Introduction
Tibia shaft fracture are common injuries. Approximately 500,000 occur in the Unites States each year (Russell 1996). Intramedullary nails are commonly used to repair tibia shaft fractures. Achieving limb length, alignment and rotation via appropriate fracture reduction is critical to optimize patient outcomes. There are multiple techniques to achieve reduction. Broadly, these can be classified as closed techniques, percutaneous technique and open techniques. Closed techniques have the advantage of not possibly damaging the local blood supply to the fracture site but it is not always possible to achieve and maintain this reduction, especially in certain clinical settings where a surgeon may be operating with minimal staff or assistants. One report (Auston et al. 2017) found that wound complications, deep infection and nonunion rates were similar regardless of type of reduction technique used at a level 1 trauma center. Similar outcomes were found in only one other paper from a level 1 trauma center (Tang et al. 2006). From this data it is possible to hypothesize that open
reduction does not have a significant negative effect on the outcomes of
operatively treated tibia shaft fractures in terms of wound complications,
deep infection and nonunion.
The purpose of this paper is to report the wound complications, deep infection and nonunion rates for a group of tibia shaft fractures treated with intramedullary nails with open reduction with bone reduction forceps treated by a single fellowship trained orthopaedic trauma surgeon at a Level 3 trauma center.
Materials and Methods
This was a retrospective study performed at a Level 3 trauma center. All patients were operated by single fellowship trained orthopaedic trauma surgeon. Patients were identified via a billing database for undergoing intramedullary treatment of a tibia shaft fracture from May of 2016 through December of 2018. IRB waiver was obtained prior to reviewing records in detail. The medical records and radiographs of all patients were reviewed. Patients were included in the study if they were treated for a closed or open tibia shaft fracture with an intramedullary implant and an open reduction was performed. Patients were included if they had completed 6 months of follow-up or until fracture union, whichever came first.
Demographic data was collected; age, gender, tobacco use and presence of medical comorbidities, such as diabetes or renal insufficiency. Mechanism of injury and surgical positioning was recorded as well. ASA score was collected as well to provide a sense of frailty of this patient population. Time from injury to surgery was recorded as well. Most frequently patients were admitted and underwent repair the same day or next day. All patients were treatment with a similar surgical technique. In either a semi extended position or a flexed position, an open reduction was performed though an anterior incision in order to reduce the fracture. The incision length was determined by the fracture length and complexity. It was typically 5-7 cm in length, usually just lateral to the tibial crest. Care was taken not to strip the fracture fragments of soft tissue connections and soft tissues were gently handled for the entire case. If the fracture was open, the open wound was extended and the fracture reduced through that incision. The selection was made by the treating surgeon during a
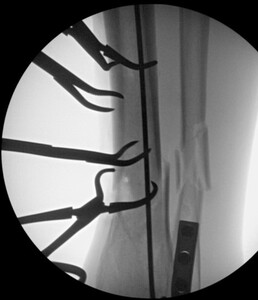
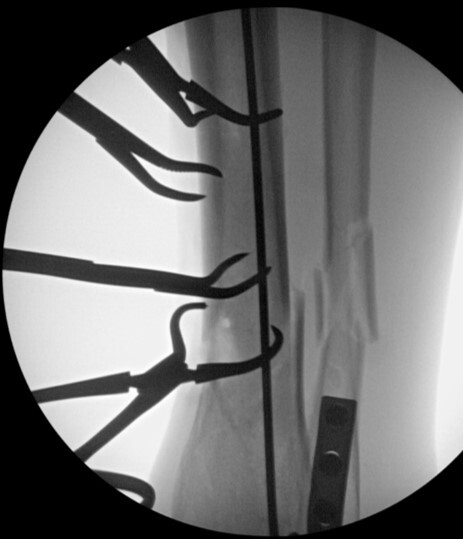
time of transition from a flexed position to semi extended position. This was not dictated by fracture location or type. It is current practice to use the semi extended position in the majority of cases currently. Multiple bone reduction forceps were used to obtain and maintain this reduction. If the fracture was transverse in nature then small drill holes were placed on either side of the fracture and then reduction forceps were used to reduce the fracture. Provisional plates were not used in this series. Please see figures below for radiographs of a representative case. All portions of the case were completed by the treating surgeon as there are few operative assistants available in this clinical setting. The intramedullary nail was then placed though an extraarticular lateral parapatellar approach in a semi extended position (Kubiak, Widmer, and Horwitz 2010) or through a medial parapatellar approach with the knee flexed over a radiolucent triangle. If the fibula was fractured, it was not routinely operatively repaired unless the ankle was found to be unstable. If the ankle was unstable, then the fibula was treated through a separate incision with a plate and screw construct. All wounds were closed in layers with absorbable suture for the fascial layers. Either 0 or 2.0 Vicryl was used in interrupted figure of 8 fashion. All skin incisions were approximated with 3.0 nylon in modified Allgower-Donati fashion (Shannon et al. 2017). All patients were placed into well-padded short leg plaster splint with the foot in neutral dorsiflexion and made non weight bearing until wounds were healed and sutures were removed. At that point all patient were made weight bearing as tolerated on the effected extremity with or without a cast boot as the patient desired.
Superficial wound complications were defined as any wound dehiscence, drainage or cellulitis that resolved with nonoperative treatment such as oral antibiotics or topical wound care. Deep infections were defined as infections requiring reoperation for debridement. Radiographic union was defined at having bridging callus across 3 of 4 cortices with the patient able to ambulate with minimal support. Nonunion was defined as no progression of healing on radiographs 9 months after injury. Any secondary reoperations, such as hardware removal or nonunion repair were recorded as well. While secondary reoperations were recorded, hardware removal rates were not the aim of this study.
Results
Thirty-nine patients were identified who had intramedullary treatment of tibia shaft fracture. A total of 32 patients met inclusion criteria. The average age of the cohort was 47 years with a range of 16-82 years. There were 17 males and 15 females. Seven patients consumed tobacco. A traditional knee flexion technique was used in 22 patients and a semi-extended approach was used in 10 patients. Average and median ASA score was 2.0 for this group. Average follow up was 8.5 months (R 2-18 months). Average time from injury to was 1.9 days (R 0-10 days). All but 3 cases were performed within 3 days of injury. There were 4 open fractures and 28 closed fractures. There was one Gustilo-Anderson grade I, 1 grade II and 2 grade IIIA. Please tables below for AO/OTA classification as well as relative fracture location. The most common mechanism in jury was fall with 16 cases followed by motor vehicle crash with 5 injuries. Sport related injuries resulted in four fractures. Three of which were related to soccer and one was related to snow skiing. Three patients were pedestrians hit by cars and one patient was injured while riding a horse.
Out of the 32 patients, zero patients required reoperation for deep infection. 2 of 32 required a short course of oral antibiotics for reported cellulitis after these patients visited outside urgent cares. On follow up exams with the treating surgeon in these 2 cases no sign of active infection was found on exam and antibiotics were discontinued. One patient did use tobacco and also had a history for alcohol abuse. The other patient had diabetes mellitus and atrial fibrillation. Both of these were closed injuries as well. In both cases, wounds healed uneventfully without any further procedures or treatment required. Four patients required reoperation for painful hardware, in all cases distal bolt or associated plates for fibula fixation were removed. One patient had one prominent locking bolt removed in the office under local anesthesia. No reoperations were needed for nonunion. All fractures were found to be healed radiographically at time of final follow up for each patient.
Discussion
There have been 2 prior reports that have examined the possible detrimental effects of open reduction on tibia shaft fractures. The most recent examined a cohort of 315 tibia fracture (Auston et al. 2017), of which 56 were treated with open reduction, 61 were treated with percutaneous reduction and 200 were treated with closed reduction. This study was performed at a level 1 trauma center with fellowship trained traumatologists as well as resident and fellows to assist with the case. There was no statistically significant difference in wound complications, deep infections and nonunion.
The second report examined the outcomes of 119 tibia shaft fractures of which 40 were treated with open reduction (Tang et al. 2006). Once again this was a study from a level 1 trauma center and there was no statistically significant difference in terms of wound complications, deep infections and nonunion. No other reports were found that specifically reported on this aspect of tibia shaft fracture care. In summary, between the two previous reports the complications of open reduction of only 96 tibia shaft fractures have been reported. This report would add a significant number of cases when viewed in that light.
This study supports previous reports that open reduction does not negatively effect the healing of tibia shaft fractures. That being said there are a number of caveats for this technique that are important. The soft tissue must be handled gently and minimal stripping of the bony fragments is required. Additionally, attention to detail must be adhered in the closure of the incision used to reduce the fracture.
This study has a number of possible weak points. First, no patient reported outcomes were obtained for this study. Second, the judgement of fracture healing was performed by the investigator and not by blinded independent judges. Third, there was not a comparison group of fractures treated with closed reduction to compare to. This is a limitation of the number of tibia fractures at this facility as well as the associated resources. All of the tibia cases were performed by the same surgeon with a single scrub technician to help with the case. It was the judgement of the surgeon that open reduction was the most efficient way to help this population of patients in this particular setting.
Strengths of this study include all surgeries being done by a single surgeon in a diverse population that could represent a more generalizable population. Another strength is that the outcomes measures are objective in the sense that deep infection and nonunion require further surgery and this cohort did not require surgery for either of these indications.
The clinical relevance of this study is that it supports the use of open reduction of tibia shaft fractures in order to achieve reductions without increasing the incidence of complications that require a return to the operating room, such as deep infection or nonunion. This technique does require attention to detail in order to achieve these results.
Conclusion
This study demonstrates that acceptably low rates of wound complications, nonunion and reoperations can be achieved when open reduction and intramedullary treatment of tibia shaft fractures is performed by a fellowship trained orthopaedic trauma surgeon in community type setting. This data can be used to support this technique being used in a diverse set of patients that can be encountered in a majority of hospitals in the United States.