For everybody here my five, and then I thought six pearls for hip revision because five just isn’t enough. I think probably one of the things that’s very important, it’s kind of underrated is “what implant do I have to revise?” I think it’s really important to identify exactly who your enemy is, because that’s how I consider this whenever I do these cases, they’re almost like the enemy. This is very interesting. The app is called Implant Identifier. (Figure 1)
You can download it off the app store. It is this huge catalog of implants, and the things that are lacking probably are the timelines when these came out, and when they were retired (those are some things that are probably that should be done). But nevertheless, what I would say is it’s an excellent app to have for your staff.
Again, the idea is to identify it. Based off that, you can come up with some specific extraction equipment that is actually the manufacturer provides. Modular implants sometimes need special instrumentation for extraction, and we previously talked a little bit about trephine reamers. If you’re going to keep the femoral components, sometimes you want to know what the neck tapers are. There’s just so much to gather from truly identifying what the component is. If you’re going to remove it, is it a full coat or partial coat? And sometimes the technical and salespeople really know where the problems are with this. However, if you just make assumptions, then you’re most likely to end up being a loser. A lot of times there won’t be anybody locally to help you, and that’s why this app actually probably is helpful and also to understand when the component was available. If you’re seeing somebody that had a surgery 20 years ago in the US we keep terrible records. Another thing that’s very important to me, and this was drilled home to me by George Cerney, who was my mentor when I was in practice, basically a physiologic classification of the patient too. When I assess patients, the first thing I do is I think about this classification and where these patients stand.
This is his classic paper. (Figure 2)
Of course he’s talking about adult osteomyelitis. But the thing is what is so important from this paper, but aside from osteo classification, is the host classification. That’s real key.
A Host: Healthy, no healing deficiencies
B Host: Systemically compromised
(e.g.: diabetes, psoriatic arthritis, lesions over the front of a knee or hip).
C Host: Does the morbidity of care exceed their illness and surpasses our capacity to withstand curative treatment?
(Is the treatment that you’re suggesting actually worse than the disease process?)
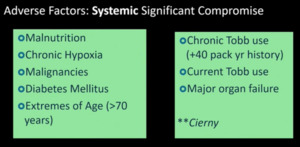
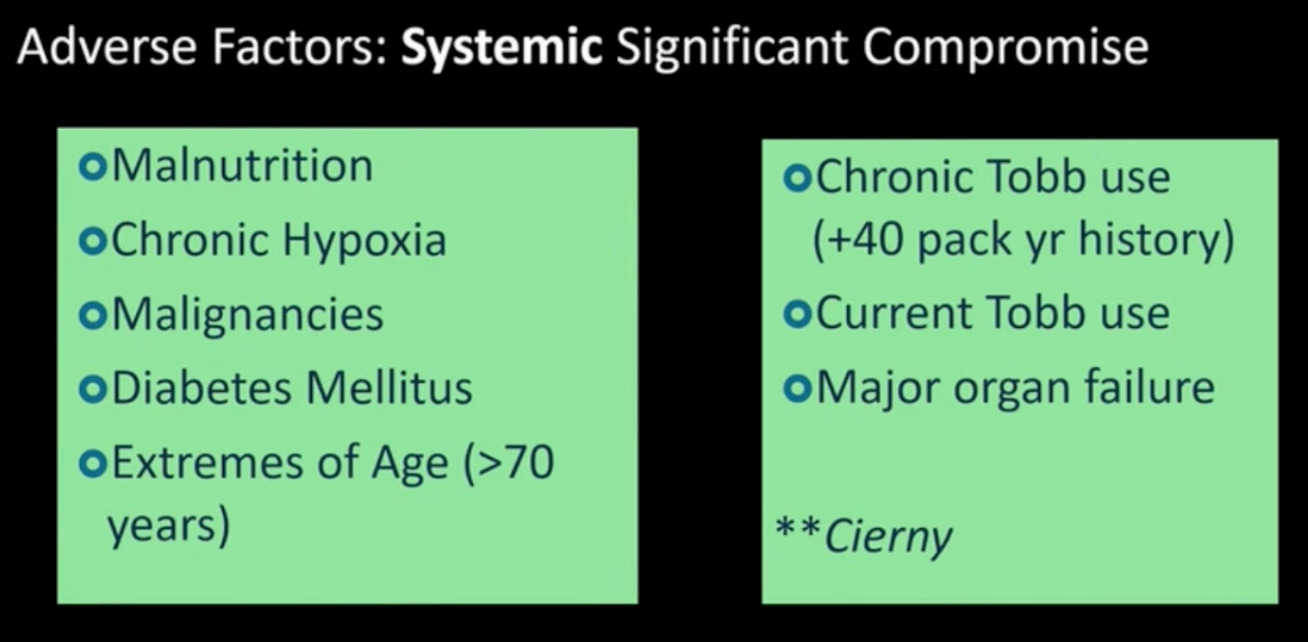
For me, these are key things to help me move forward with decision making. These are some of the systemic things that he identified, and you can see the list here. (Figure 3)
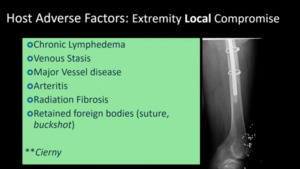
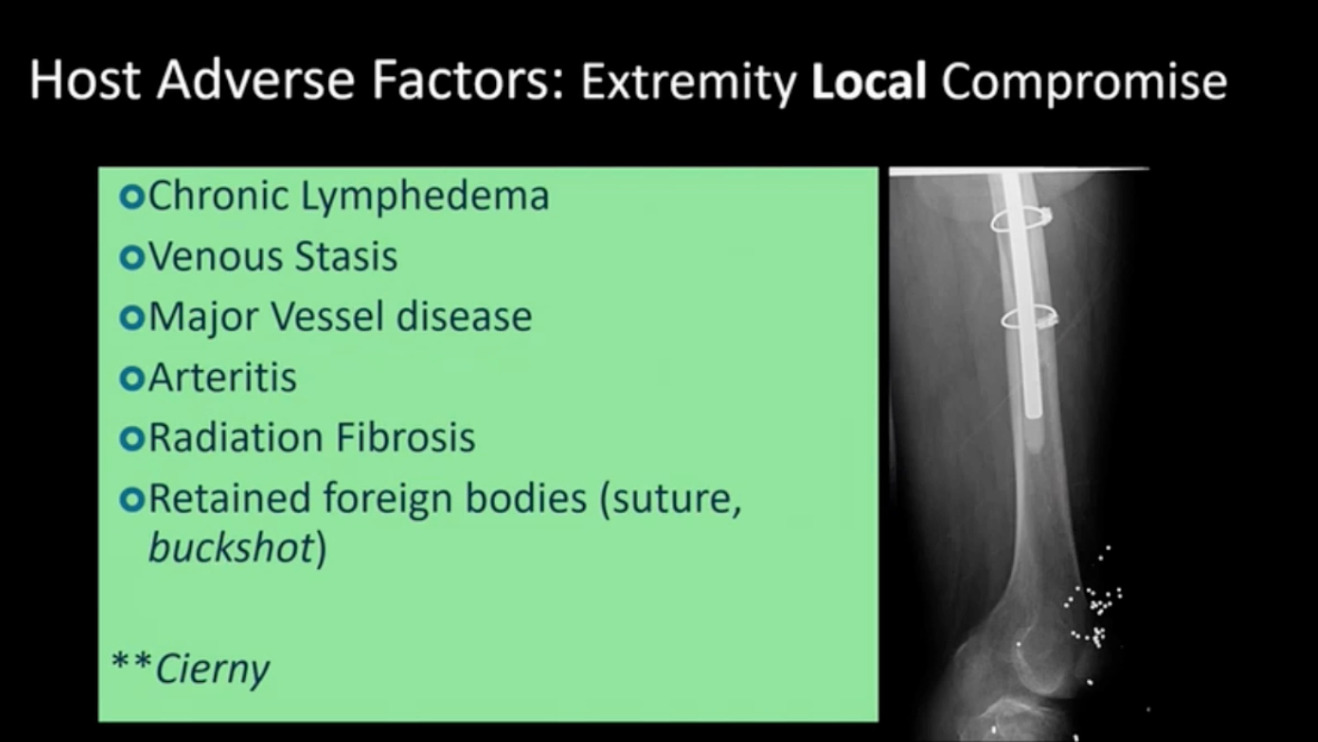
These are all the extremes of people that are especially aged, infirm, or just have multiple health problems. These are some of the local compromises that we see. (Figure 4)
Chronic lymphedema, I think that’s terribly underrated. Vessel disease arteritis. I’ve got somebody here with retained buckshot from a shotgun injury.
These are the things that it’s important to try to understand. The other thing too is, and it’s been highlighted already, is rule out infection. Absolutely 100% rule out infection. I definitely follow the ICM recommendations. We’ve got new recommendations coming out. I was an Istanbul slugging it out with everybody else trying to figure out what is really the best solution. Bution addition to the standard blood tests, you really need to get a careful history. How many surgeries, was there a complication? And then aspiration and for B open biopsy is a very small incision that I make around the hip or knee to do open biopsy testing. I don’t really trust cultures because they notoriously are negative. In addition, one of the things that I absolutely use is next generation sequencing.
What was great about, and this is a slide from the ICM Congress. It’d be great to have a hundred percent, but we’ll never get it. But 92% of the delegates endorse molecular diagnostics and next generation sequencing. And for me, there’s so many patients that come in with a history of, the doctor aspirated, but it was negative and I do one of these tests, it comes back positive. It’s very important to do that.
The other one, this has been gone over as well. Exposure is key! You have to be able to see what you’re doing. So whatever approach works for you is the one you should absolutely consider. Then the equipment. I spoke recently in Ecuador and I was so amazed at what my South American colleagues are able to accomplish a lot of times without all these fancy gadgets that we have in the US. We’ve got Watsons, we’ve got all this extraction stuff. I’ve got a versa driver pneumatic chisel. I’ve got cup extractors that are powered. It’s crazy all the things that we have. But you want to take advantage of those. If you have access, please I would urge you to consider that.
Then you have implant choices. There are so many decisions that you have to make based off what you’ve anticipated so far, and as you work up the patient. Whether it’s modular or non-modular or you got a tri-flange or jumbo, it’s in your hands based off what you see. For implant choices, you have to understand the pathology and make your choices based on the above and on your experience without a doubt.
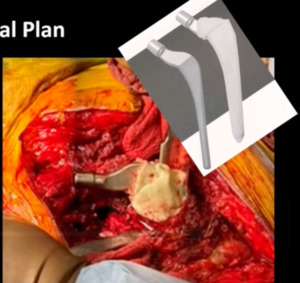
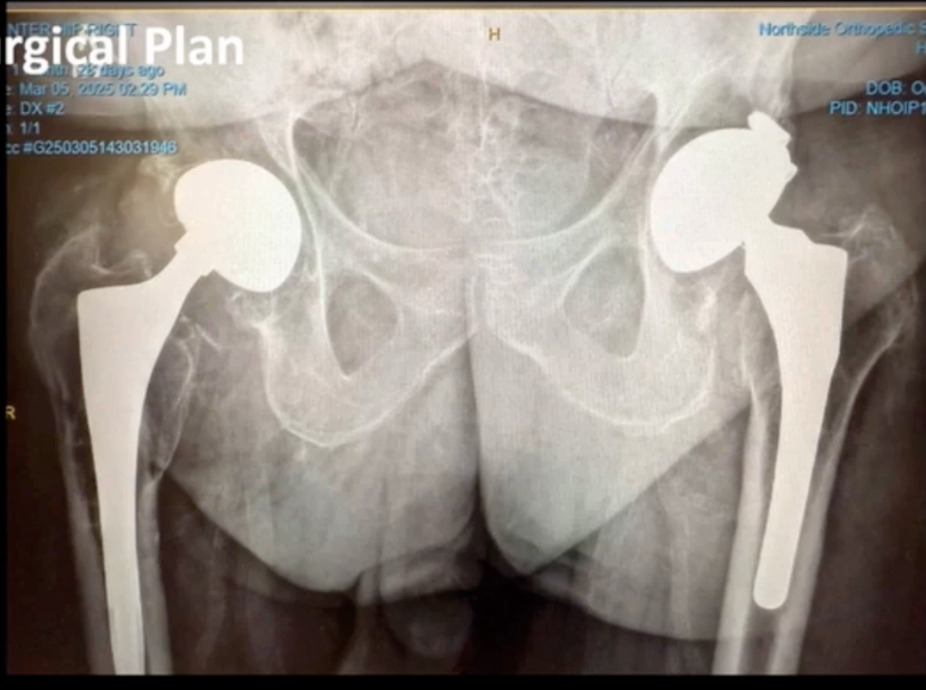
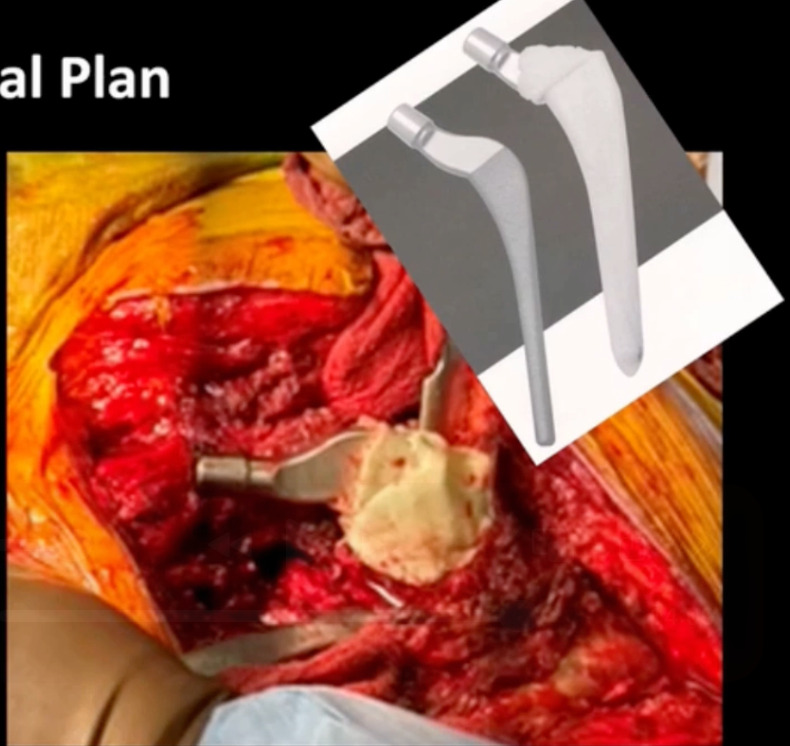
Also, I definitely like to avoid multiple implant representatives and companies, and in the OR, I like to stick with one. One of the problems I see is that there’s just so many people in the operating room. I have to “get 'em out of the way.” Actually, I can even operate on people. That’s important. That would be number six. Just to show you a case example this was a male patient came in with bilateral hip pain. (Figure 5)
His hips were done quite a while ago and recently, he had a coronary artery bypass. He’s got melanoma venous insufficiency. Just very exciting history. He’s pretty much a B bordering, not a C patient, but a definitely a B patient. We aspirated his right hip. It was negative, but the left hip unfortunately was positive on aspiration. He came back polymicrobial on next generation sequencing. But the only bug we came up with on culture was a corynebacterium. He had asymmetrical poly wear. We also did a metal ion workup through blood testing and he had really high metal ion levels. I was really concerned that he had worn through in an area and had metal ion activity. To look at it face value you’re prone to say, “okay, we can do that.” But things don’t always work out well.
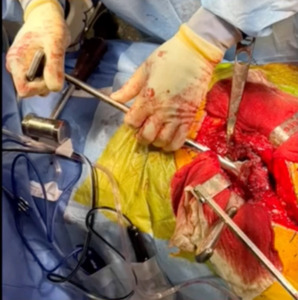
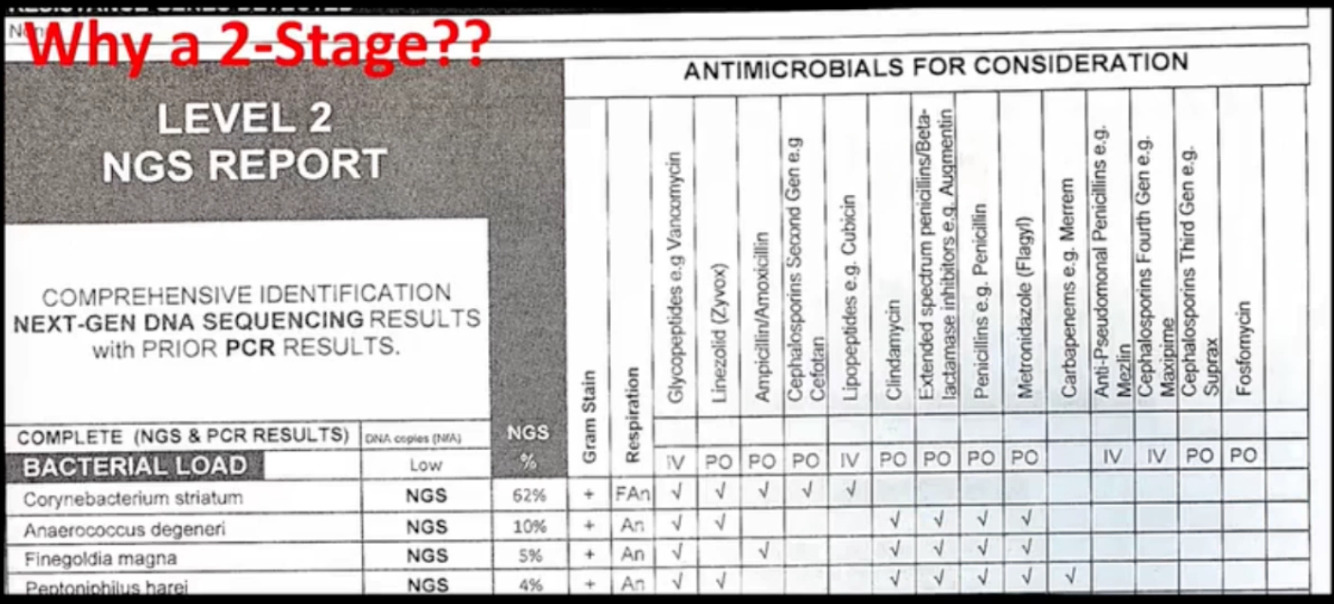
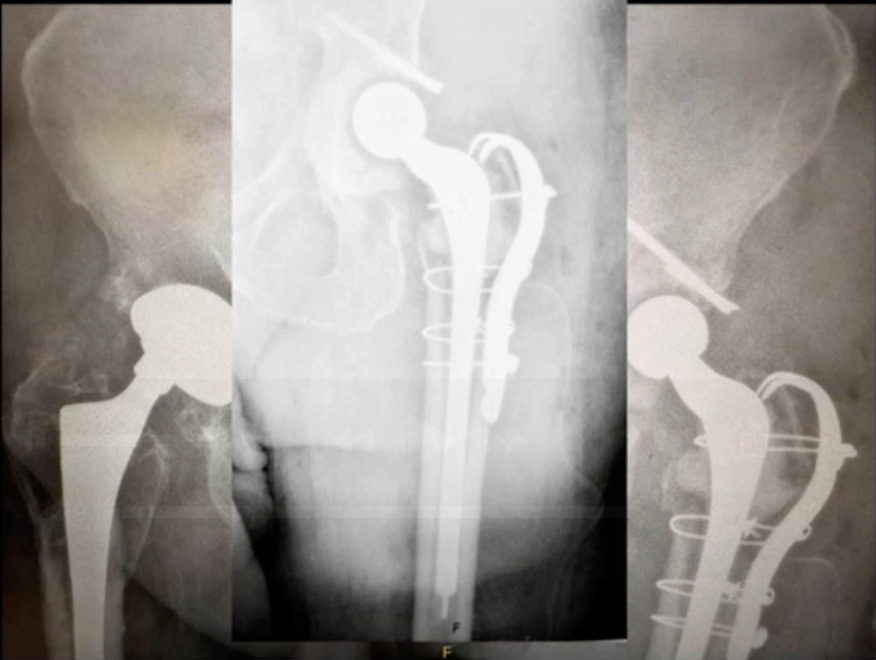
But nevertheless I applied all these steps. All these pearls to get us to a point where we operated. The right hip was fine at least for right now. The left hip that’s infected. I suggested that we do a two-stage revision. The patient endorsed that. Why did we do it? The following is the report we received. (Figure 6)
Corynebacterium, an enterococcus of finegoldia, which I’ve seen from time to time. Polymicrobial organisms in what was a negative culture. So nevertheless, what I would tell you is that I think it’s a strong consideration. Again, this is next generation sequencing.
Exposure. Just whatever’s comfortable, I do a direct lateral. I’ve been doing it for 32 years after fellowship. I like to use a Midas Rex pencil-tip burr to get around the shoulder. I think it’s a great way to just open up that bone area. You can also do that underneath a calcar. I do like to take advantage of these really cool tools that we have. Watson, osteotomes, femoral extractors. Anything I can do that will make my job easier and faster I’ll definitely try to take advantage of.
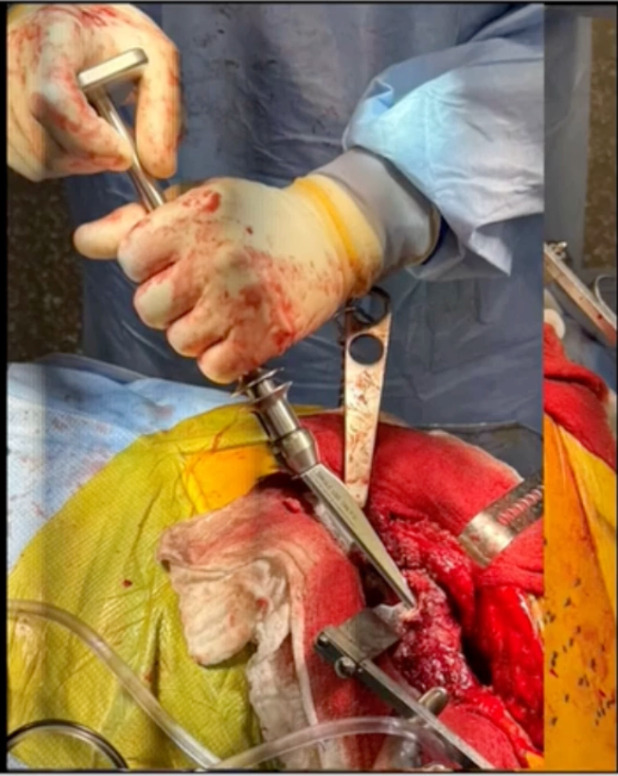
This is an example of the Watson going around the shoulder of the implant. (Figure 7)
It’s a nice tool until you crack the trochanter then, and maybe it’s not so. Nevertheless, these tools are great.
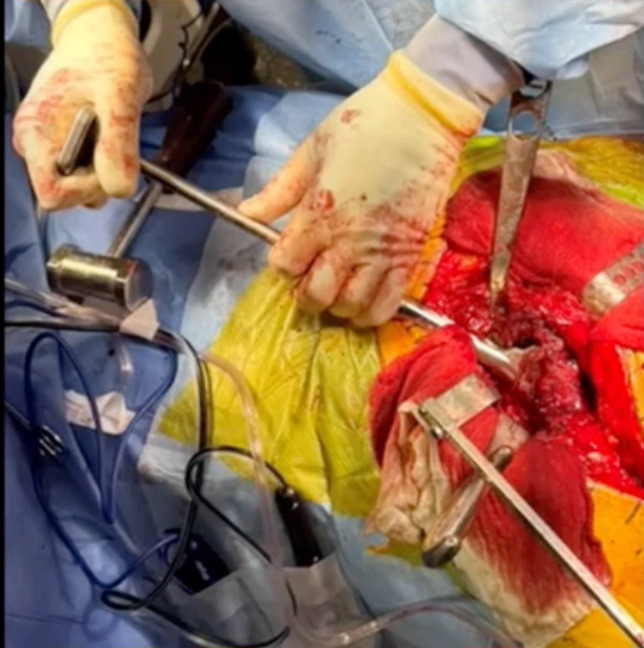
This is one around the calcar area. The idea is to use what you can to make it happen. (Figure 8)
Cup osteotomes. This is an example of just using our Slap Hammer extractor. (Figure 9)
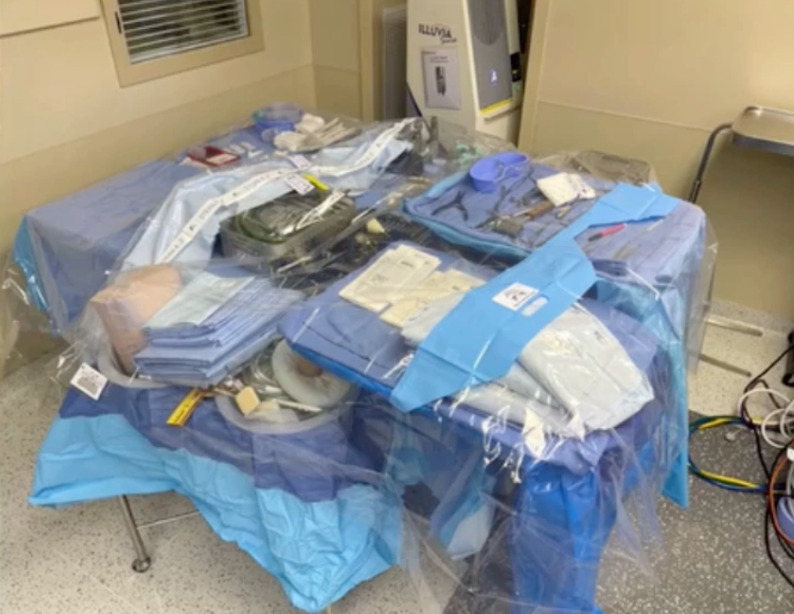
We’re able to successfully extract the cup. He did have really poor proximal bone around that shoulder. He ended up having a fracture there as well. But got the cup out, did all the things here important. But the idea is that because he did have an infection, you’ve got to do an aggressive debridement. That’s one thing I was taught. It’s almost an oncologic debridement. I do use some products that are available to us in the US. Bactisure antiseptic lavage, which is a kind of a flamethrower not dissimilar to Daikin’s, but probably less harmful and then another product called Xperience antiseptic lavage. But the idea, as Cerny emphasized to me, was a double setup. (Figure 10)
You have a dirty side and a clean side. It was great to see at the ENDO-Klinik that they do these same things. We take advantage of the tools that are available to us. This is an example of double setup. This is our clean side. What we do is we cover that with a polyethylene sheet. (Figure 10)
I have text on either side. It just pulls apart. After you’ve done all the prep and drape and do the things you need to do to expose that, then we “pop that open” and we’re ready to go. Also interestingly, I wanted to add this, that this double setup was also endorsed by our delegation. I don’t remember what the percentage was, but it was incredibly high and it was great to get agreement on this. In this particular case, and I’ve just used this for years. I just like, and I’m comfortable with it. (Figure 11)
I use a Prostalac™ cement because it was a polymicrobial, I decided to go with this and we loaded them up with this. And this was our final solution. (Figure 12)
I like to use the Prostalac™ liner. It’s a semi-constrained liner it works well in my hands and it’s got extremely low dislocation rate if you put it in the proper version.
In conclusion, these are my five or six actual pearls. I think preparation is key. There’s no question about it. You want to think about worst case scenarios. “Luck favors the prepared” and I would say good luck.
Finally,
“Good judgment comes from experience and experience well, that comes from poor judgment.”