Introduction:
In the United States, healthcare reform has led to increased scrutiny regarding healthcare expenditures, which are projected to grow at a rate of 5.8% per year according to the Centers for Medicare and Medicaid (CMS 2015). Increased healthcare spending is escalating 1.3% faster than GDP (Ahmadi et al. 2018) with much of the hospital costs derived from the operating room (Weiss et al. 2016). Inefficiencies in our hospital system are so numerous that most surgeons will spend less than 50% of their OR day actually operating (Saha et al. 2009; Sultan and Charalambous 2012; Delaney, Davis, and Tamblyn 2010).
In response to this, hospital systems have looked to minimizing costs by implementing a variety of efficiency programs such as “Lean Six Sigma,” which was originally used in the automotive industry to reduce waste and cost while maintaining value (Ohno and Bodek 1988; Womack, Jones, and Roos 1990; Hines, Holweg, and Rich 2004). All aspects of healthcare spending should be reviewed, but the greatest impact in reducing healthcare related costs would be to focus attention into reducing operating room expenses.
Demand for Value:
Improved healthcare standards have led to an increased life expectancy and an expansion of the geriatric population (Maradit Kremers et al. 2015). This increased population has expanded the prevalence of advanced osteoarthritis and recent reports have projected elective joint replacement surgery to be the most common surgical procedure in the near future (Kurtz et al. 2009; Cram et al. 2012) with up to 7.4 million Americans living with a total knee replacement in 2030 (United States Census Bureau 2014).
With this expanding usage as mentioned above, maximizing value is increasingly important. Value is defined as an outcome achieved per given set of resources (Porter 2010), and this can be maximized by improving quality or decreasing costs. Several authors have documented how streamlined instrumentation reduces OR clutter, improves OR set up and turnaround time, and maximizes efficiency (Ngu 2010; Chin et al. 2014). This improved value has led to decreased cost associated with sterile processing of instruments and decreased storage space while having no adverse effect on clinical outcomes.
The first step in decreasing unnecessary costs and increasing efficiency is to analyze the instrumentation and trays utilized. Many surgeons have “just in case” instrumentation associated with surgical trays that is rarely, if ever, used. Across all specialties, up to 78% of instruments in a surgical tray go unutilized, adding to waste associated with sterilization costs, counting and processing (Stockert and Langerman 2014). Several European studies have outlined the comprehensive cost of sterilizing and packaging reusable instruments with estimates ranging from $0.59 - $11.52 (USD) per surgical instrument (Adler et al. 2005; Demoulin, Kesteloot, and Penninckx 1996; Prat et al. 2004).
Many authors have applied this “lean” methodology to spine surgery, and have reduced 70% of instruments in the sets (Farrokhi et al. 2013) achieving cost savings as high as $41,000 per surgeon per year in sterilization and processing fees (Lunardini et al. 2014). A similar “lean” methodology can easily be applied to knee replacement surgery, and with an expected 600% increase in total knee replacements, achieving improvements in efficiency could have a large positive impact on healthcare spending (Kurtz et al. 2007).
In a recent 2019 article, the authors reduced instrument tray counts from an average of 7.5 trays to 3 trays by removing rarely used instruments. This reduction led to an annual savings of $159,600 in sterilization costs and $99,000 from improved turnover times (Capra et al. 2019). A modern implant and instrumentation system built around efficiency can further advance these improvements.
Strive for Efficiency:
Most modern implant companies vary in the trays and instrumentation needed to perform the surgery with some needing up to 9 trays of instruments per case. A decrease in surgical trays allows for faster set up and turn around as well as decreased sterilization and storage costs. This added savings from reduced surgical trays comes with no detriment to the patient and if these benefits are extrapolated over a year in a high-volume practice, the returns in cost reduction are significant. This increased efficiency can reduce preparation time by 20 minutes per case (Tibesku et al. 2013a). Fewer instruments may lead to clinical benefits as well. If fewer instruments are opened and OR preparation time is reduced, instruments spend less time exposed, thereby reducing potential contamination and increasing patient safety (Dalstrom et al. 2008). In one study, five percent of broaches and reamers were found to be positive for microorganisms before the case started (Maathuis et al. 2005).
Efficiency Maximized:
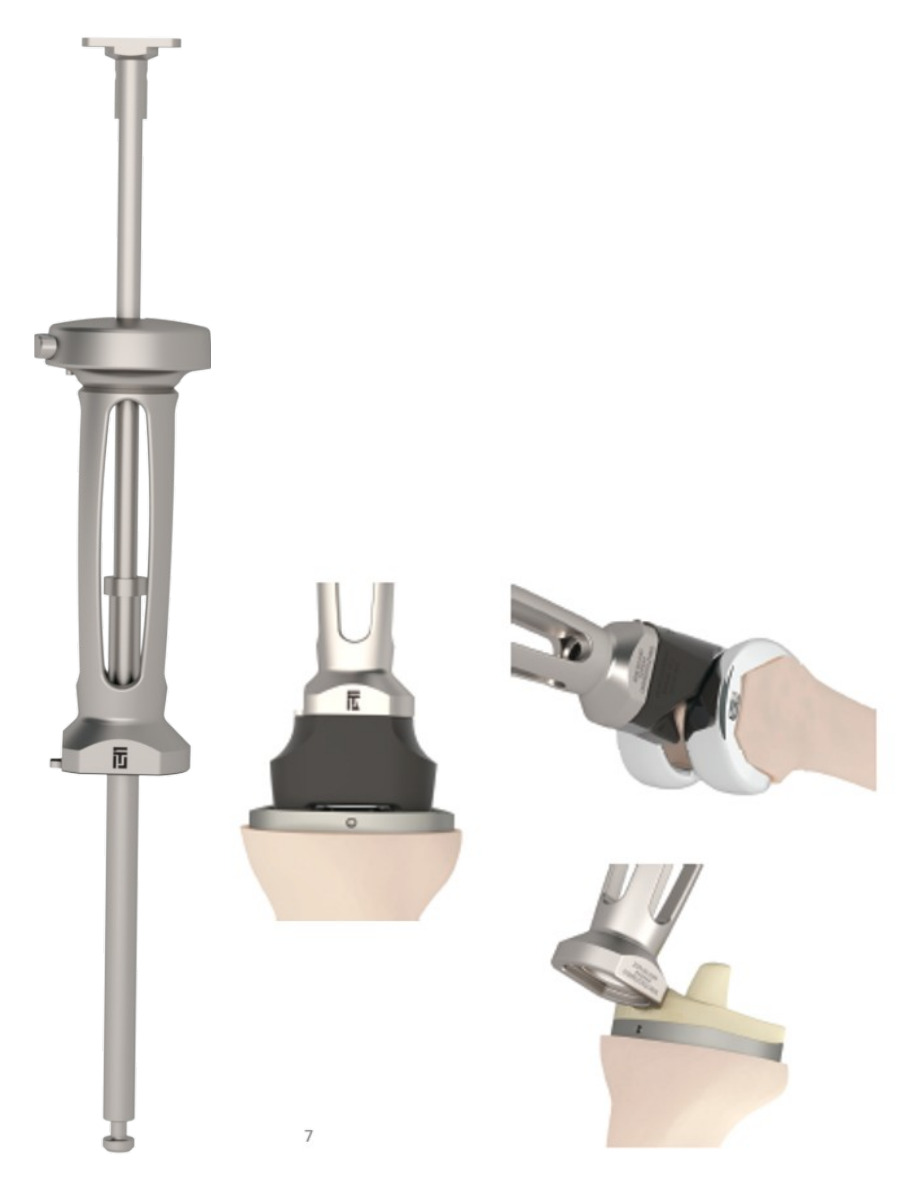
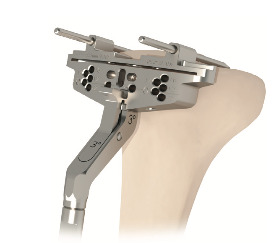
Currently, to the authors knowledge, the total knee system with the fewest number of trays is the Total Joint Orthopedics (TJO) Klassic® Knee System. This efficiently designed system offers symmetrical universal femoral and universal tibial components to accommodate both left and right knees in all shapes and sizes, minimizing inventory and instrument trays needed. Many of the instruments have multiple functions within the same knee procedure thereby allowing the instrument count to be reduced such that 90% of surgeries can be performed using a single, standard tray of instruments and 100% of cases can be performed with just two trays. (Figure 1 and Figure 2a-2c) Notice the distal femoral resection cut block is also used as a proximal tibial cut block thereby allowing it to be a “universal cut block.” Other areas of efficiency are noted in the outer handle of the slap hammer that doubles as the handle for the tibial and femoral impactor. By allowing instruments to serve multiple functions the instrument count can be reduced consolidating the knee procedure to a single tray in most cases.
Universal tibial implants are symmetrical and can be placed on either right or left proximal tibias. These implants have been well described and several authors have discussed the “pearls and pitfalls” of this prosthesis (Bozkurt et al. 2017; Martin et al. 2014). Outcome studies of the universal tibial component are numerous and demonstrate decreased inventory and instrumentation does not adversely affect outcomes (Maathuis et al. 2005). Some studies highlighted improved coverage, rotation and less risk for overstuffing using a symmetrical tibial implant (Maathuis et al. 2005; Mandalia et al. 2008; Bonnin et al. 2016). The Total Joint Orthopedics (TJO) modern tibial component accommodates both left and right proximal tibias by utilizing a “potbelly” design on the anterior arc to achieve excellent bone coverage.
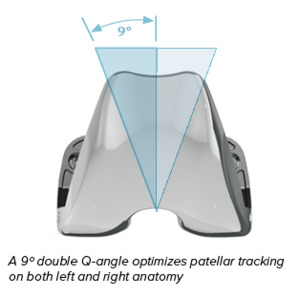
Universal femoral components are more heavily debated. The modern Total Joint Orthopedics (TJO) Klassic® Knee System utilizes a symmetrical universal femoral component and is different from the antiquated prosthetic designs. While some authors have claimed an asymmetrical (non-universal) trochlear groove improves patellar tracking, long term outcome studies; however, have failed to show a difference (Ashraf, Beard, and Newman 2003; Bindelglass and Dorr 1998; Worland et al. 2002). The Total Joint Orthopedics (TJO) Klassic® Knee System utilizes a deep trochlear groove and a patented Double Q-angle to optimize patellar tracking of the universal component in either a left or right femur. (Figure 3)
A recent knee kinematic study revealed near normal femoral rollback and axial rotation using this universal symmetric tibia and femoral implant system (Khasian et al. 2020), and outcome studies also demonstrate excellent knee society scores (Mangiapani et al. 2018). Recently published studies in 2020 demonstrated a combined knee society score improvement to 182 at final follow up, excellent knee ROM and low rates of manipulation under anesthesia using this universal knee system (Mangiapani et al. 2020; Crawford et al. 2020).
Other Efficiency Options:
There are other avenues to pursue efficiency, one of which involves “demand matching” with digital templating. This method involves templating the patient’s knee before surgery and these results are then used to fill two or three patient-specific trays with the templated size plus one size up or down to account for inaccuracies in the templating process. Demand matching studies find significant cost savings with some studies boasting a savings of $122 per surgical case through reduced central processing and turnover times (Hsu et al. 2012). This added efficiency allowed one additional surgical case to be added on each day.
Another efficiency option is the use of patient specific instrumentation (PSI). This option requires advanced imaging to custom make single use cutting guides specific to the patient’s anatomy. Studies looking at the benefit of PSI uniformly report reduced instrument tray count and faster room setup, but carries an increased cost due to the advanced imaging and manufacturing of the custom guides, plus increased waste and detrimental environmental impact from disposal of the single use guides (Capra et al. 2019; Sassoon et al. 2015). One such study analyzed the improved efficiency of the Smith and Nephew PSI guides. A standard Smith and Nephew primary TKA requires 6 surgical instrument trays but the PSI guides were able to reduce the amount of surgical equipment to 2 trays using patient matched instrumentation (Tibesku et al. 2013b). This decrease in the number of surgical trays used led to a cost savings to the hospital of almost $650 per case (Tibesku et al. 2013c). (Euro to USD conversion of 1.17)
Conclusion:
In a 2014 Harvard Business Review, Kaplan and Porter explained that hospitals often underestimate the costs of idle space and equipment. This miscalculation creates errors in utilization (Kaplan and Porter 2014). Using this Kaplan and Porter model of cost-reduction, optimizing efficiency through inventory is considered a significant opportunity to improve value. When extrapolated to TKA, the efficiency in inventory afforded by reducing trays allows a hospital to perform more procedures with the same amount of resources thereby improving overall value.
Most efficiency models that focus on minimizing instrumentation and tray count do so in two distinct ways. One of which is demand matching, this requires accurate preoperative templating and tray consolidation prior to each case. In this demand matched system, magnification errors may have detrimental effects due to lack of intraoperative equipment as a result of tray consolidation. In contrast the second option, patient specific instrumentation, is more efficient but has increased costs associated with advanced imaging and disposable single use guides which adds waste both economically and environmentally (Hsu et al. 2012). The benefits experienced in demand matched consolidation have prompted advances in total knee implants and instrumentation. By allowing instruments to serve multiple functions throughout the knee procedure (Figure 2a-2c) tray utilization is maximized while still giving the surgeon a full array of implant sizes. The modern Total Joint Orthopedics (TJO) Klassic® Knee System can provide a “demand matched” result through standard instrumentation, without going through the process of customization, thereby avoiding the possibility of human error and the cost associated with consolidating trays for every single case. By pursuing efficiency in the entire total knee design, considerable savings can be achieved while maintaining component function and options.
A modern, universal knee system designed from inception to maximize efficiency can achieve “demand matched” results, excellent clinical outcomes, and restore knee kinematics without detriment to the patient. Reduction in tray count has been shown to save approximately $250,000 in healthcare spending and decrease the environmental impact from single use disposable instrumentation and blue surgical wraps. Efficient knee systems, when properly designed, can reduce set up time, sterilization costs, storage space, and reduce sterile instrument surface area thereby decreasing exposure for contamination. A consistent, efficient tray system will help non-dedicated teams achieve “efficiency of familiarity.” This efficiency is needed in healthcare today and can be especially useful in smaller ambulatory surgery centers (ASC) where sterile processing and storage space is limited.
Acknowledgment:
I would like to thank Evan Carlson for his thoughtful comments and facilitation of this and prior drafts. I particularly appreciate his ideas, concepts and enthusiasm in completing this project.

_klassic_knee_system._this_universal_design_allows_instrumen.jpeg)


_klassic_knee_system._this_universal_design_allows_instrumen.jpeg)