INTRODUCTION
Worldwide, musculoskeletal conditions contributes half the cases of disability and is the leading contributor to chronic pain (World Health Organization 2018). Given the widespread nature of musculoskeletal conditions, the pain can originate from many parts of the body such as shoulders, hips, knees, and hand. However, the most common form of disability is back pain. This in turn can significantly impact the quality of life.
Unlike other areas of clinical specialties such as cardiovascular health’s use of blood pressure, orthopaedics lacks a standardized tool for measuring health status. The introduction of Patient-reported Outcome Measures (PROMs) offers the means of providing a more holistic approach to understanding the health status of a patient that a biomarker would not be able to assess. By tailoring clinical focus on patient reported interpretations of the severity of symptoms of musculoskeletal conditions, and focusing less on physiological markers, clinicians can offer more accurate care. The Arthritis Research UK Musculoskeletal Health Questionnaire (MSK-HQ) was specifically designed by physicians and patients to target the most relevant health domains such as pain, mobility, sleep, social interactions, understanding of condition and treatment, and overall impact. This also gives the opportunity for physician and patient to observe the longitudinal progression of the condition and response to treatment (Hill et al. 2016).
It is important to note that the MSK-HQ was originally developed as a potential candidate as standardized tool for longitudinal health status assessment for musculoskeletal conditions. The aim of this study is to use the MSK-HQ as a tool to investigate the health status and health literacy in an urban setting. The study was conducted in the Bronx, United States. As the most diverse diverse area in the United States, the Bronx population has a patient population that require a unique set of needs. The BronxCare Health System offers care primarily to the South Bronx. It is notable that the South Bronx is the poorest district in the nation with a rate of 28.6% residents living below the poverty line (United States Census Bureau 2017). Additionally, a large portion of the population have Spanish as their primary language. 46.5% of residents registered Spanish as the language spoken at home (Statistical Atlas 2018). Another striking component of the South Bronx demographic is the high rates of overweight and obese residents. 41% of the population is classified as overweight and 25% of the population is classified as obese (Bronx District Public Health Office 2007). These factors distinguish the Bronx as an urban setting with a unique set of needs that influence the health status of musculoskeletal patients. Health literacy is also a critical component of a patient’s well-being in response to their condition and treatment.
In this study the primary objectives are: (1) identify the relationship between musculoskeletal PROMs with the demographic trends of the Bronx; (2) evaluate the impact of health literacy on PROMs from the perspective of physician and patient; (3) conduct internal analysis of the MSK-HQ to identify trends between individual items and the overall PROMs with the 4 musculoskeletal cohorts; (4) evaluate leading factors that contribute to the disparity in health care and how to increase access to affordable and quality care in an urban setting.
METHODS
The Musculoskeletal Health Questionnaire (MSK-HQ) that was developed by the Arthritis Research UK was utilized as a tool to measure health status and health literacy in an urban setting. The role of this study is determine the relationship Patient Reported Outcome Measures (PROMs) due to musculoskeletal conditions and environmental factors of an urban setting (Hill et al. 2016). While studies have been conducted with the MSK-HQ in the United Kingdom, this is the pilot study in the United States.
The study was conducted in the South Bronx in the Orthopaedic Outpatient Clinic at the BronxCare Health System. A total of 83 patients were screened with the MSK-HQ. However, 2 patients were excluded from the study on the basis of age. Sex, age, English as a second language, and BMI were collected before clinical evaluation. The study’s patient population included 24 males and 57 females aged 12 to 82 with an average age of 51.6. 29 patients reported English as a second language. The average BMI is 31.0. The total number of patients were divided into 4 cohorts based on their musculoskeletal condition; spine (n=21), hand and upper extremity (n=29), sports medicine (n=16), and total arthroplasty candidates (n=16).
The MSK-HQ is a 15-item survey that assesses Patient Reported Outcome Measures (PROMs) and levels of physical activity of those afflicted with a musculoskeletal condition (Figure 1). The questionnaire encompasses the primary health domains that assess the level of disability of a patient. It offers a series of items such as pain, movement, employment, social activities, sleep, emotional well-being, and comprehension of one’s condition and treatment to gain a holistic perspective of the impact of PROMs on the quality of life. Each item has a score range of 4-0. As the numeric value decreases, the severity of disability increases for each item. Note that at the end of the survey there is an item that addresses physical activity levels that ranges from none-7 days during a week interval. This supplemental item is excluded in the total scoring. The total score is the summation of the 14 items. The minimum score of the questionnaire is 0 and maximum score is 56. A decrease in the total score indicates an increase in musculoskeletal disability (Hill et al. 2016).
The patients were individually screened with the questionnaire during their nonoperative clinical visit. The questionnaire was administered verbally and recorded by trained hospital staff. Those that declared English as a second language were screened with the aid of a telephone translator. The time duration of each of survey that was administered took approximately 5 minutes per patient.
Multivariable analysis was performed using linear regression models to evaluate the correlation between age, BMI, sex and PROMs. Separate multivariable linear regressions were created for each of the cohorts of patients that were seen by different outpatient providers. Namely, hand and upper extremity, arthroplasty candidates, sports, and spine were each correlated to PROMs, age, BMI, sex, and each of the reported score for the fourteen questions on the MSK-HQ. The patient reported understanding of condition and current treatment was also compared using a linear regression to provider-report interpretation of patient understanding of condition. The providers were blind to patient reports. The magnitude of the association was obtained as the correlation coefficient for each of the variables. P value < 0.05 was used as the level of significance. Statistical analysis was carried out using XLSTAT.
RESULTS
The initial study patient population consisted of 83 patients from the initial screening. However, 2 patients were excluded due to the failure to meet the age requirement of a minimum of at least 12 years. The mean age was 51.6 years old ± 14.1 years. There were 57 (70.37%) females and 24 (29.63%). The mean BMI was 31.0 ± 7.9. There were 12 (14.81%) patients that classified under normal weight conditions, 32 (39.51%) overweight, and 37 (45.68%) obese (Table 1).
The clinical participants were further divided into 4 cohorts by their musculoskeletal condition; spine (n=21), hand and upper extremity (n=29), sports medicine (n=17), and total arthroplasty candidates (n=16). The mean Patient Reported Outcome Measures (PROMs) for spine was 22.14, 31.46 for hand, 24.56 for sports, and 26.81 for arthroplasty candidates. The mean score for the patient’s understanding of condition and treatment for spine was 1.9 for spine, 2.36 for hand, 2.38 for sports, and 2.38 for arthroplasty candidates. The average physical activity level for the spine cohort was 3.05, 3.5 for hand, 3.5 for sports, and 3 for arthroplasty candidates (Table 2).
The questionnaire was evaluated by a numeric grading scale. Each individual item had minimum score of 0 and a maximum score of 4. The mean and the standard deviation for each questionnaire item is recorded below (Table 3).
The PROMs were calculated through the summation of each of the 14 items. Each item was then further analyzed by identifying the relationship of the individual item with the PROMs. Items 2, 5, 6, 9, and 14 demonstrated significant correlation with the total PROMs as each had a p-value of less than 0.0001 (Table 4). Each of the questionnaire items that exhibited a strong correlation with the total PROMs illustrates a positive trend. As the item scoring increases, the total PROMs also increases (Figure 2).
The patient’s understanding of their condition and treatment was a component of the MSK-HQ. This was measured against the total PROMs. It was shown that as the patient’s understanding of their condition and treatment increased, the total PROMs also increased (Figure 3).
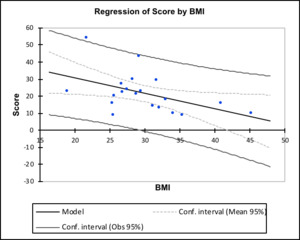
Each of the musculoskeletal cohort’s PROMs was compared to the overall BMI of its respected cohort. The PROMs of the spine cohort illustrated significant correlation with the BMI. As the BMI increased, there was a decrease in the total PROMs. The remaining cohorts, hand, sports, and arthroplasty candidates did not exhibit a correlation between PROMs and BMI (Figure 4).
DISCUSSION
The Musculoskeletal Health Questionnaire provides a comprehensive and standardized patient reported outcome measures (PROMs) for the overall health of patients afflicted with varied musculoskeletal conditions. The Arthritis Research UK developed the MSK-HQ as a potential candidate for the gold standard of musculoskeletal patient reported outcome (Hill et al. 2016). While it has gained traction as a tool for PROMs in the United Kingdom, there has been a lack of international recognition. This study is the first to use the MSK-HQ in an urban environment within the United States. This study location has further validated the MSK-HQ as a potential universal standard of PROMs for musculoskeletal conditions due to the compliance of physicians and patients during this study trial. There were no indications that difference in clinical cultures between the United Kingdom and United States would affect the baseline reliability of the MSK-HQ. Thus, the MSK-HQ has been identified as a useful tool for studying the health outcomes of those afflicted with musculoskeletal conditions in an urban setting. The South Bronx, New York is composed of a patient population with markedly low income, high BMI, high ESL, as well as increased risk of comorbidities (United States Census Bureau 2017; Statistical Atlas 2018; Bronx District Public Health Office 2007). Given the unique problems in this patient population, the MSK-HQ provided insight into the factors that contribute to poor health outcomes within this community and provided information on the needs that are most lacking in the South Bronx.
It was shown that there was no significant correlation between sex and PROMs. This finding contradicts previous studies that demonstrate that sex influences the severity and occurrence of musculoskeletal conditions. Furthermore, the absence of a significant correlation between sex and musculoskeletal PROMs can offer an additional perspective for physicians on the controversy of providing different forms of orthopaedic treatments based upon sex (American Academy of Orthopaedic Surgeons 2015). However, it is important to note that the patient population of this study contained more females (70.37%) than males (29.63%). This may influence the validity of this finding, so further studies with larger sex cohorts should be implemented. It was also found that patients seen in the outpatient setting for spinal conditions had PROMs that were negatively correlated with increasing BMI. This supports previous studies indicating that there is a correlation between BMI and back pain. As back pain is often nonspecific, this finding may propel future studies to further investigate the role of obesity in back pain. However, it is also important to note that BMI fails to recognize the difference in adipose tissue and adipose free tissue and the variation of body fat composition in males and females (Tormey et al. 2018). Given its shortcomings, it offers baseline insights that increasing BMI is also a risk factor for diabetes, cardiovascular disease and other comorbidities which would also decrease PROMs and overall health. The PROMs across all musculoskeletal conditions were correlated with total physical activity, where increasing activity level predicted higher PROMs. This demonstrates that a higher level of physical activities that a patient engages in is a accurate indicator of the overall good health. There is also the notion that an increase in physical activity may serve as a therapy tool for alleviating the effects of musculoskeletal conditions (Chou et al. 2016). This places emphasis on the need of basic physical activity in order for patients to increase their overall wellbeing.
It was also shown that there was no correlation between English as a second language (ESL) and PROMs. This finding is most likely the result of a telephone translator for every patient that indicated English was not their first language. This finding affirms the previously reported success of telephone translators in communicating with patients (Mas et al. 2013). However, because a large proportion of patients require translating services, a more in-depth analysis of written and telephone translation should be conducted to confirm consistency across communication platforms (Regenstein and Andres 2014).
The driving questions of the MSK-HQ in this urban patient population were determined based upon the p-values of the correlation between the PROMs and each of the individual questions in the MSK-HQ. The questions with the strongest correlation, or the smallest p values, were found to be (2) presence of pain and stiffness during the night, (6) pain or disability interfering with work and daily life, (5) physical activity level, (9) sleep, and (14) overall impact on health. These findings are consistent with previous research that has shown a correlation between obesity, a decrease in sleep, and decreased overall health (Jarosz et al. 2014).
As it is known that urban settings are a risk factor for low health literacy, the patients’ understanding of their condition in relation to their PROMs was also assessed (Jarosz et al. 2014). The patients with the lowest PROMs, meaning patients seen in clinic for spinal conditions, also reported the lowest understanding of their condition and any current treatment. This finding is quite significant because it affirms that low health literacy as a risk factor for low health outcomes (Valerio et al. 2016; Tormey et al. 2018). The physicians within each of the four cohorts were also asked to report on their perception of their patients’ health literacy. There was a consensus from the respective physicians affirmed that their patients did not demonstrate accurate understanding of their condition and treatment. The correlation between health literacy and overall health outcome has the potential to lead to interventions within urban communities that work to combat low health literacy as a way of increasing PROMs.
CONCLUSION
This study is the first to apply a streamlined musculoskeletal health questionnaire to an urban setting within the United States. It affirms that the MSK-HQ can be successfully applied to patient populations in the the United States. The responses indicate that patients within an urban population are most crippled by spine musculoskeletal conditions, correlating with increased BMI and decreased score on the question asking “understanding of health condition and treatment”. Hence, the leading factors that contribute to the the disparity in health in urban settings are increased BMI and low levels of health literacy. This finding was affirmed by physician reports of their patients’ poor health literacy affecting health outcomes. This places significance on the need to increase health literacy in urban settings through the collaboration of clinicians and educating urban communities. These findings can lead to the development of future research surrounding comorbidities and social driving forces that impact musculoskeletal conditions to increase health access to affordable and quality care in the an urban setting.




.jpg)




.jpg)