INTRODUCTION
Symptomatic knee osteoarthritis (OA) affects 6% of the adult population and occurs in 10% of those over age 60 (Zhang and Jordan 2010). The condition is progressive and results in loss of the articular cartilage and often leads to end stage arthritis of the knee and need for total knee arthroplasty (TKA) (Koenig et al. 2013).
Although TKA is a relatively successful surgical procedure, it should be reserved for patients with end-stage arthritis of the knee. Patients with symptomatic mild or moderate arthritis of the knee may be managed by a variety of non-operative treatment strategies (Feeley et al. 2010). These include physical therapy, weight loss, activity modification, administration of non-steroidal anti-inflammatory medications (NSAIDs), natural occurring oral supplements (glucosamine, etc.), intra-articular injection of corticosteroids and/or viscosupplementation plus others (Feeley et al. 2010; Reginster et al. 2001; Eyles, Lucas, and Hunter 2013). Most of these measures are believed to result in some degree of success for alleviating symptoms and improving function (Buckwalter et al. 2001; Douglas 2012; de Campos et al. 2013). However, administration of NSAIDs and intra-articular injection with corticosteroids carry potential adverse effects and may not be tolerated by some patients (Ashraf et al. 2013; Rashad et al. 1989). In a recent meta-analysis all classes of NSAIDs were shown to result in cardiotoxicity as well as gastrointestinal side effects, if used for a long period of time (“Cardiovascular and Gastrointestinal Safety of NSAIDs: A Systematic Review of Meta-Analyses of Randomized Clinical Trials - PubMed,” n.d.).
A recent study showed that osteoarthritis is potentially caused by dysfunction of the immune system that leads to chronic inflammation (Liu-Bryan and Terkeltaub 2015). Individuals with OA have elevated levels of inflammatory markers such as nuclear factor kappa beta (NF-ϰB), interleukin-1 alpha (IL-1a), IL-6, IL-17, tumor necrosis factor (TNF)- α, as well as many others (Beekhuizen et al. 2013; Rübenhagen et al. 2012). Administration of anti-inflammatory drugs such as NSAIDs, through inhibition of prostaglandin-E2, does result in a reduction in the level of a select group of inflammatory mediators while resulting in overexpression of others, possibly leading to a relative immune imbalance (Ricciotti and FitzGerald 2011).
Despite the availability of some non-operative strategies for the management of symptomatic arthritis in general and the knee in particular, it is not uncommon for patients to fail the aforementioned non-operative treatment measures and continue to be symptomatic. These patients either do not respond to the treatment measures or are unable to tolerate them due to adverse events.
In recent years, attention has been given to potent natural products that are known to have anti-inflammatory properties. Numerous agents have been evaluated with well-designed studies and have shown promising potential for reducing pain and improving function in arthritic patients (Cameron and Chrubasik 2014). While the mechanism of action of these agents in relieving osteoarthritis symptoms is not completely understood, in-vitro studies indicate that certain natural agents may work by reducing pro-inflammatory mediators associated with cartilage damage (Cameron et al. 2009).
The hypothesis of this randomized, prospective and blinded study was that oral administration of a blend of natural anti-inflammatory agents will result in pain relief and improved function, along with reduction of inflammatory mediators in knee joints of patients with osteoarthritis.
METHODS
The Institutional Review Board approval was obtained at each institution participating in the study before patients were approached to enroll during clinic visit. Patients who signed the consent form were randomized using the envelope technique to receive Synogesic® (Group A) or placebo (Group B). Synogesic is a proprietary blend of Turmeric Extract, Ginger Root Extract, Boswellia Serrata Extract, Vitamin C, Vitamin D and Rutin. Patients in the control group received tablets that contained safflower oil only. All patients were instructed to take the administered tablets four times a day. Patients were given a diary to record the time at which the tablets were taken. During the period of the study patients were instructed to stop taking conventional NSAIDs; simple analgesics, such as acetaminophen, were allowed. Consumption of opioid medications for control of symptoms of knee arthritis was discouraged. All other natural oral supplements commonly used for patients with arthritis (e.g. glucosamine) were discontinued. Patients were not allowed to undergo intra-articular injection with any agents for the duration of the study; receiving such treatment resulted in disqualification of the patient for inclusion in the study. Patients unable to tolerate the study pills and/or those with low compliance were also excluded.
Patient Selection
The study recruited 46 consecutive patients with a mean age of 62.6 years (range, 44.3 to 82.5 years) with symptomatic arthritis of the knee and radiographs demonstrating Kellgren-Lawrence grade II or III disease. There were 26 females and 20 males. Patients with systemic inflammatory conditions such as inflammatory bowel disease, psoriasis, eczema, or those with seropositive or seronegative inflammatory arthritis of the knee such as rheumatoid arthritis or ankylosing spondylitis were excluded from the study. It was ensured that none of the patients had received intra-articular injection of any agents into the affected knee within 3 weeks prior to the enrollment (Appendix A summarizes inclusion and exclusion criteria).
Patient Assessment
The patients were clinically evaluated at baseline (at the time of signing the consent form and enrollment in the study), and 12 weeks after enrollment. Various patient reported outcomes measures (PROM) were recorded at both time points. At the first evaluation, patients were also assessed by the Lequesne’s Functional Index score (LEQ) and a full clinical knee examination was performed. Knee range of motion was measured using a goniometer and recorded. Aspiration of the knee joint was performed under sterile conditions at baseline and after 12 weeks to obtain between 3-5 ml of fluid (total of 2 synovial fluid samples). If at first attempt an inadequate amount of fluid was obtained or the tap was deemed to be dry, then a second attempt was made either during the same encounter (if the patient was willing) or a few days later. For patients with two aspirations producing no fluid, no further attempts for withdrawal of synovial fluid were made. The synovial samples were stored at -30 C and sent in batch to Myriad RBM (Austin, TX) for measurement of 41 inflammatory markers (Appendix B) at the completion of the study.
Outcome Measures
The primary outcome of interest was improvement in pain and function based on PROM. Questionnaires included the Visual Analog Scale (VAS) for pain, Western Ontario and McMaster Universities Arthritis Index (WOMAC) and the Knee injury and Osteoarthritis Outcome Score (KOOS). Secondary outcome assessed was the change in the level of inflammatory mediators in the synovial fluid of patients who received the interventions versus placebo. It was hypothesized that those receiving the active agents would have a more significant drop in the level of inflammatory markers compared to patients receiving the placebo.
Statistical Analysis
We calculated a sample size to detect a 30% difference in VAS scores between the treatment and the placebo groups based on a previous study assessing the effect of Boswellia serrata in treating knee osteoarthritis (Ammon et al. 1993). With a power of 80% and an alpha error of 0.05, a sample size of 16 patients in each group was determined. Assuming a 20% drop out rate, our aim was to recruit 20 patients in each group. Differences in PROM (VAS, WOMAC and KOOS) were compared within each treatment group between baseline and 12 weeks following enrollment using paired sample t-test. Mean change (delta) in inflammatory markers between baseline and week 12 were compared between the 2 groups for each marker separately using independent sample t-test. To assess the global anti-inflammatory effect, the percent change was calculated for each marker and the mean percent change for all markers was compared between the treatment group and the control groups using the t-test. The mean change in each synovial marker between the 2 time points was also used for dichotomizing the cohort; a negative mean change represents a decrease in that marker levels, while a positive mean change represents an increase in that marker levels. A chi-square was then used to compare the net marker reduction between the 2 groups.
RESULTS
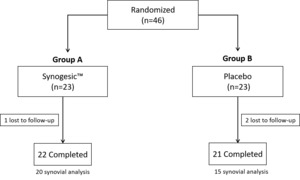
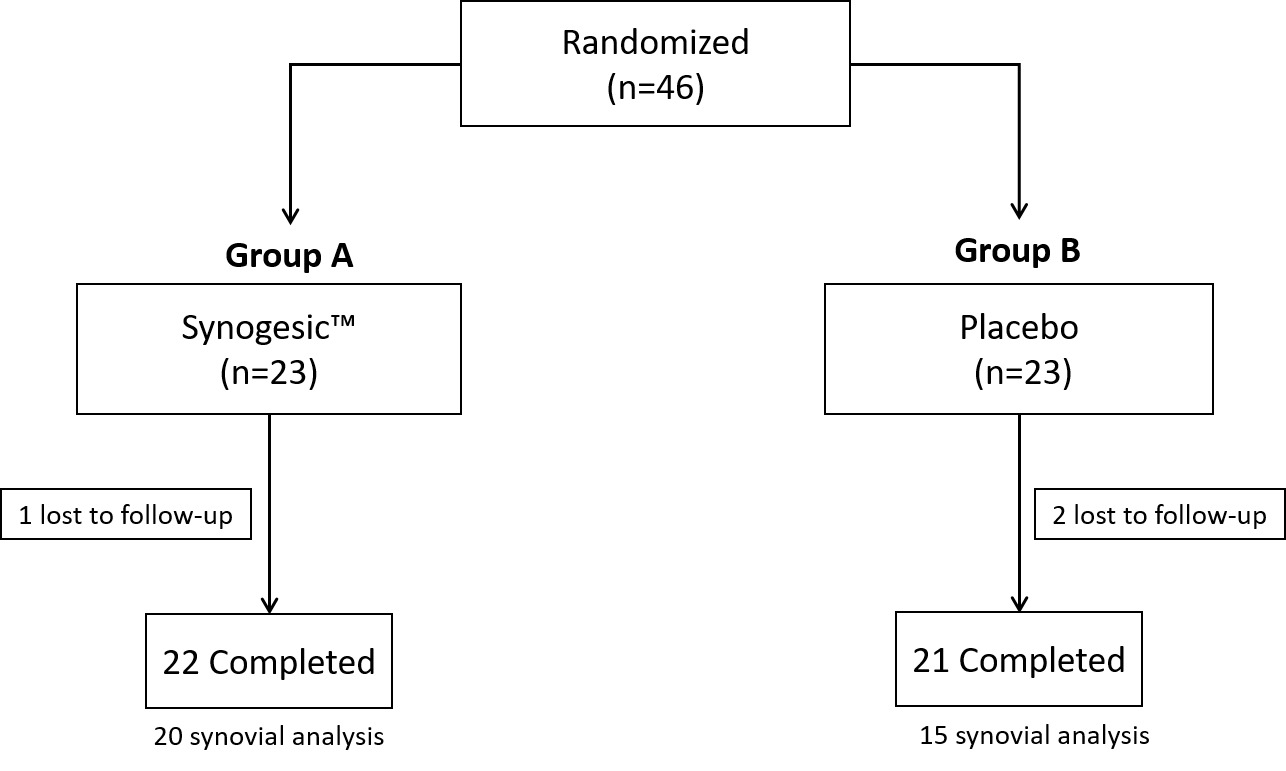
Of the 46 patients who met the inclusion criteria and agreed to take part in this study, 43 patients (22 in Group A and 21 in Group B) completed the 12 week study period (Figure 1). Two patients from Group B and one from Group A were lost to follow-up. There were no differences in demographics and baseline characteristics between the 2 study groups (Table 1). There were no adverse events associated with treatment.
Functional Outcomes and Pain Scores:
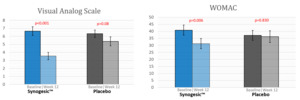
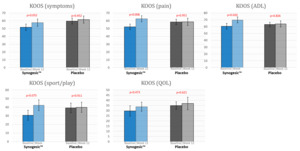
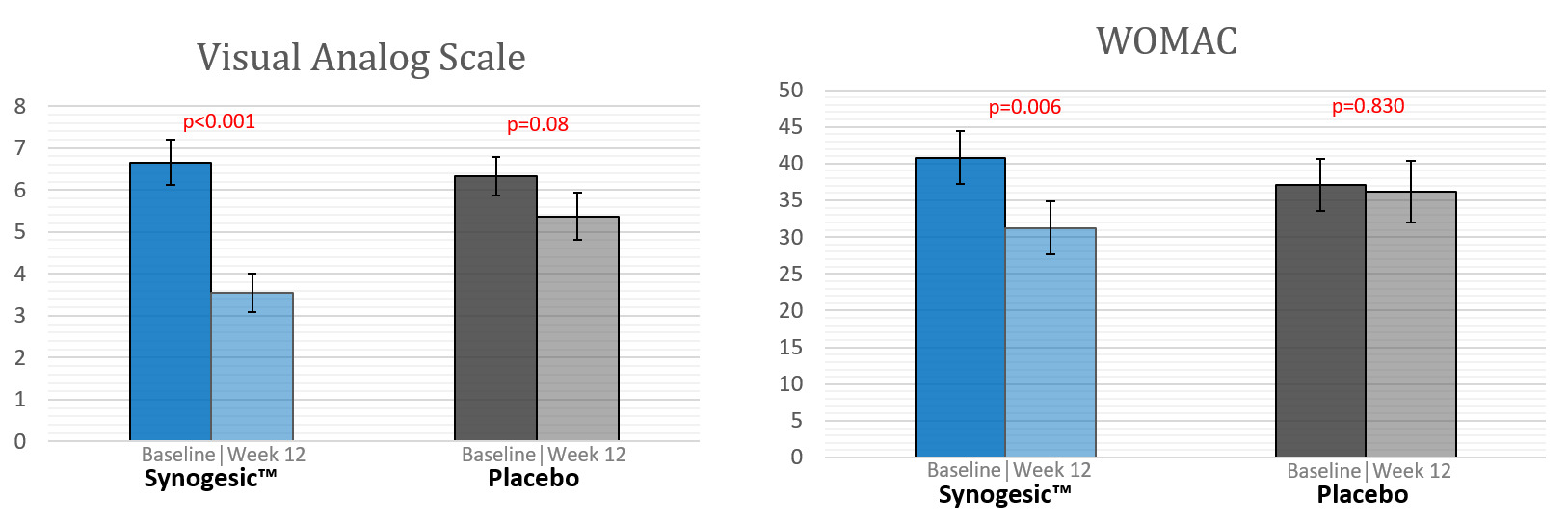
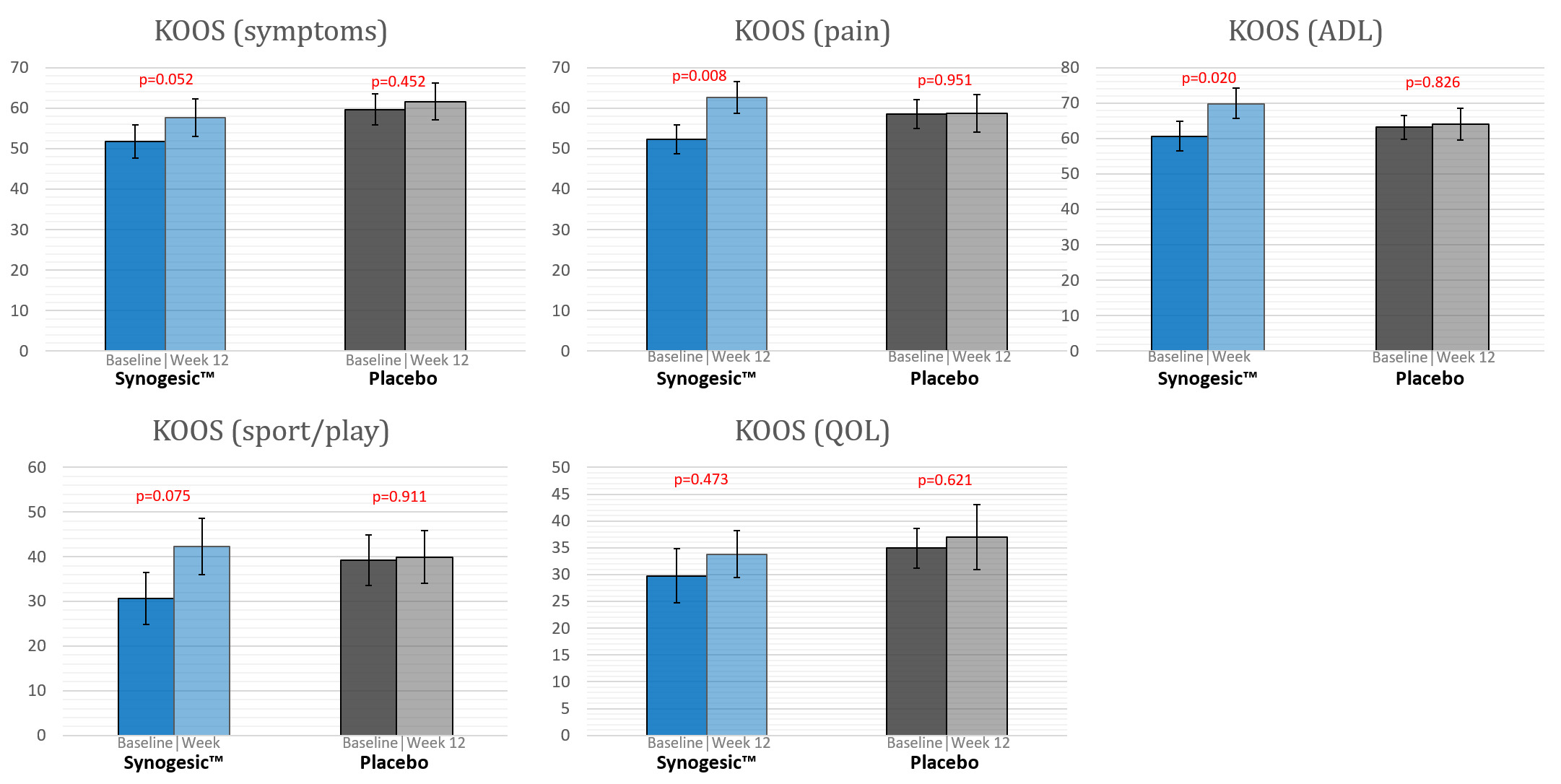
Patients in Group A reported statistically significant improvement in pain and function at 12 weeks compared to baseline, whereas patients in Group B showed no statistically significant benefit between the two time points (Table 2). In Group A, significant difference between week 12 and baseline were seen in VAS (46.8% reduction, P < 0.001) and WOMAC (23.4% reduction, P = 0.006) scores (Figure 2). KOOS for pain (19.8% increase, P = 0.008) and ADL (14.9% increase, P = 0.02) improved significantly, and marginally significant differences were noted in symptoms (11.2% increase, P = 0.052) and sport/play (37.9% increase, P = 0.075) scores (Figure 3). In Group B there was no significant improvement between baseline and week 12 in any of the PROM assessed.
Change in Synovial Biomarkers:
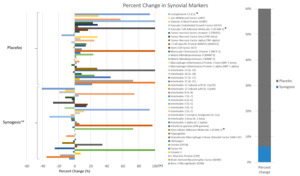
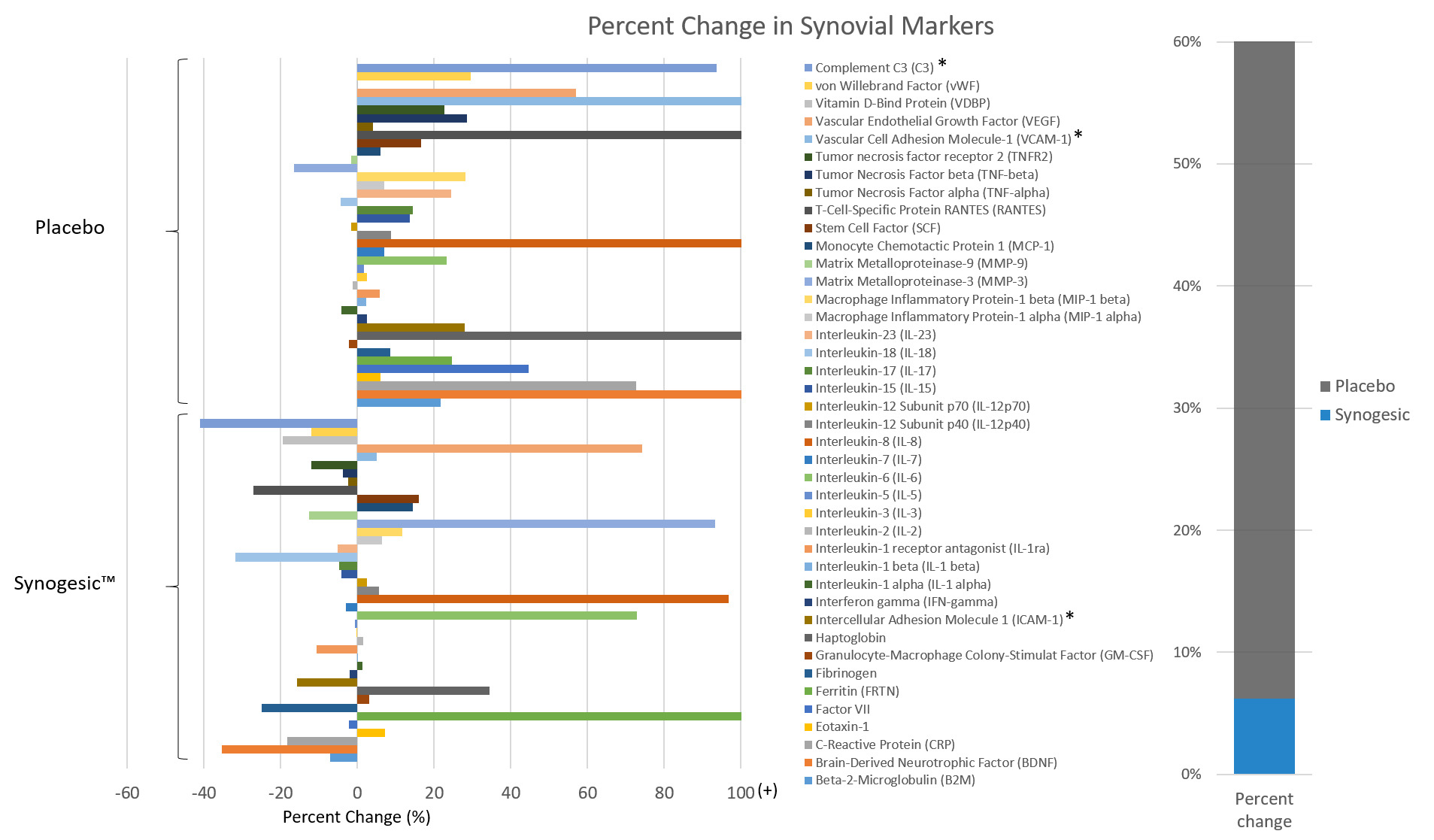
Synovial samples at baseline and 12 weeks were available for 35 patients (20 from Group A and 15 from Group B). Of the 41 pro-inflammatory markers examined, 26 (63.4%) decreased in Group A, while only 13 (31.7%) decreased in Group B (P = 0.008). The percent change from baseline levels seen in Group A (6.2% increase) was significantly lower (P = 0.018) compared to that seen in Group B (54.5% increase) (Figure 4). Markers that stood out and that showed significant between group differences were: Intercellular Adhesion Molecule 1 (ICAM-1), Vascular Cell Adhesion Molecule-1 (VCAM-1) and Complement C3 (C3) (P = 0.03, 0.02, 0.04, respectively). The average change (delta) for each marker is presented in Appendix B.
DISCUSSION
This level I study demonstrated a potential mechanism by which natural agents may alleviate symptoms of knee osteoarthritis by reducing the action of synovial fluid inflammatory mediators. The reduction in the level of these inflammatory markers corresponded with an improvement in pain and function in these patients.
Naturally occurring anti-inflammatory agents through a broad mechanism of action inhibit both lipoxygenase and cyclooxygenase pathways, as well as the complement system (Ammon et al. 1993; Kapil and Moza 1992; Abe, Hashimoto, and Horie 1999). They also directly inhibit metalloproteinase and the ensuing cartilage destruction (Saja et al. 2007). Natural agents such as Boswellia, Turmeric, Vitamin C and Ginger, through in-vitro studies, have been shown to reduce inflammatory markers (“Anti-Inflammatory Activity of Boswellia Serrata Extracts: An In Vitro Study on Porcine Aortic Endothelial Cells,” n.d.; Sahebkar et al. 2016; Carr and Maggini 2017; “Journal of Medicinal Plants Research - in Vitro Anti-Inflammatory Activity of Ginger (Zingiber Officinale Rosc.) Rhizome, Callus and Callus Treated with Some Elicitors,” n.d.). Our findings support the anti-inflammatory properties of the latter products in the human synovial fluid. The study demonstrated that more than 60% of the pro-inflammatory markers examined declined with the administration of natural anti-inflammatory products. The level of VCAM and ICAM, which have been shown to play an important role in endothelial-leukocyte interactions during inflammation and have been a target for treatment in patients with OA (Karatay et al. 2004; Ulbrich, Eriksson, and Lindbom 2003), were significantly reduced by natural anti-inflammatories in our study. The decline in the level of some of these markers did not reach statistical significance (Figure 4), which may be due to the relatively small sample size in the study.
Other studies examined the effect of some of these natural occurring agents (individually) on serum inflammatory markers in humans (Sahebkar et al. 2016; Panahi et al. 2016). These investigations demonstrated a decrease in pro-inflammatory cytokines following treatment. However, these studies were conducted in patients with a systemic pro-inflammatory state. In patients with lower levels of systemic inflammation, such as those with OA, this effect seems to be less obvious (Derosa et al. 2016; Cheras et al. 2010). Rahimnia et al. (Rahimnia et al. 2014) examined the effect of curcuminoids on serum levels of IL-4, IL-6, TNF-α, TGF-β and high-sensitivity (hs) CRP and ESR in mild to moderate knee osteoarthritis. They reported a reduction in IL-6 and hs-CRP levels at 6 weeks compared to baseline, but there were no significant differences compared to placebo (P > 0.05). Unlike prior studies examining serum pro-inflammatory markers, we examined synovial markers in the present study and were able to demonstrate a significant reduction between treatment and control groups. These results suggest the local effect of these products might outweigh their systematic effect and be responsible for the clinical improvement seen in our patients.
In an attempt to compare the patient’s global inflammatory status between the 2 groups, we averaged the mean percentage of change for all markers. While the mean change increased by more than 50% in the control group, only a slight increase from baseline was seen in the Synogesic group and these differences were statistically significant. The slight increase seen in the latter group could be attributed to the fact that participants were instructed to stop NSAIDs immediately before the study period and synovial marker levels at baseline may have been affected by this treatment. Nonetheless, the small change in the Synogesic group compared to the control group suggests efficacy equivalent to a NSAIDs and superiority over the placebo.
Earlier randomized control trials focus mainly on clinical and functional improvement using these agents with promising results (Cameron and Chrubasik 2014; Bost, Maroon, and Maroon 2010). We add further strength to the previous findings, by demonstrating that natural anti-inflammatories reduced pain and improve function; in the present study there was a 46.8%% reduction in pain levels based on the VAS score in patients treated with natural occurring anti-inflammatories. Whereas earlier studies postulate this improvement is secondary to reduced cytokine levels, they base this assumption mainly on in-vitro models. Our study confirms these experimental observations in humans and correlates them with clinical outcomes.
The main limitation of the present study is the limited number of patients in each group. There were also a number of patients in the cohort for whom synovial markers were not available due to a dry aspiration. This possibly contributed to the lack of significance in some of parameters evaluated. Nevertheless, only a small number of patients dropped out of the study and those with complete analysis were sufficient to show significant clinical and laboratory improvement. Another limitation was that the product included several anti-inflammatory agents working through different mechanisms. Thus, it is impossible to know the relative effect of each agent on the outcomes. Finally, we followed the patients for 12 weeks and we cannot state whether the improvement in pain and inflammatory markers continues with long-term treatment. Future studies should focus on the long-term effect of these agents and the potential interactions with other agents.
CONCLUSION
Natural anti-inflammatory agents hold great promise in the management of patients with arthritis, as they may reduce inflammation while avoiding the potential serious adverse effects of pharmacologically produced drugs. These agents have been shown in this study to reduce intra-articular inflammatory mediators that correlated with an improvement in pain and function of the knee in the treated patients. The findings of this study have important implications in an era where the cardiotoxicity of conventional anti-inflammatory drugs has been recognized.

.jpg)
.jpg)