Introduction
Subtalar arthrodesis presents a challenge to the surgeon due to the complexity of the joint anatomy, where the resulting mechanical stresses need to be minimized during the recovery phase. This anatomy, below the ankle, also limits the blood supply available which can potentially slow down the healing process (Rao et al. 2014). The success rates of primary subtalar arthrodesis are typically high but varied (Chraim et al. 2021; Chahal et al. 2006; Hungerer et al. 2011). In post-traumatic patients, further disruption of the blood supply, particularly involving the talus, can add additional risk (Rao et al. 2014; Kim et al. 2023; Hungerer et al. 2011). In revision of subtalar fusion procedures these challenges are even more prevalent (Chraim et al. 2021; Lerch, Gulati, and Highlander 2023).
In a reported series of 101 patients with posttraumatic subtalar arthrodesis, the non-union rate requiring revision was 24%. After revision surgery the failure rate was 12%. Consolidation of the graft occurred after 6.4 ± 6.3 months for primary procedures and took longer for revision surgery at 9.4 ± 13.1 months (Chraim et al. 2021; Hungerer et al. 2011). An additional series of 115 subtalar fusion revisions reported a 20% incidence of painful non-union (Chraim et al. 2021; Hungerer et al. 2011; Lerch, Gulati, and Highlander 2023). In a series of 88 patients with primary subtalar arthrodesis various patient risk factors were observed to affect the success rate of subtalar arthrodesis (age, smoking, diabetes, etc.) (Chahal et al. 2006). This was also reported in greater detail with a 119-patient multicenter retrospective study, which also found that the use of fully threaded screws was more likely to achieve bone union compared to partially threaded screws (Kim et al. 2023).
The use of autograft bone is believed to improve subtalar arthrodesis rates and historically is harvested from the pelvis (Miller and Chiodo 2016; Lareau et al. 2015). However, there is substantially increased morbidity with this harvest site (pain, additional surgical site infection risk, etc.) (Vaccaro et al. 2002). Harvesting from sites of the lower extremity such as the distal femur, proximal or distal tibia, and calcaneus also are options but with limited bone volumes (Danziger, Abdo, and Decker 1995).
Synthetic bone graft substitutes can reduce or eliminate the need and subsequent complications of autograft harvest and expand the amount of graft material available for fusion. In addition, knowledge of the exact specifications of the materials present, as opposed to bone bank allograft or cellular allograft, is advantageous (Vaccaro et al. 2002). Synthetic bone grafts are mostly calcium-based compounds containing hydroxyapatite (HA) and tricalcium phosphate (TCP), which resemble natural bone and are osteoconductive. Some may exhibit osteointegrative properties (Moore, Graves, and Bain 2001). The design properties of synthetic bone grafts have progressed over the years to include ionic substitution, nanoscale architecture, and enhanced surface technology, even more closely resembling human bone. This is far different from the more common sintered ceramic architecture which results in sizes many orders of magnitude larger.
A silicate enriched (5.8wt% silicon) calcium phosphate bone graft substitute (OssDsign Catalyst®) was designed so that the nanoarchitecture and site-specific silicate substitution mimic the structure of natural bone mineral. The material has been shown to activate both intramembranous and endochondral ossification, of which the latter is of particular interest where blood supply is limited (Conway et al. 2021; Bernhard et al. 2022). Catalyst has shown encouraging results in both animal models and early clinical use in spine fusion procedures (Conway et al. 2021; Gibson et al. 2025; Lazary et al. 2024; Sadrameli, Archer, and Czop 2024; Strenge, Archer, and Czop 2024).
Case Description
A 72-year-old male patient with a history of posttraumatic subtalar joint arthritis treated with a subtalar arthrodesis two years prior (two screw construct with calcaneal autograft bone), presented with constant pain (VAS 7/10) and antalgic gait (limping), along with tenderness at the subtalar joint. Comorbidities included hyperlipidemia and an undetermined (work-up in progress) autoimmune disorder, otherwise the patient was fairly healthy.
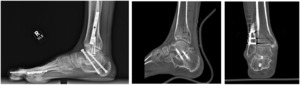
The patient underwent radiological examination (both X-Ray and CT Scan), and it was determined that the previous subtalar arthrodesis had failed (Figure 1), and the patient would require revision surgery. There was no gross evidence of infection preoperatively or intraoperatively.
The revision surgery included removal of the original screws, debridement of the pseudoarthrosis, reparation of the joint surfaces, and placement of larger fully threaded screws. A single extensile lateral sinus tarsi approach was performed. Joint preparation was performed with a powered pneumatic osteotome and curved curettes. Smooth and toothed lamina spreaders were used for visualization. Five ccs of Catalyst bone graft substitute were mixed with a small amount of calcaneal autograft (of somewhat poor quality) thus completing the revised construct.
The patient followed a standard course of non-weight bearing for the first 6 weeks postop immobilized in a short leg cast and an additional 6 weeks of gradual weight bearing in a cam boot walker with physical therapy. At three months post-operative the pain had resolved (VAS 0/10) and there was no tenderness noted at the subtalar joint.
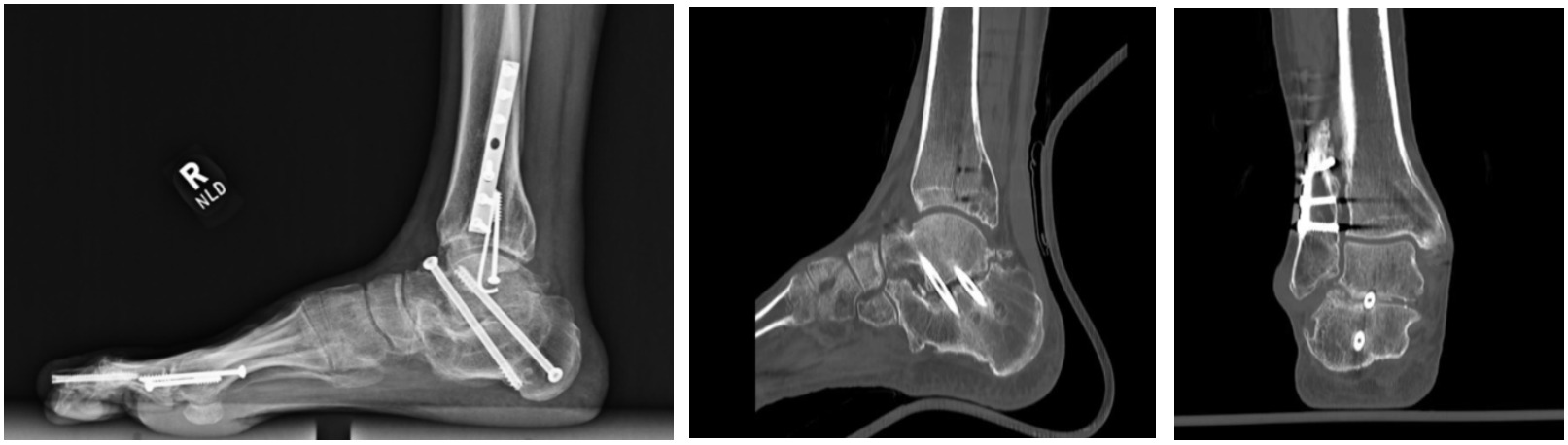
Radiographic evaluation (X-Ray and CT Scans) at this 3-month timepoint showed intact and well positioned screws and evidence of early and complete consolidation of the bone graft (Figure 2). At this point, the patient returned to full weight bearing and was able to walk free of pain with regular shoes. There were no complications noted during surgery or post-operatively.
Discussion
This patient and the case description demonstrate a challenging scenario for achieving a positive outcome. The need for revision surgery along with the prior history of subtalar arthritis secondary to trauma require careful thought for the selection of appropriate surgical adjuncts. The use of fully threaded larger screws was needed to securely stabilize the construct. The bone graft used for this case (OssDsign Catalyst® Bone Graft) was selected based on its handling and performance characteristics. In this instance, the most important performance feature of Catalyst was shown in a rabbit fusion study conducted prior to commercial availability (referred to as Osteo3 ZP Putty). Histology of tissue samples of the progressively healing bone graft at specific time points showed regions of chondroblastic tissue between Catalyst granules, indicating new bone forming through endochondral ossification (Vaccaro et al. 2002). This pathway is characterized by the initial formation of collagen matrix, followed by hypertrophic chondrocyte-mediated bone formation. This performance characteristic is advantageous when vascularization, extensive rapid bone formation, and mechanical strength are needed, and is not typically observed as a predominant mechanism of bone formation in other synthetic grafts (Danziger, Abdo, and Decker 1995).
The combination of surgeon skill and experience in selecting the most appropriate and effective surgical adjuncts, including both the use of larger fully threaded screws and choice of bone graft, resulted in an unexpectedly early and excellent clinical outcome. Further research in foot and ankle procedures with longer follow-up will be needed to determine the repeatability and durability of the results in this challenging case.

.png)
.png)