Introduction
The CDC has declared that in 2018, 32% of the 47,000 overdose deaths involved prescription opioids (Wilson et al. 2020). As orthopedic surgeons, we strive to provide the most comfortable, safe and pain-free experience for our patients. Unfortunately, elective surgery has become an inadvertent gateway into the opioid crisis. Studies have shown that the likelihood of prolonged use of Opioids increases the longer the patient is prescribed them (Shah et al. 2017; Callinan et al. 2017). The most common reason for initial prescription is post-surgical pain management, most commonly prescribed by the surgeon (Shah et al. 2017; Callinan et al. 2017). Prescription opioids not only put the patient at risk for addiction and dependency, but they also provide a source for the spread and misuse of opioids into the patient’s community. This is not to mention the costly toll prescription opioids take on the US healthcare system, that spends over $50 billion on the sequela of opioid addiction (“Costs of Substance Abuse,” n.d.).
It’s abundantly clear that an opioid-sparing approach is necessary and beneficial to all. In fact, there have been multiple evidence-based reports to date that demonstrate opioid-sparing surgical tactics. These studies have demonstrated safe and effective surgical outcomes, while minimizing the exposure to opioid medications. Dr. Nirav Amin reported on an expert panel that outlined pre- and intra-operative guidelines for the use of Liposomal Bupivacaine (LB) in hip fracture surgery (Amin, Hutchinson, and Sanzone 2018). The panel concluded that local infiltration of LB is effective at controlling pain and reducing opioid requirements. In addition, Dr. Andrew Wickline’s 12 week study utilizing an aggressive multimodal pain management protocol showed that 86.3% of patients undergoing total knee arthroplasty (TKA) required 10 pills or less and 18.9% required no opioid pills at all (Stevenson and Wickline 2020). Opioid-sparing techniques are certainly not understudied and produce promising results.
Multimodal protocols that significantly reduce post-operative pain and limit opioid exposure also include a team-based approach to surgery that emphasizes the necessity of communication. This approach is best described by Dr. Zeev Kain, who coined the “Perioperative Surgical Home” (PSH), a model that begins at the moment the operation is scheduled and ends 30 days post-surgery (Desebbe et al. 2016). The PSH ensures coordination of care from staff to physician to caregivers in order to effectively manage pain and patient expectations. It is imperative that opioid-sparing approaches target preoperative care. In a pain management study following carpal tunnel release surgery, Dr. Asif Ilyas found that preoperative opioid counseling reduced opioid consumption by 30% in his patients following surgery (Alter and Ilyas 2017). This is a practice we implement as well. A comprehensive discussion on the plan for perioperative pain management is discussed with all of our patients at the time of surgical consent in the office. In addition, prior to TKA, our patients undergo a preoperative appointment to review all relevant medical data, including consults and lab results and to educate the patients on what to expect the day of surgery. Furthermore, all of our TKA patients must attend a mandatory preoperative class, in which they learn important pain management strategies.
The discussion of pain management continues throughout the perioperative experience. As mentioned, initial pain management strategies are discussed at the time of surgical consent. They are reiterated in the holding room prior to surgery and emphasized by the entire perioperative team in the PACU prior to discharge.
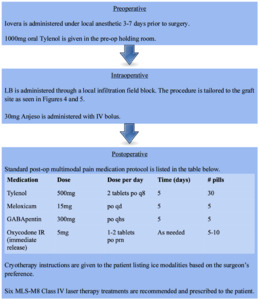
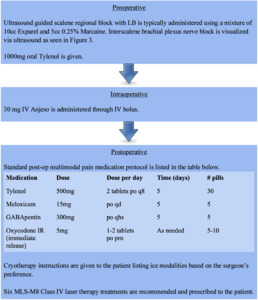
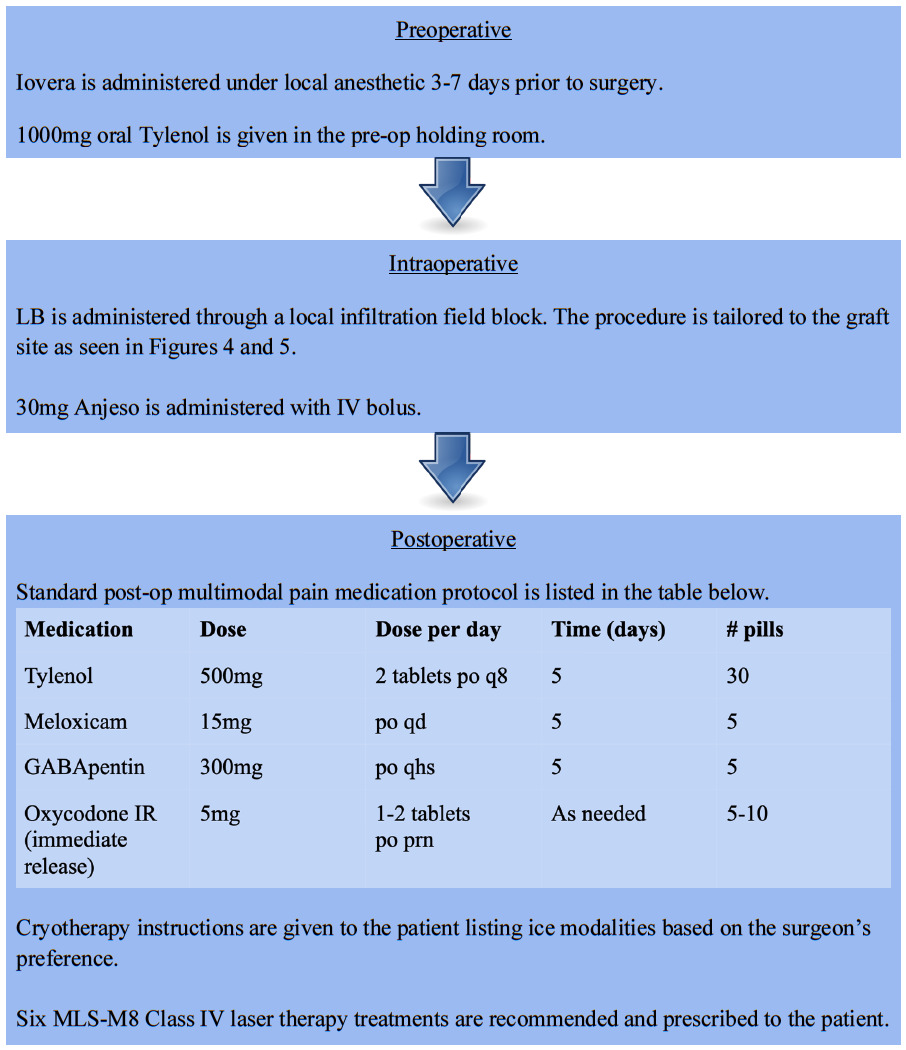
Specific protocols have been established for each of the time windows involved in the perioperative surgical experience. We use a combination of medications, medical devices, local and regional anesthetics to minimize pain while trying to avoid Opioids. The specifics of the preoperative, intraoperative, and postoperative protocols will be outlined below.
Alternative Non-Opioid Pain Modalities
Iovera
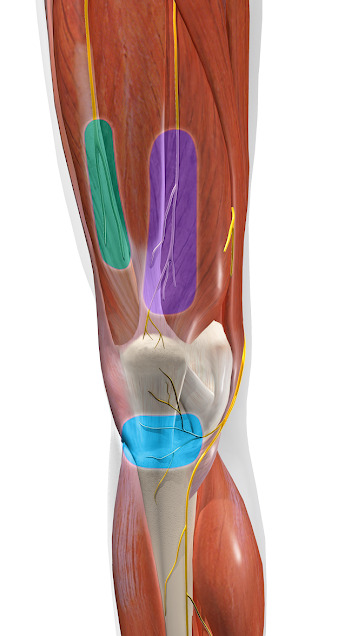
Iovera involves the use of a cryo-axonotmesis device that creates temporary axonotmesis to the anterior femoral cutaneous nerve as well as the infrapatellar bursa at the saphenous nerve. This procedure does not ablate the nerves; it freezes them such that there is no permanent loss associated. Iovera can provide significant pain relief for as long as six months. A multicenter, randomized, double-blind, sham-controlled trial of knee osteoarthritis produced results showing that Iovera reduced pain at significantly greater levels than patients in the sham group at 30, 60, and 90 days post-treatment (Radnovich et al. 2017). Iovera is indicated in patients with osteoarthritic pain and plays a similar role in pain prevention for total knee arthroplasties. Landmarks for the Iovera procedure are shown in Figure 1.
Exparel (Liposomal Bupivacaine)
Exparel is a local anesthetic (Bupivacaine) encapsulated in liposomes. It is injected locally at the surgical site or used with regional nerve blocks. After Exparel injection, particles gradually release Bupivacaine over time, as the lipid membranes are absorbed, prolonging the duration of action of Bupivacaine. This creates regional or targeted analgesia and blocks a significant amount of postoperative pain. Pain relief can be seen for 24 to 72 hours.
Anjeso
Intravenous Anjeso (meloxicam) is a safe and effective nonsteroidal anti-inflammatory drug. Anjeso studies following boney operations showed 31% less pain in patients who were administered two doses of Anjeso over 48 hours compared to patients who received a placebo (Hamblin 2017). We routinely prescribe meloxicam for pain management as an opioid-alternative to patients for which it is indicated. It is an effective anti-inflammatory that works well for pain management intraoperatively as well.
MLS-M8 Class IV Laser Therapy
MLS-M8 Class IV robotic laser sends pulsed light of wavelengths 808 and 905nm over the zone of pain. The laser penetrates 5cm beneath the skin to excite the cells and act as a powerful anti-inflammatory modality that generates a rapid healing response to the affected tissues. Some of the well-established biological effects include enzymatic activation, increased ATP production, alteration of the pain perception threshold, increase in circulation and vascular inflow, as well as nerve regeneration (Gottlieb et al. 2018). A photobiomodulation therapy study that used laser light energy with similar properties to the MLS-M8 laser showed that laser therapy is effective in significantly decreasing pain intensity and post-surgical inflammation in patients following total hip arthroplasty (Nesioonpour et al. 2014). MLS-M8 lasers do not generate significant heat energy and there are no known associated side effects. It is thus a great tool for postoperative pain relief and healing.
Regional blocks
Ultrasound-Guided Interscalene Block
This block is typically performed preoperative by a skilled anesthesiologist utilizing ultrasound guidance. Typically, patients will see 24-hour motor blockade, 36-hour sensory blockade, and up to five days analgesia pain relief.
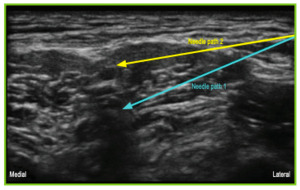
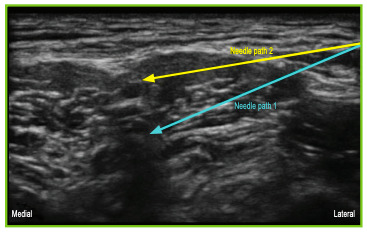
IPACK Block
IPACK (infiltration between popliteal artery and capsule of the knee) is a recent technique that involves the use of an ultrasound-guided local anesthetic infiltration of the interspace between popliteal artery and the capsule of posterior knee. IPACK has proven to be effective at inducing analgesia to the posterior knee without affecting motor nerves. IPACK can also be used as a supplement to other blocks such as adductor canal blocks for compounding analgesic effects (Thobhani, Scalercio, Elliott, et al. 2017). For total knee arthroplasties, we use either IPACK/adductor blocks or a local infiltration of Exparel.
Adductor Block
Adductor canal blocks target the saphenous nerve to generate analgesia to the medial leg and foot. Visualization via ultrasound enables the spread of local anesthetic adjacent to the femoral artery, branching into the muscle adjacent to the saphenous vein. The comparative benefit of this technique is that there is no motor blockade; patients maintain control of important quadricep function of their leg.
Surgical Site Local Infiltration Techniques
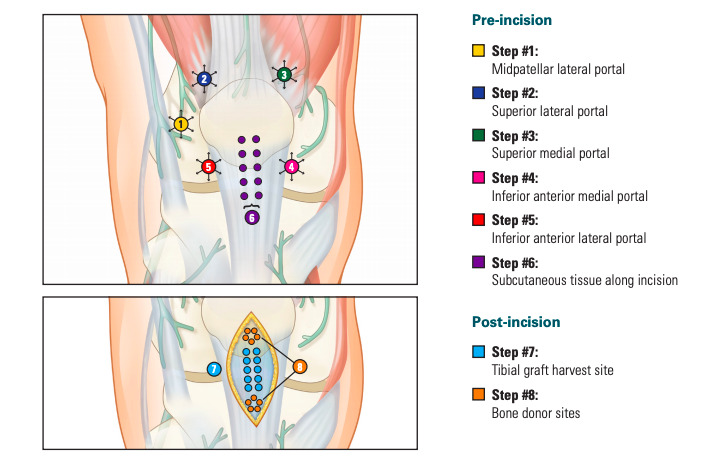
Bone-Patellar-Bone ACL Reconstruction
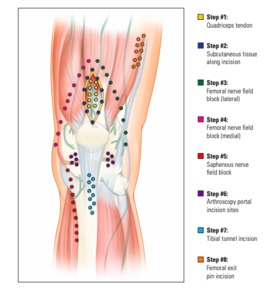
This infiltrative technique consists of 20cc Exparel, 20cc 0.25% Marcaine, and 40cc saline mixture. 10cc syringes are used in an eight-step process as outlined in Figure 4.
Quadricep Tendon ACL Reconstruction
This infiltrative technique consists of 20cc Exparel, 20cc 0.25% Marcaine, and 40cc saline mixture. 10cc syringes are used in an eight-step process as outlined in Figure 5.
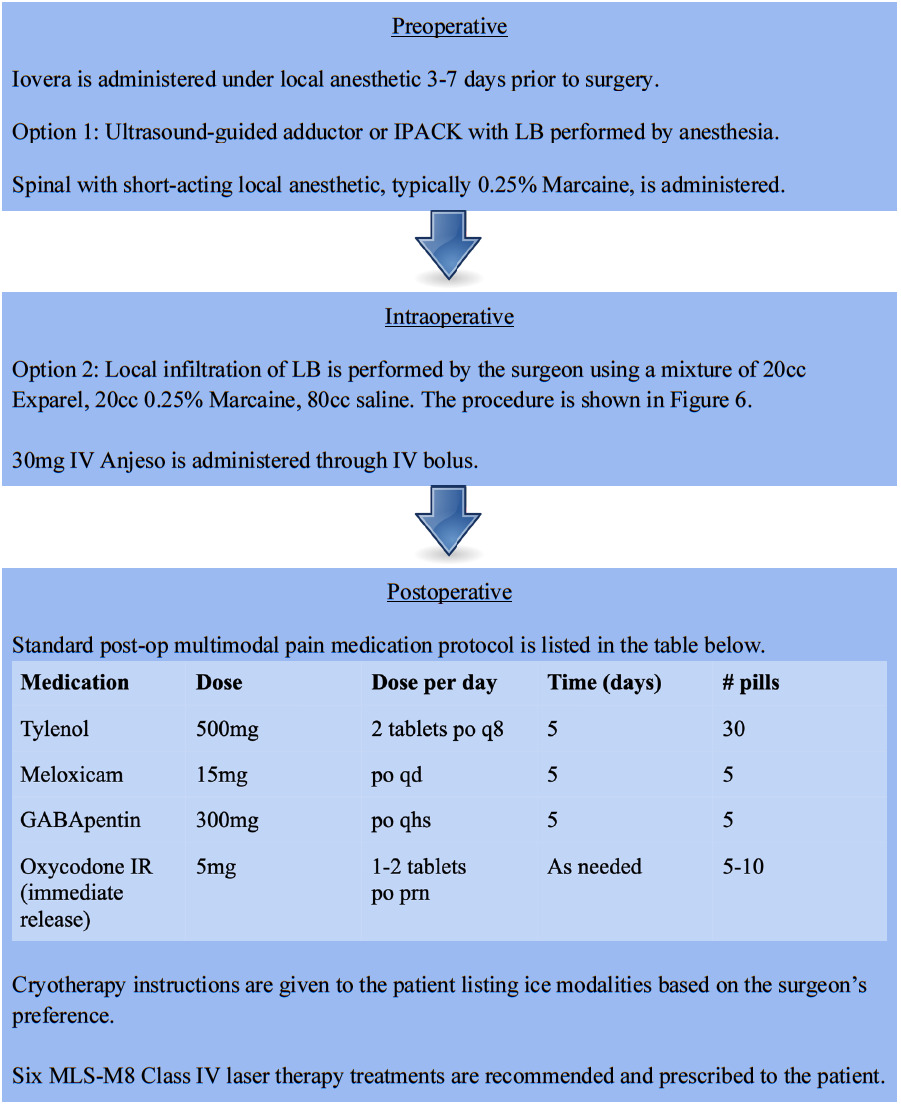
Total Knee Arthroplasty
This local infiltration technique utilizes a 20cc Exparel, 20cc 0.25% Marcaine, and 80cc saline mixture. 10cc syringes are used in a six-step process as outlined in Figure 6.
Comprehensive Perioperative Surgical Protocols
ACL Reconstruction
Total Knee Arthroplasty
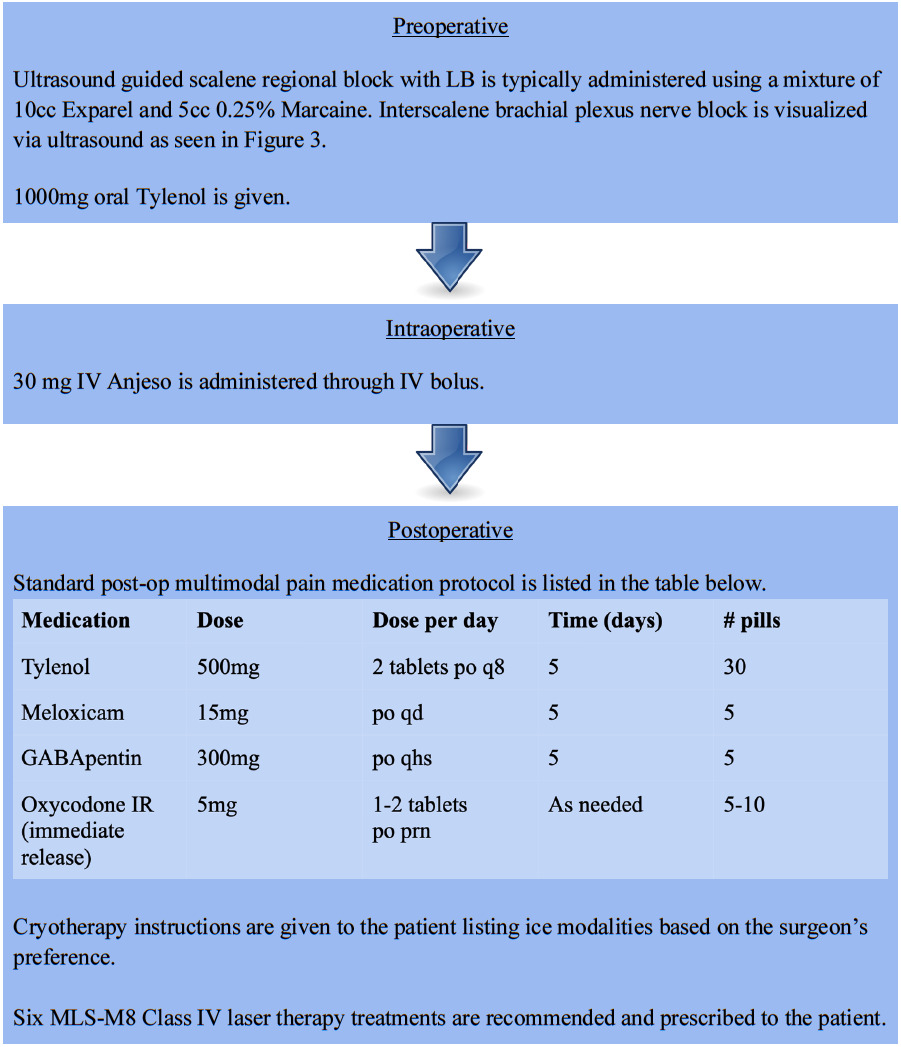
Upper Extremity Surgery
Discussion
A multi-modal approach to pain management can significantly reduce the need for highly addictive opioids. An opioid-sparing strategy for orthopedic surgery, and medicine at large, is possible with the right combination of tools and does not have to come at the expense of the patient experience. Reducing opioid exposure during the perioperative period should be a priority. The studies mentioned in this article has proven the effectiveness of pain reduction modalities such as Exparel, Anjeso, regional blocks such as IPACK and adductor canal block, and MLS-M8 laser. The argument is that opioid alternatives are more expensive than traditional opioid pain management. Additional studies are indicated to assess the long-term outcomes of patients treated with opioid-sparing techniques in order to prove a reduction in overall cost to the healthcare system. Further evidence-based research for opioid-sparing protocols is indicated.