A 12-year-old little leaguer comes into your office with elbow pain. There is a 100% certainly that you have a complete protocol to take this player from pain and inability to participate in sport to full function. In fact, you can find peer-reviewed published articles with such protocols available for your evaluation.
A 45-year-old patient comes to your office with new onset of low back pain with radiculopathy. As in the case above, there is certainty you have a standard protocol for treatment of this. The treatment may or may not end with surgery, but either way, your treatment protocol is designed to return the patient to function.
In contrast a 62-year-old comes to your office with knee pain and Grade 1 osteoarthritis on radiographs. Maybe you obtained an MRI which confirmed no meniscus tear and the osteoarthritis changes. Maybe you give NSAIDs (but for how long), maybe you offer an injection, maybe this, maybe that. Maybe you bring them back in 3 months for a reevaluation. Maybe you send the patient to their primary care physician. Too many “maybes.”
It is extremely hard to find, in the literature, treatment protocols to treat the entire episode of care of the diagnosis of knee osteoarthritis, ICD 10 17.0, 17.11, or 17.12. There are more than enough protocols published for treatment of the episode of care for the surgery for knee osteoarthritis, CPT 27446 or 27447. As more insurance companies and health systems move to a value-based health care, while CPT bundles are well -developed, ICD bundles are lagging behind. Not only will a wide range of governmental and commercial payors be interested in optimizing ICD bundles, but certainly employer-based insurers will probably lead the way.
The literature is full of articles comparing one non-surgical treatment to another as well as surgical treatment vs. non-surgical treatment in knee osteoarthritis. The problem with these articles is that none really speak to any validated or even experiential comprehensive multi-month or multi-year conservative treatment protocol.
While individually, many of these treatments, including over-the-counter analgesics and over-the-counter or prescription NSAIDs, have solid evidence of having some success it is not clear that there have been widespread attempts to develop treatment protocols that can be separately evaluated.
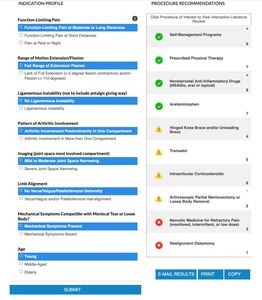
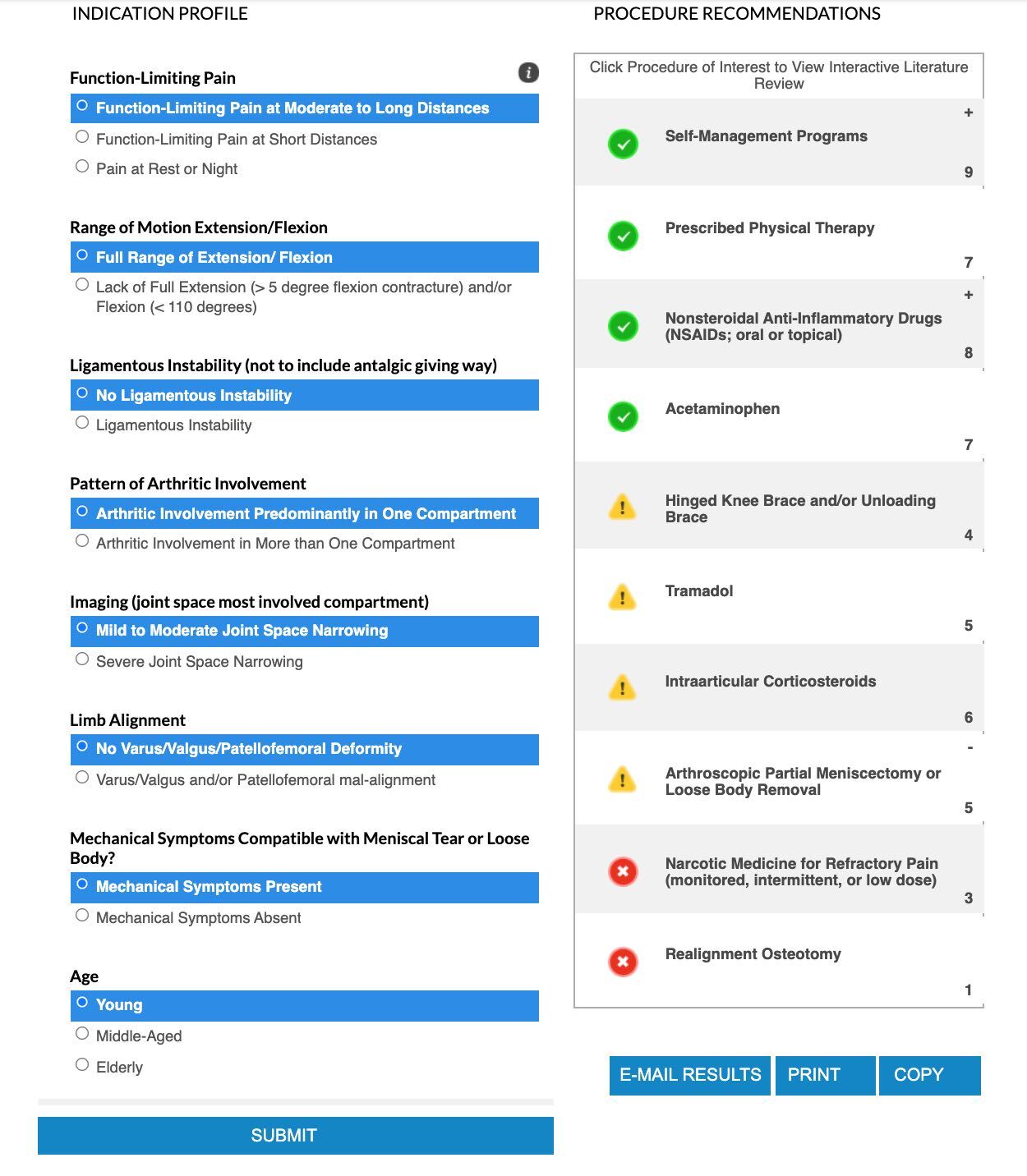
Additionally, the AAOS Appropriate Use Criteria for Non-Arthroplasty Treatment of the knee, while a valuable piece of work, only give procedure recommendations based on your answer to profile questions. Appropriate use guidelines and procedure recommendations are not protocols, though. For example, Figure 1 shows an actual use of the guidelines.
You see that, after you put in the answers you get a series of suggestions but not as actual protocols. Here is what I mean:
-
Self-management programs- what type, for how long
-
Prescribed Physical Therapy- what program, for how long, for three years?
-
NSAIDS- what if the first round does not work and all the answers to your questions are the same- now what is your protocol?
-
Same can be said for acetaminophen
-
All the groups in yellow are a group "may be appropriate- again- in what setting and more importantly, what is your protocol over a three-year period- which corticosteroid, what does, how many times, how often do you reevaluate?
So, while the AAOS Guidelines a superb, they do not speak to an actual, real-practice protocol that is drilled down to actual details. While some may call this cookbook medicine, I would argue that great chefs start with a recipe in a cookbook and then modify based on experience. In the end, they come up with a better product. Where are all those “better” recipes out there? If medicine, in the age of robots, is still an art, what are the protocols of those orthopaedic non-operative artists to produce a great result.
A few examples of selective treatment results, supporting these approaches to be part of a protocol, have discussed injections (Bert et al. 2018), radiofrequency ablation (Orhurhu et al., n.d.), comprehensive “Joint Clinics” (Abbott et al., n.d.), unsupervised general programs (Duong et al., n.d.), non-pharmacologic treatments (Ceballos-Laita et al., n.d.), analysis of factor influencing individualized programs (Gwynne-Jones et al., n.d.), comparison of biologics (Chen et al., n.d.), and more.
I propose the following thought-experiment for all orthopaedic surgeons and for readers to post their answers with their protocols on the LinkedIn JOEI Group.
The patient, Jane Doe, is a 62-year-old female who arrives in your office complaining of moderate knee pain. She has stable hypertension and well-controlled Type II diabetes with an A1c of 7.0. To date, she has only sporadically taken over-the counter acetaminophen and NSAIDs with variable relief of symptoms. Her BMI is 26.1. She comes to you for treatment of her osteoarthritis, but the following situation MUST be respected- she needs to work, as a full-time employed salesperson for a medical device company- making calls on doctor offices, sometimes observing procedures, and so on until she can retire at age 65. She will not agree to any surgery until she retires. Additionally, she is a VIP to your practice, so you don’t want to lose her from your care.
Since it is our experiment, here is what the timeline of her osteoarthritis looks like (and at no point in time does she develop a meniscus tear or loose osteochondral defect that may need surgery):
Age 62-63: Grade 1 osteoarthritis
Age 63-64: Grade 2 osteoarthritis
Age 64-65: Grade 3 osteoarthritis
Age 65: Ready for knee replacement with Grade 4 osteoarthritis
At each year, whether month-to month or quarterly, or some other time period, if you can construct a protocol for such a patient, what would it look like. You can use any FDA approved device, medication, injectable (synthetic or biologic), durable medical equipment, or anything else on the market. You can use nutraceuticals (although not FDA-regulated), any type of physical therapy, or specific exercise modalities.
One more thing. She has employer-based insurance which will pay fully for any and all interventions in your program without preauthorization needed.
What treatment protocols would you construct in this scenario, year-by-year?