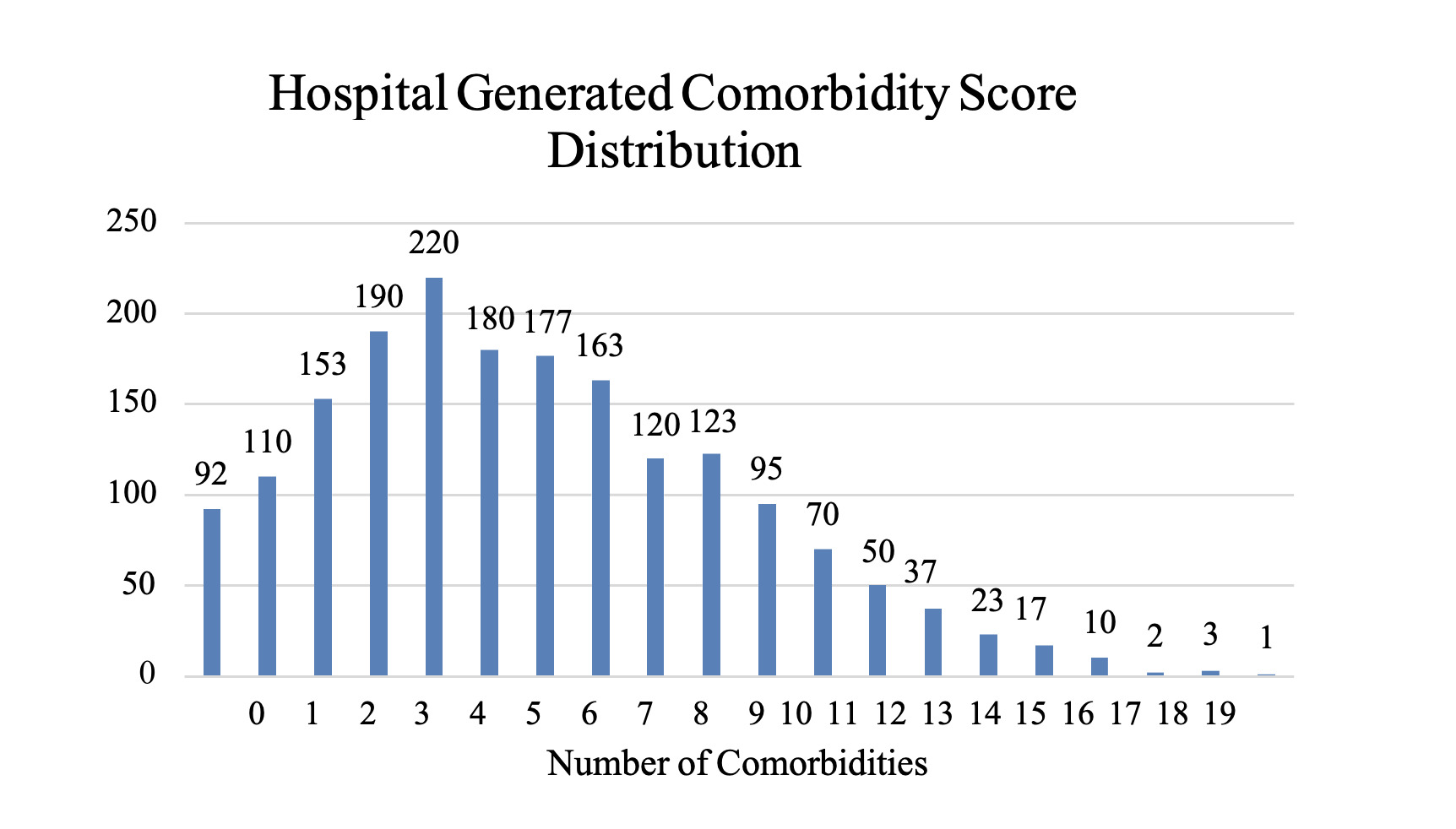
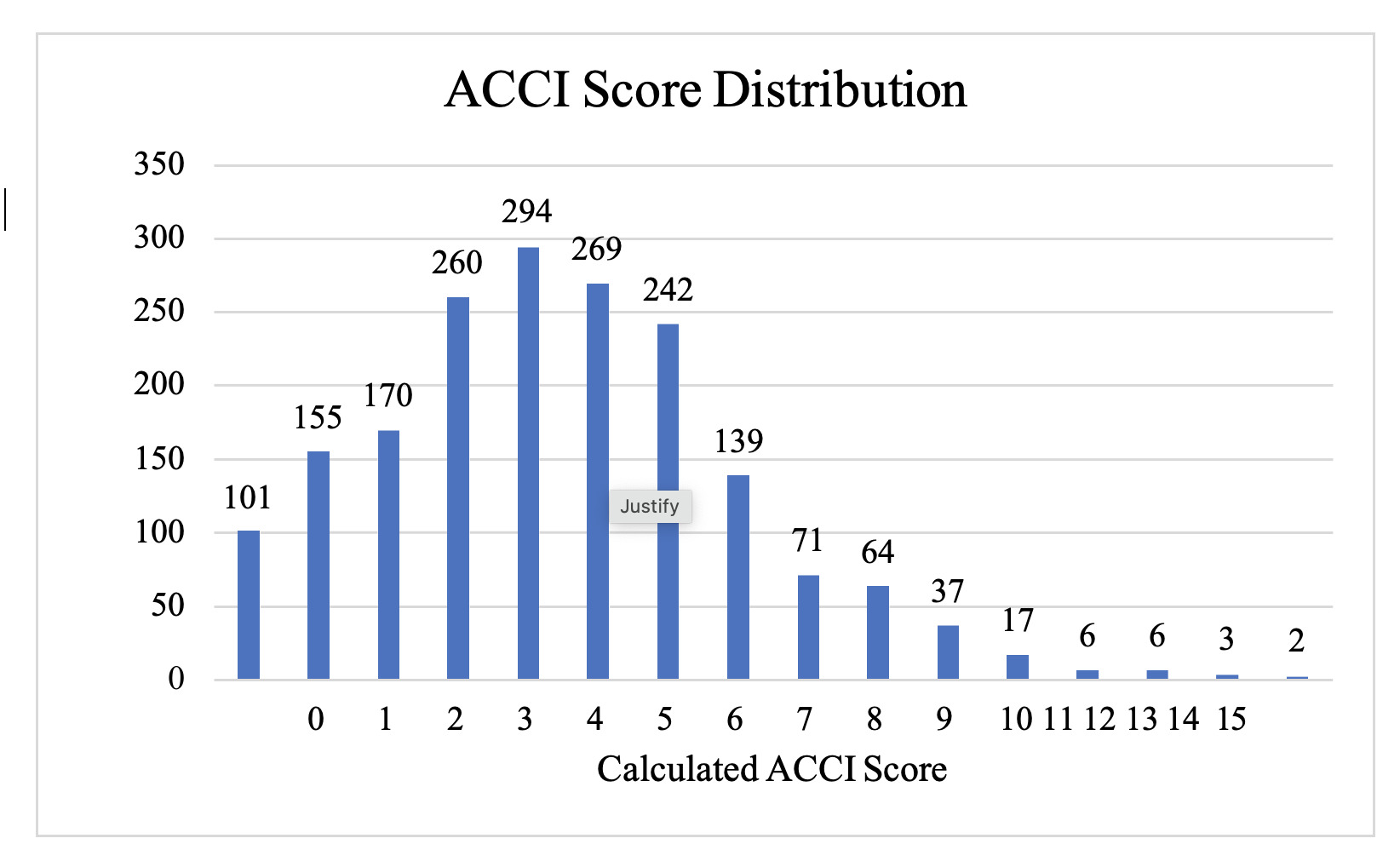
__t2_mri_imaging_of_ists_(arrows)_on_non-o.png)