Introduction
As the coronavirus 2019 (COVID-19) pandemic continues across the United States, the influx of patients affected by the virus has created economic, social, and physical strains on healthcare systems. New York was one of the earliest states drastically affected by COVID-19, and New York City quickly became the epicenter of the crisis in early March 2020 as cases began to rise exponentially. A wartime mentality was initiated by multiple health systems in the greater New York City region in response to the coronavirus outbreak (Konda et al. 2020; Schwarzkopf et al. 2020; Mo et al. 2020; Richardson et al. 2020). Healthcare professionals were redeployed to COVID-specialized units, research efforts and funding was diverted toward understanding the disease, and personal protective equipment (PPE) was prioritized for healthcare workers with direct exposure to infected patients.
One of the earlier efforts by hospital systems was the establishment of a prone positioning protocol for intubated patients with acute respiratory distress syndrome (ARDS). At Lenox Hill Hospital, the Department of Orthopaedic Surgery was repurposed from the Operating Room (OR) to the Intensive Care Unit (ICU) and formed prone positioning teams with physical therapists and intensivists. Constant multi-disciplinary collaboration was utilized to develop a standardized prone positioning protocol with a focus on maximizing efficiency and patient safety (Rahman et al., n.d.). This initiative originated from research from the PROSEVA study group suggesting a decreased 30-day mortality for intubated patients with ARDS who were routinely placed in the prone position to improve aeration (Guérin et al. 2013). While in the ICU, a team of orthopaedic surgeons recognized the need to optimize medical equipment to ensure that bony prominences on the face, shoulders, and chest were appropriately padded while maintaining safe access to the airway and endotracheal tube. With input from wound care specialists and critical care physicians, our team collaborated with a medical device company and designed a patient positioning tool to efficiently and safely position these patients.
The Problem
Orthopaedic surgeons are well-experienced in positioning patients prone in the OR in order to optimize surgical approach. Placing an intubated patient in the prone position has a complication profile that includes vision loss, neurologic injury, and the development of decubitus ulcers overlying bony prominences, and therefore the benefits of this type of positioning must outweigh the risks. To that end, orthopaedic surgeons are hypervigilant on patient safety in the operating room. There are multiple issues that can occur when a patient is placed in the prone position, which has been extensively studied in spine literature for patients undergoing posterior lumbar and cervical procedures. While the management of endotracheal tube placement is generally handled by anesthesia team, head and neck positioning is primarily handled by the operative team. Iatrogenic injuries can occur in the prone position. A systematic review examining postoperative complications in prone positioned patients found vision loss as the most commonly reported complication at an average of 3.09 per 10,000 spinal fusion procedures (Shriver et al. 2015; Shen, Drum, and Roth 2009; Warner et al. 2001). There is also an increased risk of injury to the brachial plexus and cervical spine due to focal pressure points or improper neck flexion and extension (Kwee, Ho, and Rozen 2015; Akhavan, Gainsburg, and Stock 2010; Mobley et al. 2007).
Ulcers from pressure dependent areas can also occur postoperatively, with stage 1 pressure ulcers rates ranging from 5 to 66% (Grisell and Place 2008; Koreckij, Price, and Schwend 2011). One study found increased BMI, male gender, and increased age as significant covariates in the development pressure ulcers in the ICU (Girard et al. 2014). If proper padding is not placed on the thorax and abdomen in the prone position, there can be an acute increase in intra-abdominal pressure. An increase in intra-abdominal pressure greater than 12 mmHg has been shown to place patients at risk for the development of abdominal compartment syndrome (Shih et al. 2011). Facial edema can also occur in the prone position with increased risk in longer duration procedures and with increased volume resuscitation efforts. Facial pressure in the prone position has been reported to be an average of 30 mmHg and as high as 50 mmHg at the chin and forehead (Leibovitch et al. 2006).
These studies demonstrate a clear positive correlation between increased operative time in the prone position and an increase in complications related to surgical positioning. In the ICU, intubated patients were placed in the prone position between 16 to 18 hours, multiple magnitudes longer than operative times recorded in the spine literature. Therefore, intubated COVID-19 patients placed in the prone position for an extended amount of time were at high risk of developing these complications.
Developing a Solution
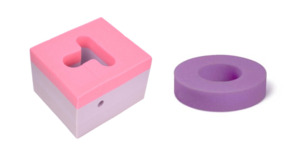
Current practices for facial protection in the prone position are limited to either a pillow or a disposable foam head doughnut (Figure 1). As documented by our experiences in the ICU, these levels of support provided minimal cushioning and support and led to the development of pressure ulcers. Unfortunately, during the pandemic, complications related to insufficient padding of bony prominences occurred, as higher priority and focus was given to more emergent maladies that affect the multisystem organ failure patient. Although the hospital staff is inundated with more emergent tasks affecting the COVID-19 patient, care should not be taken away from patient safety. Ulcerations on the face, nose, or lips can have serious long term consequences such as infection, tissue necrosis, and the development of skin cancer. Decreased quality of life due to chronic skin and wound breakdown can be severely detrimental both physically and psychologically to the patient. However, with careful attention to detail and the use of the optimal equipment, many of these complications can be avoided.
After recognizing this problem and discussing potential solutions with the intensivist team, we began to brainstorm a patient positioning tool that could address the problems observed. We discovered that the ICU physicians and nurses did not know the optimal way to address this issue since intubated patients in the ICU are not typically placed in the prone position for an extended time. Existing products from the operating room used by anesthesiologists such as disposable foam head doughnut and pillows were designed for OR tables and not for standard hospital or ICU beds (Figure 2). We found that these foam supports placed the neck in excessive extension and required the use of multiple pillows in the chest and shoulder area to allow the neck to achieve more flexion. Overall, our original padding method, although effective, was clumsy and resulted in too much variability in providing safe padding.
One of our first attempted solutions was to use prone massage mattresses for pregnant women that had been graciously donated to our institution (Figure 3). However, we found that the mattress to be too firm, and the mattress edges caused an unacceptable rate of facial pressure ulcers and bruising. In addition, the leather material was difficult to clean and thus precluded the use of the mattresses for additional patients. Lastly, the mattresses were too costly to be single-use and disposable. In order to mitigate cross-contamination between patients and providers, we concluded that a prone support should be ideally made of foam, single-use, disposable, and cost-effective.
Learning from our previous failures and shortcomings of available products, we sought to develop a single foam support that could safely and efficiently protect the face and upper torso while maintaining a neutral cervical spine position and safe airway and endotracheal tube access. Furthermore, this support would be optimized for use on a hospital or ICU bed. We discussed the problem of compromised patient safety in prone positioned patients with a medical device company that develops orthopaedic positioning tools for use in the OR. Our design efforts led to the development a prone positioning tool (Prone Foam, Bone Foam Inc., Corcoran, MN) for intubated patients affected by COVID-19 (Figure 4) (Bone Foam, n.d.).
We tested out this hypothesis by utilizing a prototype on intubated patients in the ICU. After multiple uses, it was apparent what aspects of the design provided protective padding for the patient and what areas may potentially impede on rapid airway access (Figure 5). A key principal in effective prone positioning was to increase the height of the chest padding relative to the facial padding to allow the neck to fall into a neutral flexion. However, there was still the need for sufficient facial padding to ensure that the nose, eyes, or lips did not contact the mattress underneath. Furthermore, after observing that successful utilization of the prone support was somewhat operator-dependent, it became evident that we needed to develop a prototype and method that would be easily teachable to the multidisciplinary ICU team and could be implemented in a timely manner. Finally, we developed removable chin and neck supports that could be personalized based on the patient’s body habitus. Outlined in Appendix 1 and Video 1 are the proper instructions on placing an intubated patient in the prone position using the Prone Foam.
After identifying patients that would benefit in the ICU, we further validated the prototype on awake patients. During the COVID-19 pandemic, even awake patients in respiratory distress were placed in the prone position for up to 8 hours. Recent studies suggested that prone positioning may improve oxygen saturation in awake patients in respiratory distress with the goal of avoiding or at least delaying early intubation, which is associated with increased mortality (Caputo, Strayer, and Levitan 2020; Jiang et al. 2020). We discovered that these patients experienced significant discomfort laying prone for multiple hours using either a pillow or foam head doughnut. After trialing the prototype, patients reported that the foam device felt comfortable and made the prone position more tolerable. While existing devices are available for patients in the prone position, such as a specialized kinetic beds (RotaProne, Arjo Inc., Addison, IL) or proning mattresses (Prone2Help Inc., New York, NY), these may be costly to health systems and not readily accessible during a pandemic (Kim and Mullins 2016). Our hope is the prone positioning device can be rapidly distributed to health systems in need during the COVID-19 pandemic and have the ability to be stored and reused for potential future viral outbreaks.
Conclusions
The process of designing a patient positioning device was challenging and many lessons were learned along the way. As medical professionals on the front lines during the pandemic, we were positioned to deeply understand the day-to-day problems in the care of the prone-positioned, intubated patient. We saw the gradual development of ulcers on our patients even with proper positioning and support of at-risk regions. Available devices in the ICU did not adequately support these patients and we realized a simple but effective positioning device was needed. This entrepreneurial and multi-disciplinary endeavor was resident-physician driven and validated by not only the intensivist staff but also awake patients in the prone position. These efforts reflect the concept of ‘intrapreneurship’ in that novel ideas can start within health systems and that innovation can start at any level (Tomas 2020). Resident physicians spend many hours in the hospital interacting with patients and providers from multiple disciplines. There are certainly difficulties encountered in patient workflow at every level of care. Instead of getting frustrated by inefficiencies that may impede workflow, it may be valuable to reflect on these experiences as potential problems that can be resolved (Campbell et al. 2018). Writing a brief note on difficulties encountered can allow for reflection at a later time to understand the root cause of the problem. These thoughts can later be developed into a potential solution that can enhance clinical outcomes or improve inefficient workflow (Maher et al. 2019).
Another lesson learned was the concept of bridging of silos. Ideas from other industries, or in this case the orthopaedic surgery subspecialty, can be transferred to other arenas in order to benefit patients. Although orthopaedic surgery is a highly specialized and technical surgical subspecialty, it is important to have an acute awareness of best practices embraced in other medical specialties as well as other industries all together. We discovered that the ICU was facing difficulties and were able to apply best practices in surgical positioning to the intubated and prone positioned ICU patient. In an article in Harvard Business Review, Poetz et al. discuss that collaborating with individuals from analogous fields can be a source of radical innovation (Poetz, Franke, and Schreier 2017). Thought leaders in other specialties or industries are not bogged down by the intricate details of a specialized field and provide a fresh perspective on novel solutions that work for similar problems in their respective field. Bridging of domains can be bidirectional and by embracing this practice, the orthopaedic surgeon can develop novel and innovative concepts to their field of expertise.
In the midst of a pandemic, our team demonstrated resilience in developing an effective solution that was out of the normal scope of practice for an orthopaedic surgeon. We were able to take best practices utilized in the operating room and apply them to intubated and prone positioned patients with ARDS. Due to early efforts to contain the spread of the virus, the number of new cases in New York City stabilized in late Summer 2020. However with continued outbreaks in recent months, there is another resurgence of infections and high risk of further spread. Therefore it is prudent to remain steadfast and prepared for all situations. We hope that our efforts demonstrate that even in the face of adversity, there is an opportunity for us as medical professionals to think creatively and develop effective solutions that can help improve care to our patients.