Introduction
Meniscus tears are one of the most common sports related knee injuries reported in the adolescent population, usually occurring in the setting of acute trauma during organized sports (Mosich et al. 2018). Bucket handle meniscal tears are commonly encountered in the adult population, yet infrequently present in the pediatric and adolescent populations. Most bucket handle meniscal tears in younger patients occur in males during sports and affect the medial meniscus (Kramer et al. 2019). Bucket-handle tears tend to occur more frequently in normal menisci than in abnormal menisci throughout the literature (Schlossberg et al. 2007).
Isolated meniscal injuries are uncommon in children under the age of fourteen. These injuries are typically associated with congenital meniscal abnormalities including discoid meniscus morphology (Andrish 1996; Yalcin et al. 2009). The discoid lateral meniscus is one of the most common abnormal meniscal variants in children, estimated to have an incidence of 1 to 3% in the pediatric population (Kushare, Klingele, and Samora 2015; Hart et al. 2008). The incidence of bilateral lateral discoid meniscus is up to 20% of the cases, whereas bilateral medial involvement is rare (Dickason et al. 1982).
The first theory for the etiology of discoid meniscus was developed by Smillie in 1948 which postulated that the discoid shape is a normal stage in the developing embryo and that failure of absorption of the central portion will persist during the fetal state (“congenital discoid meniscus”; Smillie 1948). This theory was later refuted because neither human nor animal embryological specimens demonstrated such a stage during normal development (Clark and Ogden 1983; Kaplan 1955). The “congenital” theory, which is supported by case reports of the occurrence of the condition in twins and descriptions of familial transmission, considers the discoid meniscus as an anatomical variant and suggests that increased shear stress causes meniscocapsular separation and secondary hypermobility (Gebhardt and Rosenthal 1979; Dashefsky 1971).
Discoid meniscus occurs more commonly in Asian populations, with incidences as high as 13-16% (Lucas et al. 2015; Fukuta, Masaki, and Korai 2002; Sun and Jiang 2011). The abnormal shape and increased tissue thickness predispose these discoid menisci to injury and tears (Kushare, Klingele, and Samora 2015). Arthroscopic treatment for bucket handle tears and torn discoid menisci should be offered for symptomatic patients. Treatment can consist of saucerization, partial meniscectomy, and/or meniscus repair. Arthroscopic repair of torn discoid lateral meniscus in children has been shown to have favorable clinical outcomes in short and long-term follow up, with range of motion restored and significant improvement on patient reported outcome scores (Koga et al. 2016; Okazaki et al. 2006; Yoo et al. 2015; Lee et al. 2017).
Our case report is the only reported isolated bucket handle discoid lateral meniscus tear in a child less than ten years old to undergo meniscal repair. Furthermore, it is the second reported isolated bucket handle lateral meniscus tear in a child less than ten years old (Yalcin et al. 2009). Limited case reports, seven, exist detailing bucket handle meniscus tears in patients less than ten years old. The youngest reported bucket handle tears in the literature involved two and four-year-old patients. These both involved the medial meniscus (Nooh et al. 2016; Fink et al. 2018; Bloome et al. 2000; Saddawi and Hoffman 1970). Another case report detailed a bucket handle tear of a lateral meniscus in a six-year-old girl treated with a subtotal meniscectomy. This is the only previously reported case report, to our knowledge, of an isolated bucket handle discoid lateral meniscus tear in a child less than ten years old (Yalcin et al. 2009; Nooh et al. 2016). Our case details the presentation, treatment, and recovery of a seven-year-old female who presented with an isolated bucket handle tear of a discoid lateral meniscus.
Case Description
A seven-year-old Hispanic female, with no past medical history, presented to our clinic with left knee pain and progressive limp which developed over the previous two months. The patient denied any falls, inciting trauma, or any illness surrounding the onset of her symptoms. The patient did not remember how she initially hurt her knee. The patient’s mother reported the possibility of an unwitnessed fall while at school. The patient reported waking up with pain in the back of her knee which progressed over the next two months. The pain was also noted to keep her up at night.
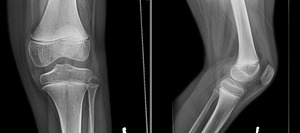
Physical examination of the patient’s left knee demonstrated passive range of motion that was 5 degrees shy of full extension with flexion to 130 degrees. She was 121 centimeters (3 feet 11 inches) tall and weighed 34 kilograms (74.8 lbs) with a BMI of 23.2. Her ligamentous knee exam was noted to be stable. She had tenderness over the lateral joint line and a sense fullness reported on the posterior aspect of her knee. Initial radiographs performed demonstrated normal anatomic alignment and did not reveal any bony hip or knee pathology (Figure 1).
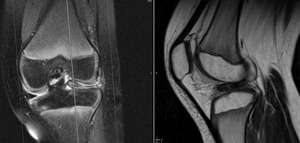
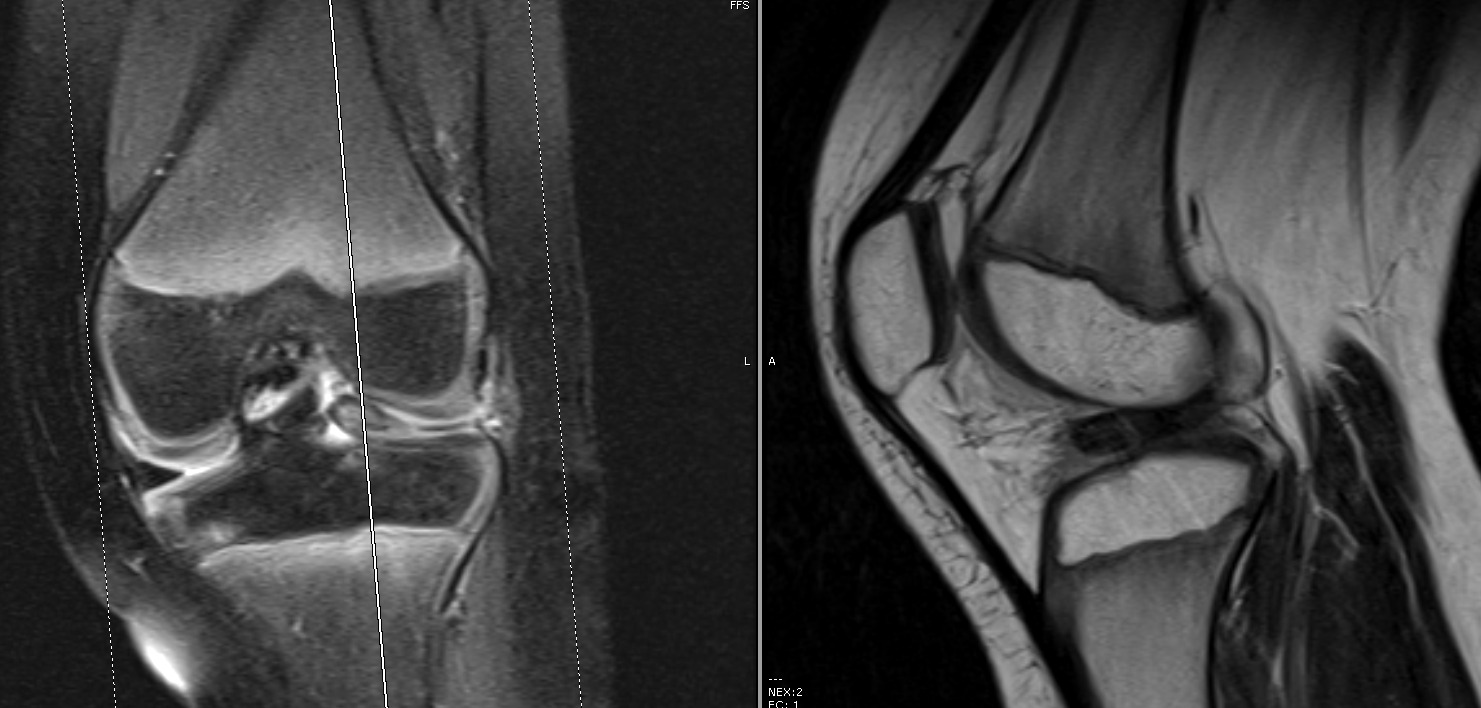
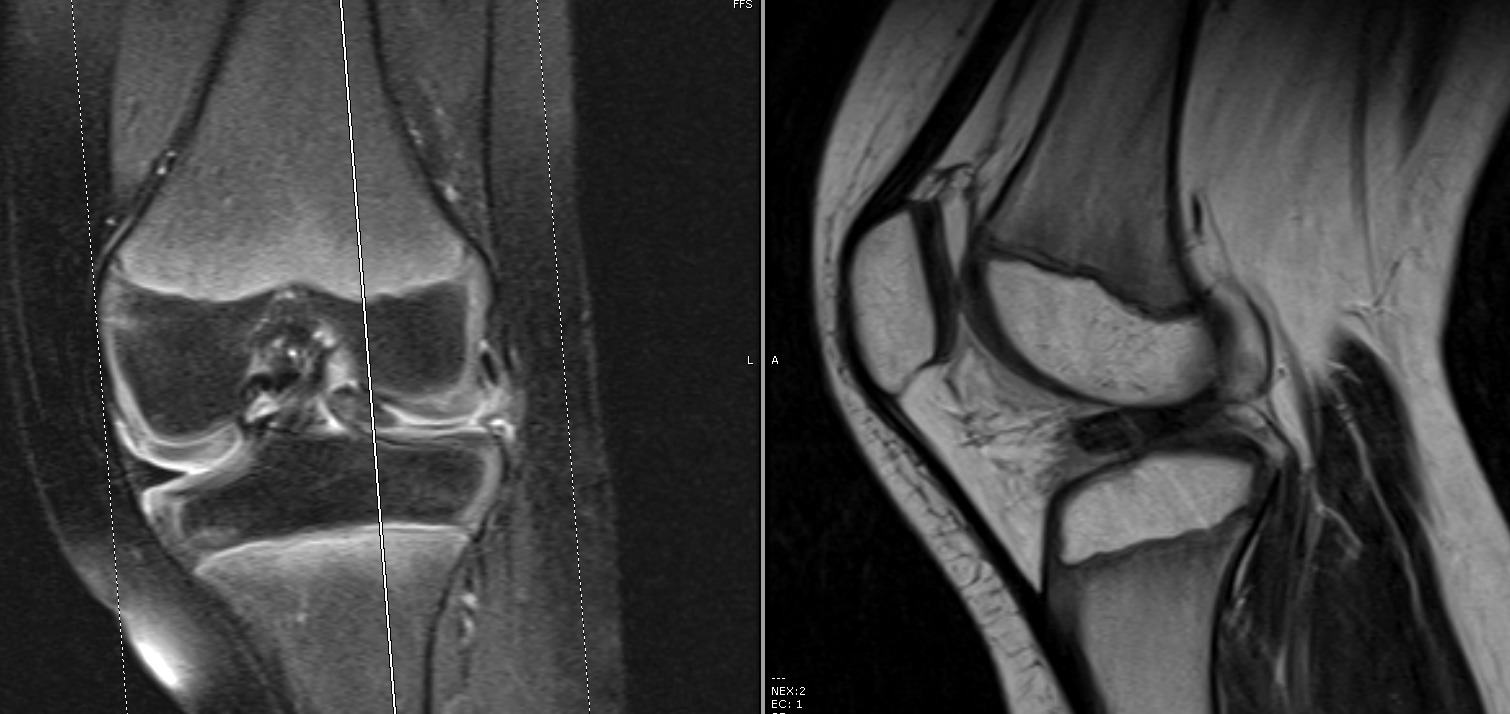
A MRI of the knee revealed a displaced tear of the anterior and posterior horns of the lateral meniscus (Figures 2 & 3).
The patient was evaluated in the orthopaedic pediatric and sports medicine clinics. Risser staging was not assessed. She was Tanner Stage I at time of presentation. There was no obvious discrepancy between her biologic and radiographic ages. The decision was made to proceed with surgical management of her bucket handle lateral meniscus tear utilizing diagnostic arthroscopy and lateral meniscus repair.
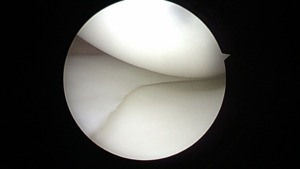
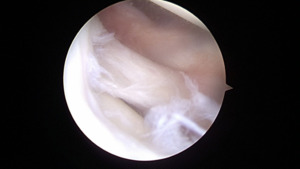
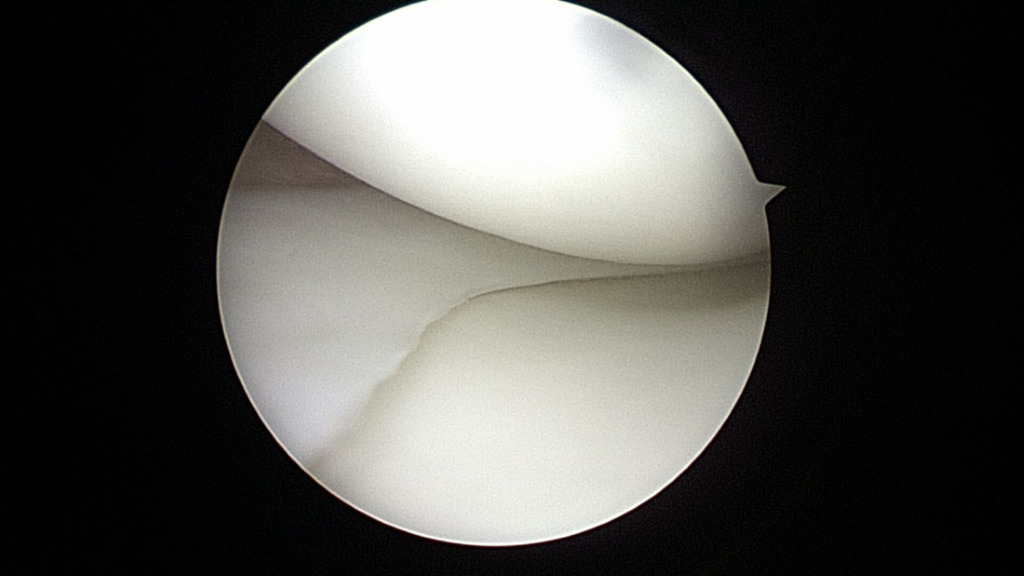
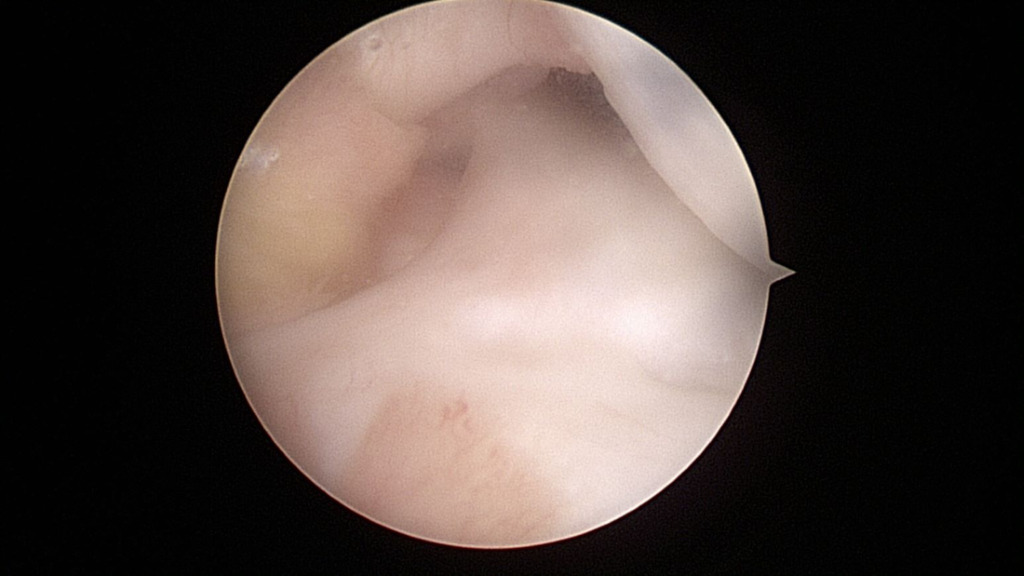
At the time of surgery, diagnostic arthroscopy revealed intact cartilage without any defects or abnormal wear. There was no evidence of a ligamentous injury. The medial meniscus was found to be intact (Figure 4).
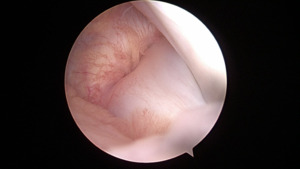
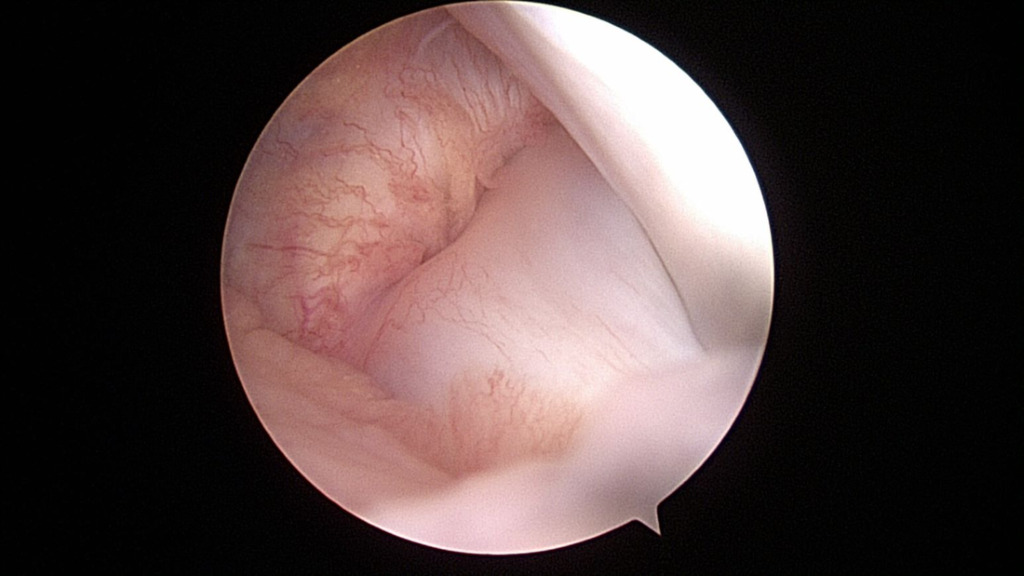
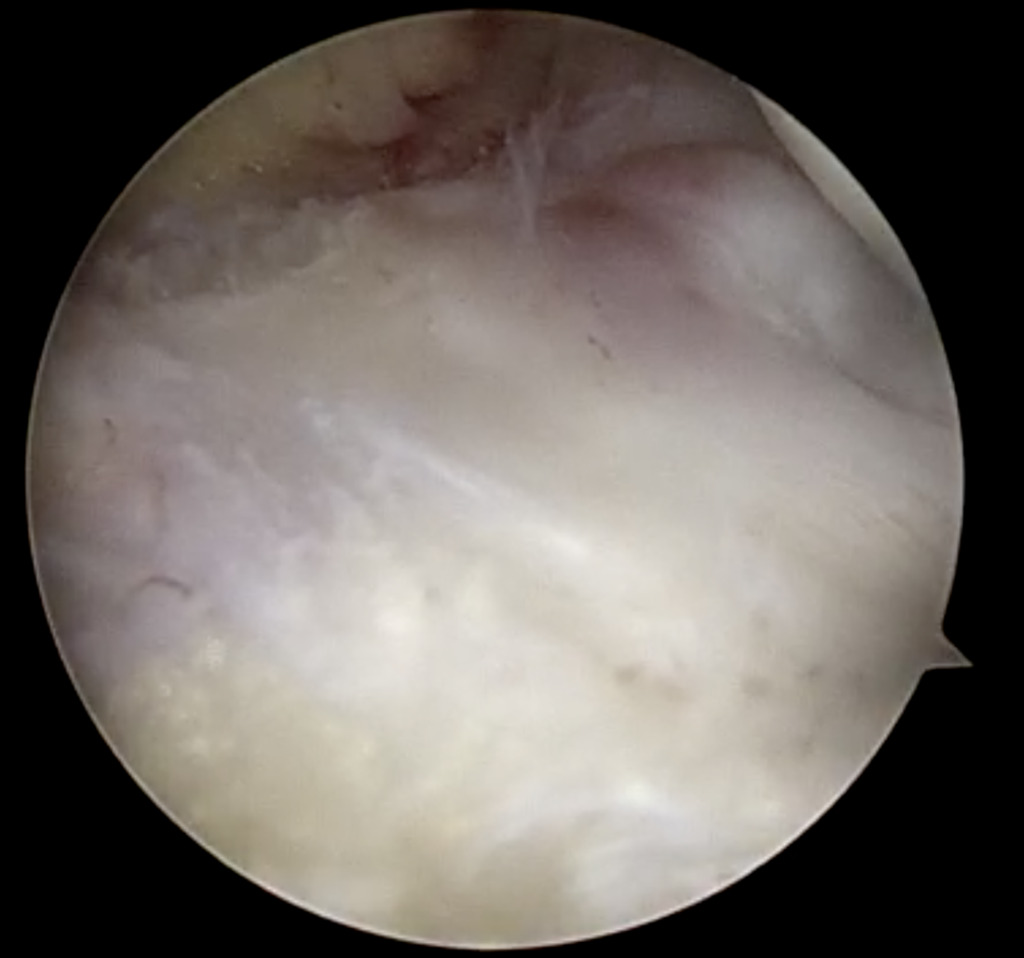
The ACL and PCL were intact. The lateral compartment revealed a lateral meniscus tear with the tissue displaced centrally into the notch, impinging on the ACL (Figure 5).
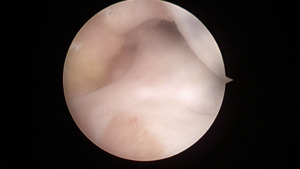
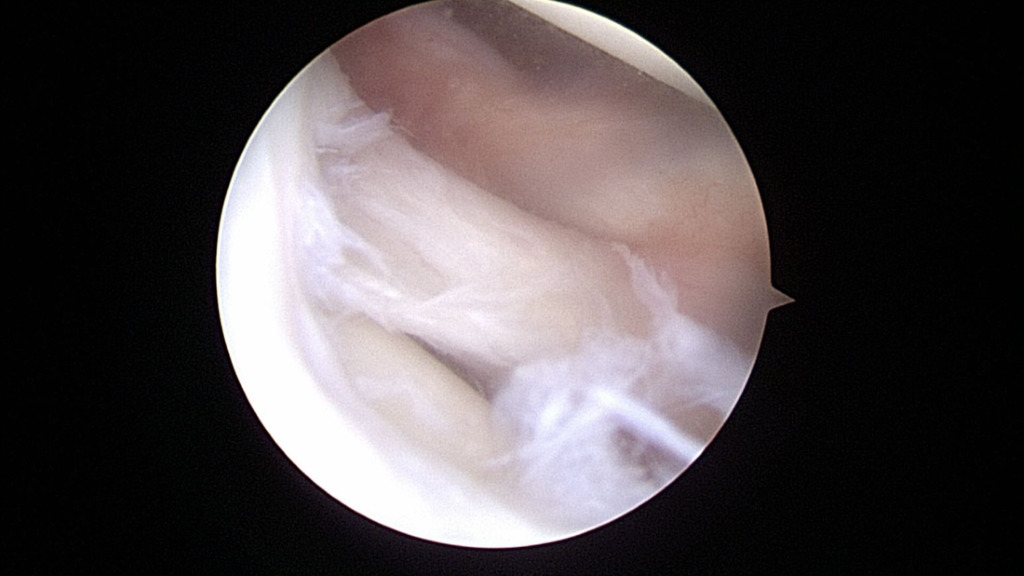
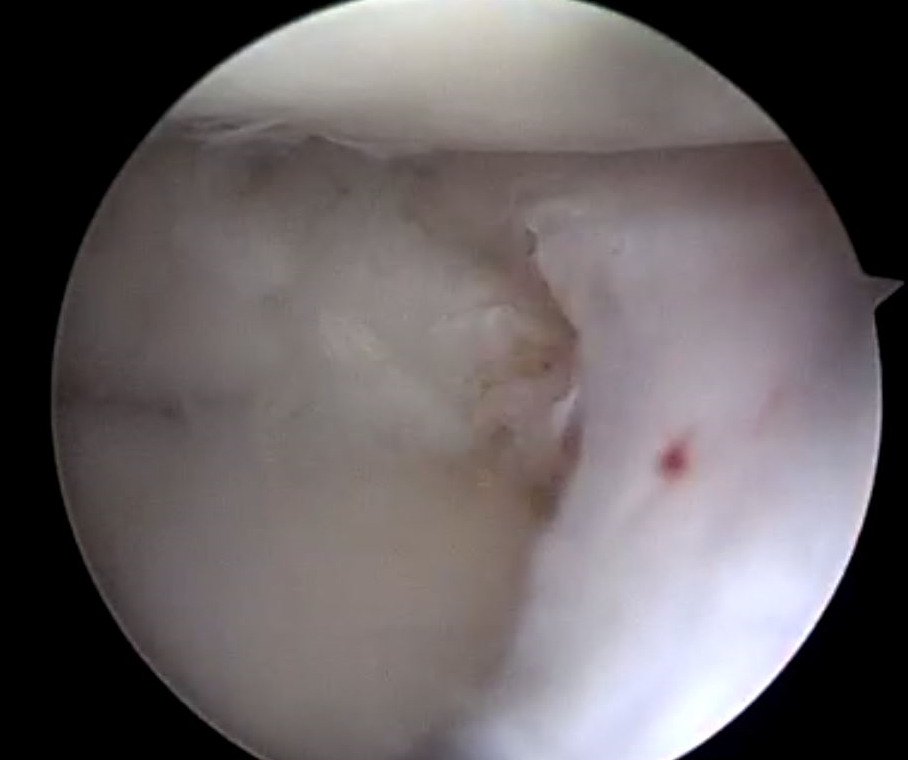
The tear pattern involved the periphery of the lateral meniscus, extending along the meniscocapsular junction from zones I though III (Figure 6).
The anterior and posterior roots of the lateral meniscus were intact (Figure 7).
The lateral meniscal tissue appeared hypertrophied and was noted to be a Wrisberg-type discoid variant (Figure 8).
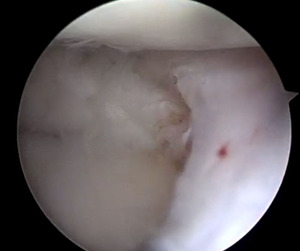
Saucerization of the redundant lateral meniscal tissue aided in the reduction of the displaced meniscus (Figure 9).
Gentle abrasion of the capsule was performed to establish a biologically favorable environment for healing. A #2 Fiberwire (Arthrex, Naples, FL) suture was passed through the periphery of the lateral meniscus at the zone II/III junction in an outside-in manner to act as a traction suture and aid with reduction. Two all-inside suture passing devices (Mitek Truespan, Raynham, MA) were used in Zone III to stabilize the posterior horn. Additional Fiberwire (Arthrex, Naples, FL) sutures were passed through Zones I & II in outside-in fashion to create horizontal and vertical mattress configurations, stabilizing the anterior horn and mid-body of the lateral meniscus. This was repeated until stable fixation was achieved throughout the meniscus. The sutures were tensioned and tied with the knee in extension. The meniscus reduced well and was found to be stable after repair (Figures 10 & 11).
After fixation, the knee demonstrated full range of motion. Once the procedure was complete, the patient was placed in a long leg cast in slight flexion to ensure adherence to non-weight bearing status.
The patient was seen at her two, four, six, and twelve-week follow-up appointments. She progressed without incident through her post-operative period. She reported no pain and no issues with cast/non-weight-bearing instructions at six-week post-operative follow-up. The patient’s wounds healed well. The patient’s knee range of motion after cast removal at six weeks was noted to be 30-90 degrees. The patient began progressive weight-bearing without assistive devices at the six-week post-operative mark. She participated in a home exercise program and formal physical therapy sessions working on her knee range of motion. She presented at twelve weeks postoperatively with neither pain nor any feelings of catching. She was full weight-bearing without assistive devices and had returned to activity without pain. At four months post-operatively she demonstrated full active and passive range of motion. She was jumping rope and resumed full activity without restrictions. She was seen at her six-month post-operative follow-up visit and continued to have full range of motion with no complaints. A phone visit follow up at 9 months post operatively was performed and she continued to have no pain or mechanical symptoms and was continuing with normal activity with full knee range of motion.
Discussion
Sparse reports exist of pediatric bucket-handle meniscal tears in patients under ten years old. Furthermore, within this cohort only one previous pediatric patient has been reported to have a bucket-handle tear of the lateral meniscus, but this was not a discoid variant. This case report details the only patient found to have a bucket handle tear of a discoid lateral meniscal variant.
Discoid meniscus morphology contributes to a predisposition for meniscal tears. Homogenous collagen fiber organization is lost within the discoid morphology, with the periphery of the discoid meniscus maintaining a typical uniform parallel fiber orientation and the central portion having a more random fiber orientation (Bisicchia, Botti, and Tudisco 2018; Atay et al. 2007; Kim, Han, and Lee 2016). This demarcation of tissue organization was appreciated arthroscopically and used to determine level of saucerization (Figure 10). The unique histological structure likely leads to inability to resist forces while dissipating hoop stresses within the knee joint, resulting in increased tear rates with minimal trauma.
Multiple studies have highlighted the deleterious effects of meniscectomy in the pediatric population. Examining outcomes reported in non-discoid literature, only 25% of patients that underwent meniscectomies continued to be asymptomatic after 5 years and 80% had radiographic evidence of osteoarthritis after this time. Furthermore, the rate of OA development in patients following meniscectomies for symptomatic discoid patients at eight-year follow-up was approximately 50% (Sabbag et al. 2019). Other deleterious effects after meniscectomy include decrease in range of motion, decreased hip abductor strength, and increased pain (Haskel et al. 2018; Sabbag et al. 2018; Vahvanen and Aalto 1979; Kocher, Logan, and Kramer 2017).
The recommendation regarding repair of meniscal tears in pediatric patients is rooted in previous literature that has supported the idea of fibrocartilage regeneration after meniscectomy in pediatric patients (Bisicchia, Botti, and Tudisco 2018; Han et al. 2018). Meniscus repair rate in the pediatric population is noted to be 53% with one study concluding that up to 75% of symptomatic discoid meniscus patients received surgical repair (Sabbag et al. 2019; Jackson et al. 2019). Based on the favorable outcomes reported, meniscus repair should be attempted in most meniscus tears in children (Yang, Liotta, and Paschos 2019). The clinical success rate of arthroscopic meniscal repair in patients 18 years old or younger has been reported to be 80% for simple tears, 68% for displaced bucket-handle tears. Risk factors for failure included complex tears and rim width greater than 3 mm (Krych et al. 2008).
Outcomes of meniscus repair after restricted weightbearing and early weightbearing have provided similar results (VanderHave, Perkins, and Le 2015; O’Donnell, Freedman, and Tjoumakaris 2017). Early weight bearing in extension has been thought to improve healing rates after meniscal repair by providing compression of the repaired tissue with axial load. There is also the idea that range of motion with axial load can cause sheer stress across the repair construct leading to decreased healing and increased failure rates. In our specific patient, there was some concern in her comprehension and adherence to touch down weight bearing in extension with an adjustable hinged knee brace due to her young age. Rather than risk early unprotected weight bearing compromising the repaired meniscal tissue, she was placed in a long leg cast with slight flexion to ensure adherence to non-weightbearing status.
A limitation of this study is the low level of evidence by this case report, but this is necessary given this inherently unique patient presentation and treatment. Future research should describe similar patient presentations and compare patient characteristics and difference in treatment methods. It could also evaluate long term outcomes in pediatric patients treated with meniscus repair versus meniscectomy. Another avenue of future research could involve optimal post-operative immobilization and weight bearing in the pediatric population after meniscal repair. This unique case report can aid in the diagnosis and treatment of young patients with discoid meniscus tears.
In conclusion, this is a unique case of a pediatric patient less than ten years old presenting with a bucket-handle tear of a discoid lateral meniscus. This case report details the saucerization, repair technique, and successful post-operative recovery of a rare injury pattern in a pediatric patient. Furthermore, it highlights a technique for bucket handle meniscus repair, in lieu of partial meniscectomy, which is of particular benefit to minimize future risk of cartilage breakdown in the pediatric population.