Introduction
Sacroiliac(SI) and transiliac-transsacral(TITS) screw fixation have become well accepted means of posterior ring fixation in pelvic fractures requiring operative fixation. Chronic pain, disability and sexual dysfunction are well documented complications of pelvic ring injury and fixation. Retained posterior implants have been cited as a possible source of pain due to decreased mobility, arthritis and chronic pain (Quade et al. 2019). There is disagreement among surgeons as to the true incidence of symptomatic implants, the benefit of implant removal and the safety of this procedure. Some suggest routine removal of implants (Culemann et al. 2004; Gänsslen, Hüfner, and Krettek 2006). Others recommend removal only in event of complications (Abumi et al. 2000; Chip Routt, Simonian, and Mills 1997). Our objective is to document the incidence of symptomatic posterior pelvic screw fixation, the complication rate of this procedure and the clinical outcome associated with screw removal.
Materials and Methods
Following investigational review board approval, the trauma database for our hospital’s four trauma fellowship trained orthopedic surgeons was queried from January 2006 to January 2018 to identify patients treated with sacroiliac (SI) or transiliac-transsacral (TITS) screw fixation.
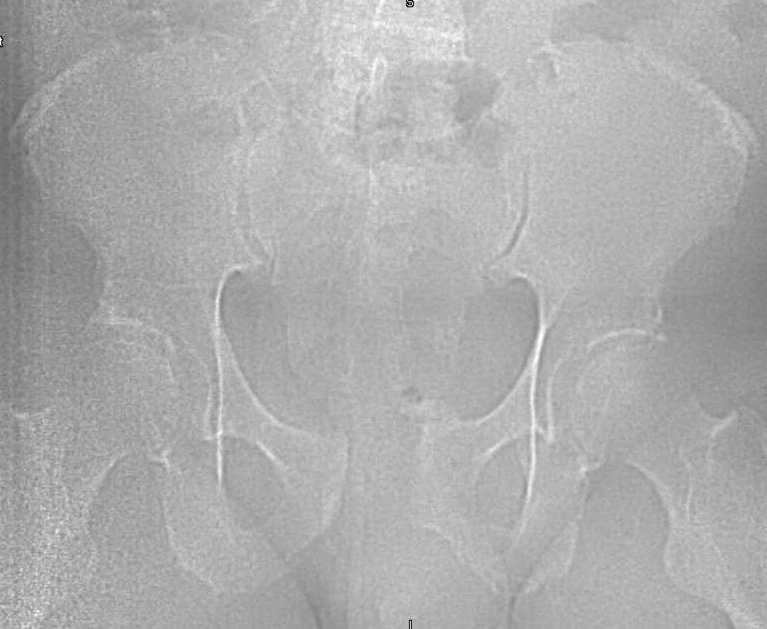
Chart review was undertaken to obtain basic demographic variables such as age, sex, smoking and diabetic history. Injury radiographs were reviewed to determine fracture type and Young-Burgess fracture classification. Preoperative and postoperative radiographs are demonstrated in figures 1A, 1B, 2A and 2B. Operative records were reviewed to determine which patients underwent screw removal and if any adverse intra-operative events occurred. Hospital charts and clinic charts were reviewed to document any postoperative complications and record pre and postoperative visual analog pain scales.
Results
Two hundred and fifty patients with 300 posterior pelvic ring screws were identified. 195 screws were SI and 105 screws were TITS. 46/250 (18.4%) patients underwent implant removal, accounting for 66 screws. Mean patient age was 42.5 years (+/-2.4). There were 28 males and 18 females. 43 patients cited pain as reason for removal and 3 patients cited infection. (Table 1) In patients requiring screw removal, fracture patterns by the Young and Burgess classification were 17 APC2, 5 APC3, 7 LC1, 13 LC2, and 4 LC3. (Table 2) Average time to implant removal was 6.7 months (+/- 1.8 months). 23.5 percent of SI screws and 19.7 percent of TITS screws were removed (p=0.61). No intra-operative complications or postoperative complications occurred. Some measure of pain relief occurred in all patients with mean preoperative and postoperative pain scales of 4.91 and 0.51 respectively (p<0.001). Mean follow up time for patients with implant removal was 34 months (+/- 3.1). (Table 3)
Discussion
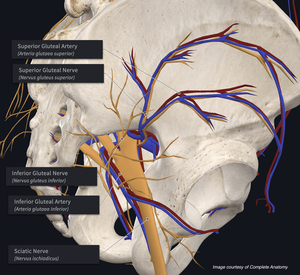
Posterior pelvic ring fixation with SI or TITS fixation is a well-accepted, successful means of fixation with good outcomes. Despite its widespread utilization, a paucity of publications exists on the indications and results of implant removal (Abumi et al. 2000; Culemann et al. 2004; Gänsslen, Hüfner, and Krettek 2006; Chip Routt, Simonian, and Mills 1997). Several case reports have demonstrated the proximity of neurovascular structures to these screws and demonstrated the possible risks associated with screw removal (Ebraheim et al. 1997; Mirkovic et al. 1991; Chip Routt, Simonian, and Mills 1997; Templeman et al. 1996). Figure 3 presents a diagram showing the proximity of neurovascular structures most likely to be damaged during placement or removal surgery.
In 2019, Quade et al found a 5.4% incidence of implant removal in patients treated with SI or TITS screw fixation. No intra-operative or postoperative complications occurred during implant removal and 83% of patients had improved symptoms with implant removal. Average time to removal was 10.7 months (Quade et al. 2019). Our study supports these findings. Our patients had a slightly higher incidence of implant pain and removal. In addition, patients did benefit from implant removal. In this study, average time to implant removal was 6.7 months, demonstrating that patients with painful implants can safely have their implants removed 4 months sooner than previously published.
This study is retrospective in nature and as a result is subject to certain bias. It is possible that some patients went elsewhere for screw removal after the data collection period was finished. However, our facility is geographically isolated and such a possibility is unlikely. Visual analog scale pain scales are subject to recall bias, but this should be similar across all patients. Pelvic ring fractures are complex injuries with many possible associated bone, muscle, ligament, nerve, and tendon injuries that could cause pain unrelated to implant position.
In conclusion, posterior pelvic ring fixation with SI or TITS screws is a well-accepted, successful means of posterior pelvic ring fracture fixation. Symptomatic implants are a reported complication occurring in 18% of patients. Implant removal is a safe procedure that is associated with improved subjective pain relief. Over 6 months following the index operation, implant removal appears to be a safe and effective procedure.