Introduction
Total hip arthroplasty (THA) is one of the most successful and commonly performed operations in the United States annually (Shichman, Roof, Askew, et al. 2023; Learmonth, Young, and Rorabeck 2007). Given excellent clinical outcomes combined with an aging population, the prevalence of THA is on the rise and estimated to increase by 140% by 2040 and over 600% by 2060 (Shichman, Roof, Askew, et al. 2023; Patel et al. 2023). Continued improvements in material sciences and bioengineering have contributed to the development of cementless femoral stems with long-term survivability (Y. H. Kim, Park, and Jang 2021; Wyatt et al. 2014). Increasing utilization of cementless femoral stems in THA in the United States is multifactorial but can be partially contributed to consistent clinical outcomes, reduced operative time, reduced risk of cement pressurization and perceived improvements in long-term fixation in the growing cohort of young and active patients undergoing THA (Y. H. Kim et al. 2023; Radaelli et al. 2023).
While cementless stems offer reliable femoral fixation in many patients, the choice of femoral stem should be made on an individual basis as cementless implants have been shown to have increased risk of perioperative periprosthetic fracture in multiple database studies (Sassoon et al. 2024; Springer et al. 2019). Several classification schemes exist for cementless femoral stems (Radaelli et al. 2023; Khanuja et al. 2011; Kheir, Drayer, and Chen 2020). This article seeks to provide a comprehensive review of the principles of cementless femoral fixation and demonstrate their biomechanical application in modern implant designs to assist surgeons in the selection of appropriate patient-specific implants.
Biomechanics of Cementless Fixation
Successful outcomes in cementless THA rely on the three fundamentals of cementless fixation (Radaelli et al. 2023). First, rigid initial fixation achieved by direct contact between implant surface and prepared bone. Second, osseointegration for mid-term biologic fixation, and third, balanced femoral stress distribution which determines long-term survivability.
Rigid Initial Fixation
The first principle of cementless femoral fixation in THA is the generation of rigid initial fixation of implant to bone. The most important technical driver of initial fixation is meticulous femoral preparation. Femoral preparation is carried out in one of three manners depending on the implant and desired fixation method: ream only, ream and broach, or broach only. Individual stem geometry and intended location of bony fixation dictate the necessary method of fixation, but in general, shorter stems engineered to obtain metaphyseal fixation may be inserted with broach only technique while longer stems and those designed for diaphyseal engagement require reaming of the femoral canal with or without broaching (Radaelli et al. 2023; Kheir, Drayer, and Chen 2020; McCrosson et al. 2023).
Broach technique can be further subclassified into compaction, extraction or hybrid broaching, which combines compaction and extraction. A previous randomized study showed no difference between bone density or clinical outcomes at 5 years with compaction versus extraction broaching (Hjorth, Kold, Søballe, et al. 2017). Certain short metaphyseal loading stems have encouraged the so called “round the corner” broaching technique in which the broach is inserted medially and follows the natural curvature of the medial calcar to prepare the femur for implant insertion (Radaelli et al. 2023; Choi and Kim 2016).
Osseointegration
Biologic fixation in cementless THA is achieved via osseointegration. Osseointegration is described as the attachment of lamellar bone to implants without an intervening layer of fibrous tissue (Albrektsson et al. 1981). Crucially, the formation of bone versus fibrous tissue is determined by the stability of the initial fixation and amount of micromotion at the bone-implant interface (<28m yields bone, 28-150m mixture of bone and fibrous tissue, and >150 m only fibrous tissue formation) (Jasty et al. 1997). Furthermore, osseointegration can be achieved via ingrowth or ongrowth which is dictated by the surface of the implant or applied coating (Albrektsson et al. 1981; Bobyn et al. 1980). Ingrowth describes bone growing into the porous surface of an implant and requires implant pore sizes between 50–400m with a porosity of 40-50% (Bobyn et al. 1980). Existing implant surfaces designed to generate ingrowth include sintered beads, fiber mesh and porous metals (Kheir, Drayer, and Chen 2020). On the other hand, ongrowth occurs via bone grows onto a roughened nonporous surface such as that which occurs with grit blasting, plasma spraying or longitudinal grooves or splines (Radaelli et al. 2023; Kheir, Drayer, and Chen 2020). Studies have shown no difference in clinical or radiographic outcomes between ingrowth and ongrowth (Won, Dorr, and Wan 2004).
Additional osteoconductive coatings including hydroxyapatite (HA) have been applied to several implants following enhanced osseointegration in animal models (Søballe 1993). Clinical outcomes of HA coated stems are controversial. A study of 116,000 implants in the Nordic Arthroplasty Register Association database demonstrated no difference in survivorship comparing HA implants to no HA-coated implants (Hailer, Lazarinis, Mäkelä, et al. 2015). A meta-analysis performed by Chen et al. demonstrated no increased survival in the HA cohort but did show a reduction in thigh pain and Harris Hip Scores (Chen, Lin, Liu, et al. 2015). Conversely, the most recent meta-analysis by Kim et al. in 2024 reviewed 24 studies including over 2000 primary THA cases and found a significant reduction in stem revisions in the HA-coated cohort as well as decreased thigh pain compared to non-coated implants (W. T. Kim, Woodruff, Kalore, et al. 2024). Coating surface types for cementless femoral stems is summarized in Table 1.
Femoral Stress Distribution
While osseointegration drives short to mid-term outcomes, long-term success of cementless femoral implants requires appropriate femoral stress distribution. Stem geometry is perhaps the most critical driver of stress distribution and will be discussed in greater depth in the next section. Implant material is also an important factor to consider. The majority of cementless femoral stems are made of a titanium aluminum vanadium alloy with a minority being a cobalt-chrome molybdenum alloy (Radaelli et al. 2023). Titanium alloys are preferred in cementless implants due to a closer modulus of elasticity to cortical bone (100 GPa compared to 20 GPa) that facilitates osseointegration and more evenly distributes stress to the proximal femur (Healy et al. 2009). Contrarily, cobalt-chrome has a significantly higher modulus of elasticity than cortical bone (220 GPa) that can theoretically lead to increased stress shielding and thigh pain, potentially leading to early loosening (Healy et al. 2009).
Stem Design
Stem design incorporates several independent aspects in the engineering of femoral implants. The most important factor is stem geometry, which determines the site of cortical contact between the implant and bone. Additional considerations include presence or absence of a calcar collar, nature and location of any surface coatings, stem length, modularity and variety of neck angles/offset. The updated cementless femoral stem classification system by Radaeli et al. considers 6 essential stem geometries: flat tapers, quadrangular tapers, fit-and-fill, conical, cylindrical, and calcar guided short stems (Figure 1) (Radaelli et al. 2023).
Stem Geometry
Type A: Tapered
The first category of stem geometry are tapered stems. Single tapered stems taper only in the coronal plane and may be flat or rectangular in the sagittal plane depending on the desired metaphyseal fill. This implant achieves fixation via medial to lateral metaphyseal cortical bone engagement and 3-point fixation along the length of the stem (Radaelli et al. 2023). These stems typically require broach only bone preparation.
Type B: Quadrangular Tapered
These femoral stems exhibit a quadrangular cross-sectional geometry where initial rigid fixation is achieved in the metaphyseal and proximal diaphyseal regions, particularly in the coronal plane, while providing greater engagement in the sagittal plane when compared to single taper designs. This configuration facilitates a more uniform distribution of mechanical loads across the proximal cortical bone and contributes to enhanced torsional stability (Figure 1). These implants are typically intended for insertion using a broach-only technique and are classified into three distinct subtypes (Radaelli et al. 2023).
Type B1: Rectangular Taper Stems
Type B1 stems are characterized by a rectangular cross-section and a gradual taper. Their primary fixation occurs within the meta-diaphyseal junction, providing robust coronal plane engagement with improved sagittal fill compared to Type A stems (Radaelli et al. 2023).
Type B2: Quadrangular Taper Stems
Unlike B1 stems, Type B2 designs incorporate a metaphyseal taper in both the coronal and sagittal planes. This promotes closer contact with the proximal cortical bone, thereby improving load transfer. Additionally, a lateral taper design is incorporated to preserve trochanteric bone during canal access. Proximally, these stems demonstrate a trapezoidal configuration due to a taper from lateral to medial, whereas the distal portion maintains a more rectangular design (Radaelli et al. 2023).
Type B3: Short Quadrangular Taper Stems
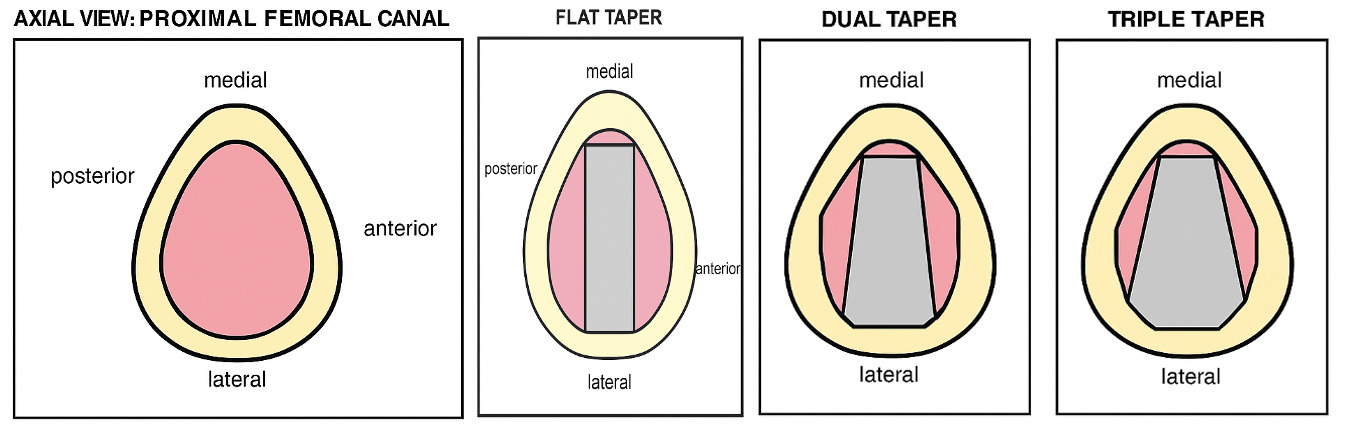
The advent of shorter femoral stem designs compatible with DA approach has driven substantial innovation in both implant geometry and broaching technique. These stems utilize a “round-the-corner” preparation method that follows the anatomic curvature of the medial calcar and is tailored to the specific level of femoral neck resection (Radaelli et al. 2023). From a geometric standpoint, these designs typically maintain a coronal silhouette similar to that of Type A and B2 stems while preserving a quadrangular cross-section that enhances sagittal plane engagement (Radaelli et al. 2023). Some stems incorporate a triple taper configuration to improve load distribution onto the calcar. To better conform to a range of femoral morphologies, these stems often exhibit reduced distal dimensions or a variable medial curvature (Radaelli et al. 2023).
Type C: Fit and Fill Stems
Fit and fill engaging stems come in two geometries: conical and cylindrical both of which have excellent track records in primary THA as well as in the treatment of periprosthetic femur fractures (PFF) (Radaelli et al. 2023). These stems completely fill the metaphyseal canal proximally and distally to achieve rotational stability (Figure 1) (Radaelli et al. 2023). They are typically designed for bone preparation with a ream-and-broach technique.
Type C1: Fit-and-Fill Stems
Type C1 fit-and-fill femoral stems are distinguished by a larger overall volume and unique metaphyseal geometry, typically exhibiting elliptical or trapezoidal cross-sections (Radaelli et al. 2023). In the coronal plane, these stems feature pronounced square shoulders, while the diaphyseal portion is either cylindrical or conical in shape (Radaelli et al. 2023). Compared to Type B stems, Type C1 designs aim to achieve a more comprehensive fill of the metaphyseal and proximal diaphyseal regions in both the coronal and sagittal dimensions, thereby enhancing initial mechanical stability (Radaelli et al. 2023). Canal preparation for these implants can involve a combination of reaming and broaching, although certain short-stem variants may be inserted using a broach-only technique.
Type C2: Anatomic Fit and Fill
These stems are designed to mimic the proximal femoral geometry to achieve maximum metaphyseal fill (Radaelli et al. 2023). As a result, they have a posterior metaphyseal bow lending to an anterior concavity when viewed laterally. These stems achieve initial fixation via metaphyseal fit and fill. Due to the unique sagittal geometry, bony preparation and stem insertion of anatomic stems can be more technically challenging (Radaelli et al. 2023).
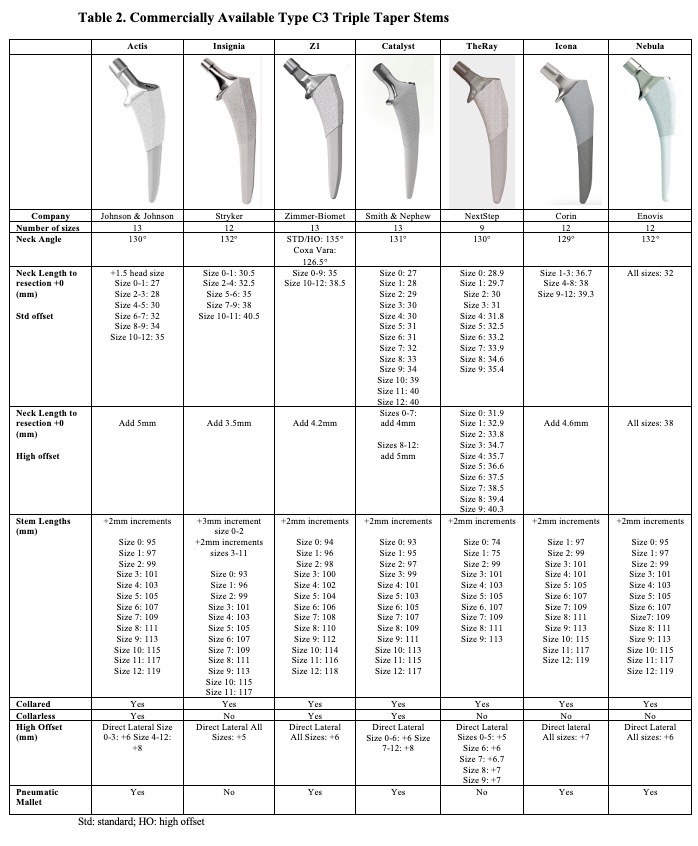
Type C3: Short Fit and Fill Triple Taper
Type C3 stems, similar to Type B3 stems, were developed to accommodate the technical demands of the DA approach and to mitigate issues related to proximal-distal mismatch (Radaelli et al. 2023). Unlike the more traditional Type C1 stems, C3 designs are a hybrid between traditional fit=fil; stems and blade-type stems and typically feature a shortened stem length and reduced distal profile, often eliminating the need for diaphyseal reaming during preparation. These stems do not fit-fill proximally to the extent that traditional fit-fill stems do, however, they do fill the metaphysis more than a blade type stem. Instead of the prominent square shoulders characteristic of C1 stems, C3 implants incorporate lateral relief at the level of the greater trochanter (Radaelli et al. 2023). This design enables preservation of trochanteric bone and facilitates implantation using a broach-only “round-the-corner” technique similar to B3 stems (Radaelli et al. 2023). Differentiating from Type B3 stems, C3 stems generally possess a trapezoidal design proximally and distally rather than quadrangular cross-section, which is intended to maximize metaphyseal engagement and enhance fit within the proximal femur in both coronal and sagittal planes (Table 2). Triple tapered femoral stems are the most commonly used stems in the United States for primary THA and continue to rise in prevalence according to the American Joint Replacement Registry (AJRR) (Carender et al. 2025). Axial views of the single, double and triple taper stems are summarized in Figure 2.
Type D: Conical
Conical stems, also known as tapered spline-cone stems, exhibit a circular cross-section that tapers distally in both the coronal and sagittal planes (Figure 1) (Radaelli et al. 2023; Kheir, Drayer, and Chen 2020). The conical design enables the stem to wedge into the medullary canal contributing to excellent axial and bending strength. They also exhibit longitudinal splines that contribute to rotational stability and provide a roughened surface for bony ongrowth. Bony preparation is typically carried out in ream-only fashion. Conical stems come in short and long varieties. Short conical stems were initially indicated for abnormal proximal femoral anatomy and have a steeper taper (typically 5) that enables axial stability over a short distance. Long conical stems are often utilized in the revision setting as they facilitate diaphyseal fixation irrespective of metaphyseal bone quality (Sassoon et al. 2024; Khanuja et al. 2011). In comparison to short conical stems, they typically have a gentler taper between 2.5 and 3 to minimize bone loss (McCrosson et al. 2023). They are available as either monoblock stems or with subtrochanteric modularity that allows surgeons to adjust stem height after diaphyseal fixation is achieved, select the appropriate offset and uncouple anteversion from the distal stem (McCrosson et al. 2023).
Type E: Cylindrical
Cylindrical stems also demonstrate circular cross-sections but do not taper distally leading to their cylinder shape (Figure 1). These stems are fully-coated and are designed to facilitate osseointegration over the entire length of the stem including the distal diaphysis. As these stems are primarily used in the revision setting or in cases of aberrant proximal femoral anatomy, it is not uncommon to see non-uniform osseointegration along a cylindrical stem. While this may theoretically lead to proximal stress shielding and bone loss, repeated clinical trials demonstrate excellent long-term survivability (MacDonald, Rosenzweig, Guerin, et al. 2010; Paprosky, Greidanus, and Antoniou 1999).
Type F: Calcar-Guided Ultra-Short, Neck-Preserving Stems
Calcar-guided ultra-short stems are designed to preserve proximal femoral bone and restore native hip biomechanics (Kutzner and Pfeil 2018). Though some resemble flat-wedge stems, they are smaller, retain more of the femoral neck, and feature an elliptical cross-section with a pronounced medial curve that conforms closely to the calcar (Figure 1) (Kutzner and Pfeil 2018). This design allows for individualized alignment and accurate restoration of femoral offset (Radaelli et al. 2023; Kutzner and Pfeil 2018). These stems follow a “round-the-corner” technique that tracks the medial calcar’s curvature, making stem position dependent on the femoral neck resection level (Kutzner and Pfeil 2018). Different hip morphologies yield distinct fixation patterns: coxa vara with a high neck cut results in varus alignment, increased offset, and metaphyseal 3-point fixation, while valgus hips with a low-cut leads to valgus positioning, reduced offset, and meta-diaphyseal fixation (Kutzner and Pfeil 2018). These stems often have a steeper learning curve.
Collared vs Collarless
Presence or absence of a calcar collar is another variable to consider when choosing a cementless femoral implant. While clinical results are varied, the benefits of calcar collars are multifactorial including increased bony stability, reduced risk of subsidence, improved rotational control, decreased risk of calcar fracture propagation, and decreased risk of PFF (Panichkul et al. 2019; Nerys-Figueroa et al. 2024). Opponents to calcar collars in cementless femoral fixation cite concerns that the collar may prevent complete implant seating, thus decreasing primary stability, or may not demonstrate rotational instability (Radaelli et al. 2023).
Stem Length
Femoral stems also vary in their overall femoral length. Femoral length can be measured in an absolute context (mm from tip to tip) but is more useful to consider when evaluated in relationship to a patient’s native anatomy. In their recent classification of cementless femoral stems, Radaelli et al. broke stem length into 5 separate categories: ultra-short, short, traditional, long, and ultra-long. Stem length category was determined by comparing the relative distance between the lesser trochanter and the distal tip of the implant (Radaelli et al. 2023). Ultra-short implants are defined as having less than one-third of the implant distal to the lesser trochanter (Radaelli et al. 2023). Short implants have one-third to one-half of the overall length distal to the lesser trochanter, and traditional implants one-half to three-quarters (Radaelli et al. 2023). Long implants have three-quarters of the implant distal to the lesser trochanter, and ultra-long implants extend distal to the isthmus (Radaelli et al. 2023).
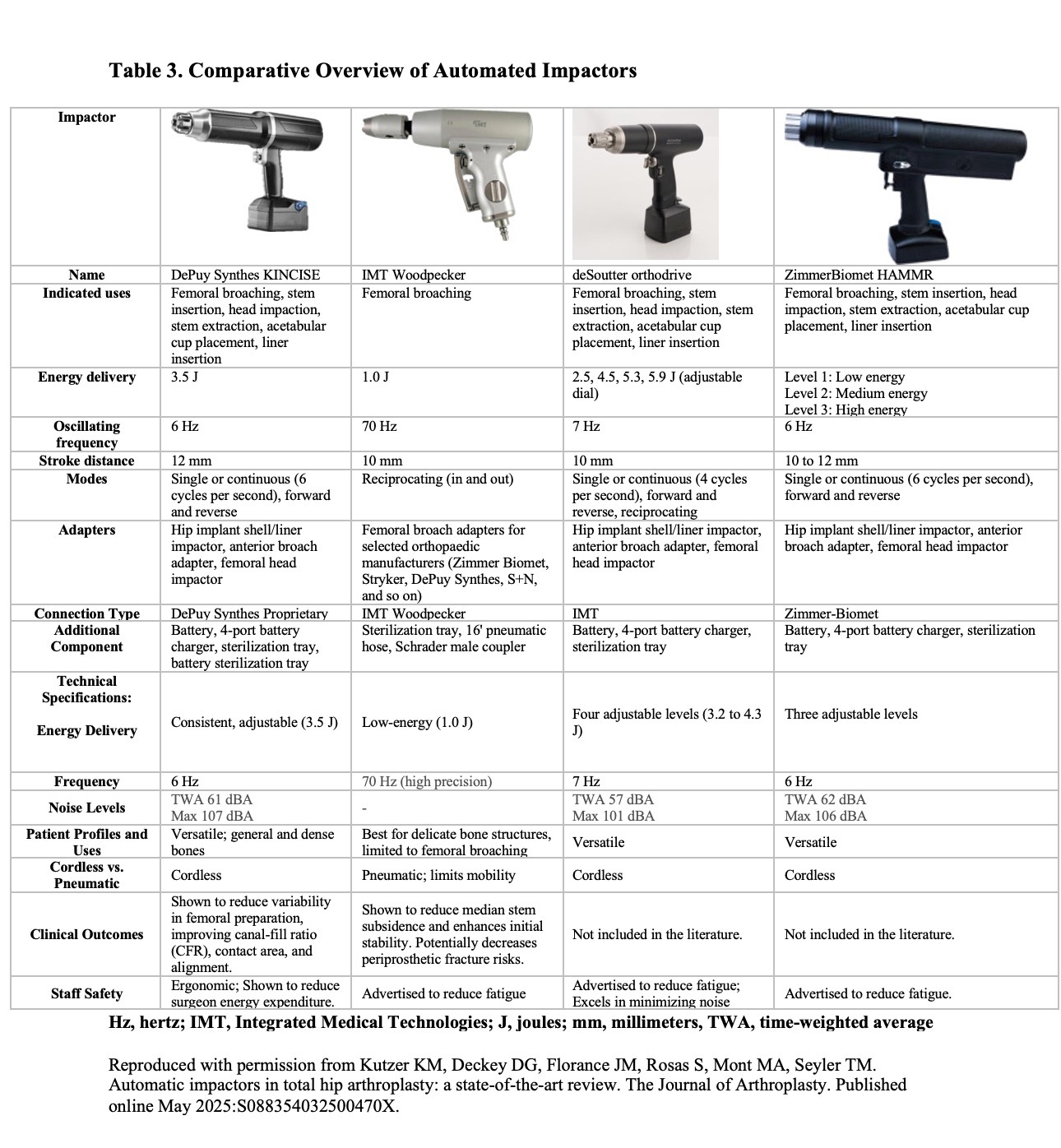
Automated Impaction
Conventional femoral stem preparation relies on manual impaction using handheld mallets. Although widely practiced, this technique presents several limitations, including variability in outcomes, risk of intraoperative femoral fractures, and significant physical strain on surgeons, particularly in high-volume practices. To address these concerns, automated impactors have been developed to deliver consistent and controlled impaction force, thereby enhancing procedural accuracy and reducing surgeon fatigue (Panichkul et al. 2019; Kutzer et al. 2025).
Early clinical data indicate that automated impaction systems may improve femoral component seating, increase canal fill ratios (CFRs), and reduce operative time (Kutzer et al. 2025). Moreover, when used with contemporary implants, such as Type C3 stems via the DA approach, these devices may help lower the incidence of femoral and acetabular fractures (Kutzer et al. 2025). Despite their growing use, automated impactor systems differ in design, functionality, and clinical utility. The most common commercially available devices for femoral canal preparation are summarized in Table 3 (Kutzer et al. 2025). Recent studies have suggested automated impaction has consistent advantages in stem preparation consistency and risk reduction compared to manual broaching as summarized in Table 4. (Kutzer et al. 2025)
Global Trends in Stem Type Utilization
American Joint Replacement Registry (AJRR)
The AJRR 2024 Annual Report (N=943,690) identified that the utilization of modern Type C3 triple taper stems continue to rise (Carender et al. 2025). Type C3 stems were used in 7% of primary THA in 2018 with exponential growth to nearly 30% by 2023 while the other stem designs has progressively declined over the last 5 years (Carender et al. 2025).
National Joint Registry (NJR)
The NJR which collects THA data from England, Wales, Northern Ireland, the Isle of Man and the States of Guernsey has shown steady utilization of Type B2 stems (nearly 50%) from 2014 to 2022 (“National Joint Registry - Annual Report 2024 - The National Joint Registry,” n.d.). During that same time period, Type A stems usage increased from nearly 1% in 2014 to nearly 20% by 2022 (“National Joint Registry - Annual Report 2024 - The National Joint Registry,” n.d.).
Swedish Arthroplasty Registry (SAR)
Similar to the NJR, the SAR reports steady utilization of Type B2 stems (51%) from 2009 to 2023. Type A and B1 stems represent a smaller minority of utilization (<5%) as cemented stems are most commonly reported (Kärrholm, Rogmark, Nauclér, et al., n.d.).
Australian Orthopedic Association National Joint Replacement Registry (AOANRR)
In 2020, AOANJRR reported type B2 stems comprising of nearly 38% of primary cementless THA with type A stems as the second most commonly utilized type design (29%) (“Australian Orthopaedic Association National Joint Replacement Registry,” n.d.). However, over from 2021-2023, the utilization of type A stems has continued to rise (41%, 46%, 51%, respectively) (“Australian Orthopaedic Association National Joint Replacement Registry,” n.d.). In 2023, modern type C3 stems were implanted for the first time which represented 4% of all cementless stems used (“Australian Orthopaedic Association National Joint Replacement Registry,” n.d.).
New Zealand Joint Registry (NZJR)
In 2024, NZJR reported that over the prior 10 years, the utilization of fully cemented THA declined significantly, cementless stems remained relatively stable and hybrid THA more than doubled (“Annual Reports | New Zealand Orthopaedic Association,” n.d.). Type B2 stems are the most used cementless femoral stems (60%), followed by Type A (23%) and C1 (7%) (“Annual Reports | New Zealand Orthopaedic Association,” n.d.). Type C3 stems usage has not been reported.
Clinical Outcomes
Although cementless femoral stems overall have shown to provide a safe and efficacious option for primary THA, different stem designs have variable outcomes (Rocha, Somerville, Moody, et al. 2025). Type A single wedge designs have been reported to have a higher risk of aseptic loosening relative to type B double wedge designs (Reddy et al. 2023). However, Jeong et al (Jeong et al. 2023). reported the incidence of PFF to be significantly higher in type B1 stems compared to type A and type B2 stems. More surgical treatments (1.7 versus 0.5 versus 0.7%; p=0.013) and femoral revisions (1.2 versus 0.2 versus 0%; p=0.004) were required for PFF in type B1 stems (Jeong et al. 2023). Over a prospective period of 36 months, Berdini et al (Berdini et al. 2024). compared 44 patients with B1 femoral stems and 40 patients with C2 anatomic stems and found that although there was no statistical relevance, patients with C2 stems has lower incidence of anterior thigh pain and higher degree of motion in external rotation between 6 and 12 months. Additionally, type B1 stems had greater incidence of iatrogenic fractures, dislocation, infection and heterotopic ossification (Berdini et al. 2024).
Finger et al. (Finger, Gong, Mirvish, et al. 2025) reported overall revision rates based on stem design from 2021 joint registry data collected from the AJRR, NJR, AOANJR, and NZJR. In total, the most utilized stem types were type B2 stems (429,752 cases), type A stems (247,198), and type C1 stems (101,954 cases) (Finger, Gong, Mirvish, et al. 2025). The aggregated registry data found an overall all cause revision rate amongst all stem designs to be 4.19% (Finger, Gong, Mirvish, et al. 2025). Among the grouped stem categories, the highest revision rates were found in type B1 stems (8.09%, 1,680 revisions out of 20,776 cases), type B2 stems (4.97%, 21,339 of 429,595 cases), and type C1 stems (4.66%, 4,742 of 101,849 cases) (Finger, Gong, Mirvish, et al. 2025). In contrast, the lowest revision rates were recorded for type C3 stems (1.12%, 172 of 15,299 cases), type E stems (1.35%, 101 of 7,506 cases), and type B3 stems (2.55%, 48 of 1,880 cases) (Finger, Gong, Mirvish, et al. 2025). Compared with other stem designs, type C3 stems are relatively newer with fewer implants currently available on the market without long term data (Table 2). However, recent short term data has shown type C3 stems to have low rates of complications, including subsidence, loosening and PFF, especially in elderly patients (>70 years old) (Grayson et al. 2025).
Summary
Femoral stem designs in cementless THA have continued to evolve presenting orthopaedic surgeons with a wide variety of stem designs to choose from. Regardless of specific design, cementless femoral stems are widely successful with excellent long-term survivability. Nevertheless, surgeons should evaluate each patient on an individual basis to determine the appropriate femoral stem for their unique anatomy, bone quality, and activity level to optimize patient outcomes.

_and_mediolateral_(ml)_plan.jpeg)


_and_mediolateral_(ml)_plan.jpeg)